Developmental and Behavioral Pediatrics 4: ADHD
Session: Developmental and Behavioral Pediatrics 4: ADHD
792 - Risks of ADHD from Prenatal Opioid Exposure Differ Between Infants With and Without Maternal ADHD
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 792.6346
Andy Shen, UC Berkeley, Berkeley, CA, United States; Samuel D. Pimentel, University of California Berkeley, Berkeley, CA, United States; MICHAEL W. KUZNIEWICZ, Kaiser Permanante, Los Gatos, CA, United States; Sherian X. Li, Kaiser Permanente Division of Research, Pleasanton, CA, United States; Cynthia Salorio, Johns Hopkins University School of Medicine, Baltimore, MD, United States; Cynthia Campbell, Kaiser Permanente Northern California Division of Research, Pleasanton, CA, United States; Sandra D. Comer, Columbia University Vagelos College of Physicians and Surgeons, New York, NY, United States; Monique M. Hedderson, Kaiser Permanente Northern California, Division of Research, Pleasanton, CA, United States; Dana Edelman, Kaiser Permanente Division of Research, Pleasanton, CA, United States; Jennifer L. Ames, Kaiser Foundation Research Institute, Pleasanton, CA, United States; Lena S. Sun, Columbia University Vagelos College of Physicians and Surgeons, New York, NY, United States

Samuel D. Pimentel, PhD (he/him/his)
Assistant Professor of Statistics
University of California Berkeley
Berkeley, California, United States
Presenting Author(s)
Background: Prenatal opioid exposure (POE) is associated with increased risk of ADHD. ADHD is partially heritable and has been linked with maternal (Mat) ADHD. However, it is unknown whether the impact of POE on ADHD may vary with Mat ADHD.
Objective: To examine ADHD risks associated with POE, with and without maternal (Mat) diagnoses (Dx) of ADHD and depression.
Design/Methods: In a 2010-2023 birth cohort from an integrated healthcare system, POE was identified using pharmacy records, urine drug screens, and chart review among infants scored for abstinence for at least two days. ADHD was defined as having an ICD-9/ICD-10 ADHD Dx and ADHD medication dispensed twice. Mat clinical and demographic baseline variables were extracted from electronic health records and linked census data, including indicators for Mat ADHD and Mat depression.
Each case with POE was matched with 5 unexposed controls using cardinality matching. Unexposed (Unexp) matched samples were chosen for: entire POE group, POE group with Mat ADHD, POE group without Mat ADHD and for subgroups defined by Mat depression (Figure 1). We report risk differences and hazard ratios (HR) fit with stratified Cox proportional hazards models. Significance was assessed using permutation tests.
Results: 2,475 POE and 536,536 Unexp subjects were identified. In the full cohort 3.1% of subjects had Mat ADHD, 24% had Mat depression, and 1.1% had ADHD. ADHD rates were elevated among subjects with Mat ADHD (4.3% with vs. 1% without, p < 0.001) or with Mat depression (2.2% with vs. 0.7% without, p < 0.001). Matching balanced all baseline variable means within 0.002 standard deviations across all matches (Table 1). The ADHD risk difference in the overall matched POE vs. unexposed comparison was 2.5% vs. 2.2% (p=0.23) with HR=1.3 (p=0.19). In the matches for subjects with and without Mat ADHD, we observed risk difference 4.1% vs 5.8% (p=0.18) and HR=0.72 (p=0.36), and risk difference 2.3% vs 1.9% (p = 0.17) and HR= 1.84 (p=0.004), respectively. In contrast, for groups with and without Mat depression, we observed risk difference 3.1% vs 3.2% (p=0.75) and HR=1.17 (p=0.41), and risk difference 1.5% vs 1.2% (p=0.4) and HR=1.47 (p=0.36), respectively (Table 2).
Conclusion(s): While there was no significant effect of POE on ADHD overall or for those with Mat ADHD, a significant POE effect was found in infants without Mat ADHD. No such effect appears for maternal depression. Thus, Mat ADHD may have a specific effect on the risks of ADHD from POE.
Figure 1: Overview of matched comparisons conducted.
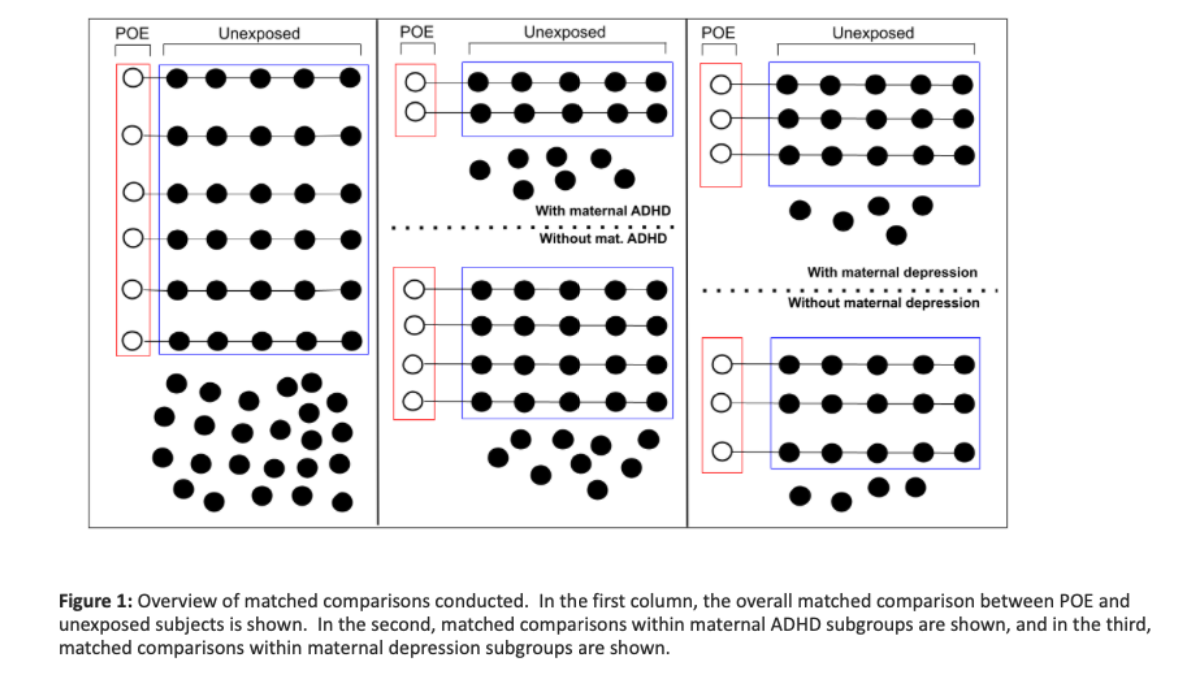 In the first column, the overall matched comparison between POE and unexposed subjects is shown. In the second, matched comparisons within maternal ADHD subgroups are shown, and in the third, matched comparisons within maternal depression subgroups are shown.
In the first column, the overall matched comparison between POE and unexposed subjects is shown. In the second, matched comparisons within maternal ADHD subgroups are shown, and in the third, matched comparisons within maternal depression subgroups are shown. Table 1: Balance on selected variables before and after matching, stratified by maternal ADHD diagnosis.
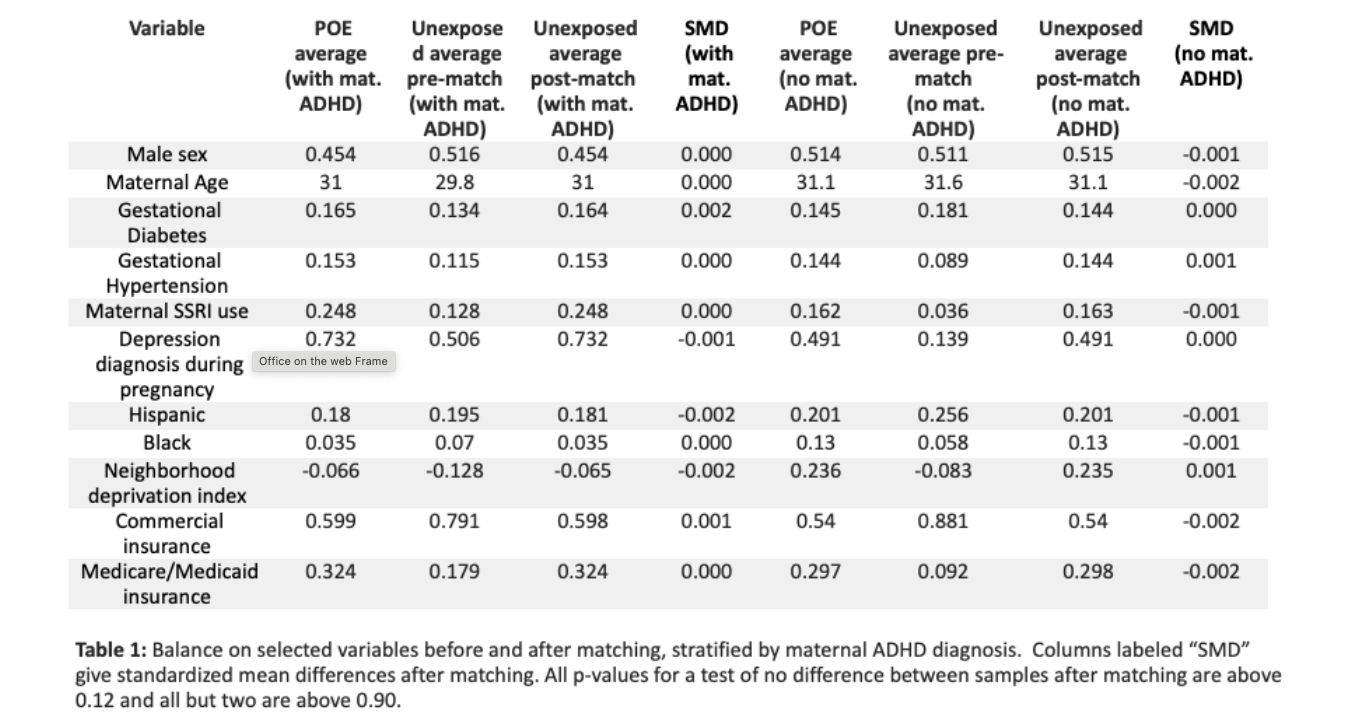 Columns labeled “SMD” give standardized mean differences after matching. All p-values for a test of no difference between samples after matching are above 0.12 and all but two are above 0.90.
Columns labeled “SMD” give standardized mean differences after matching. All p-values for a test of no difference between samples after matching are above 0.12 and all but two are above 0.90. Table 2: POE vs unexposed control outcome comparison.
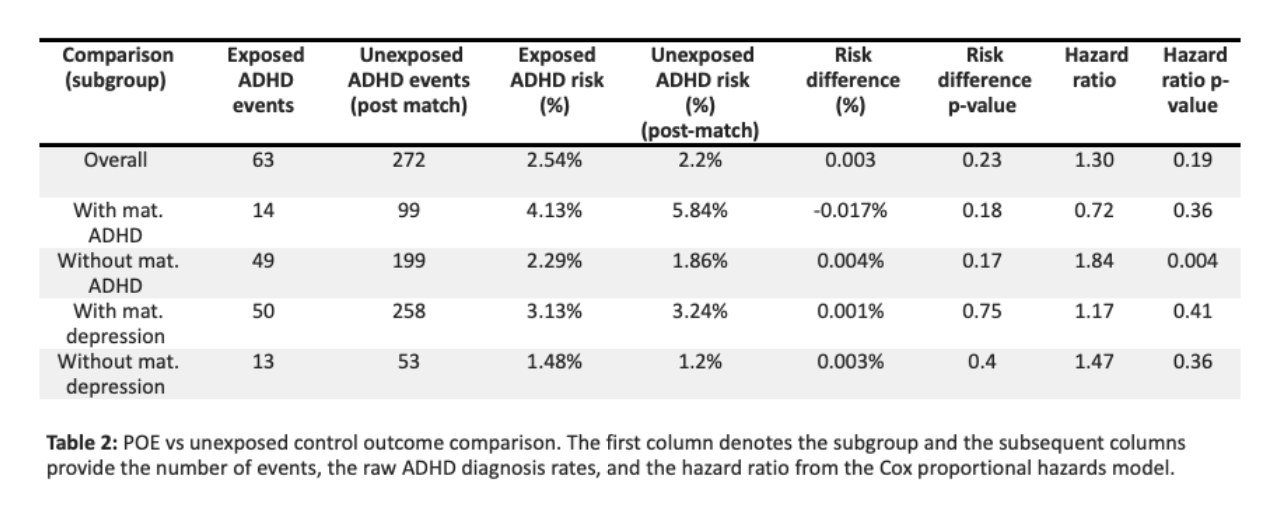 The first column denotes the subgroup and the subsequent columns provide the number of events, the raw ADHD diagnosis rates, and the hazard ratio from the Cox proportional hazards model.
The first column denotes the subgroup and the subsequent columns provide the number of events, the raw ADHD diagnosis rates, and the hazard ratio from the Cox proportional hazards model. 
