Neonatal Fetal Nutrition & Metabolism 2
Session: Neonatal Fetal Nutrition & Metabolism 2
617 - Vitamin D deficiency and its association with preterm birth from January 2016 to March 2024: Eight years of effect.
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 617.7029
Anjali Borsum, Medical University of South Carolina College of Medicine, Charleston, SC, United States; Maya Andrade, Medical University of South Carolina College of Medicine, Charleston, SC, United States; Kilee W. Knight, Medical University of South Carolina College of Medicine, Mount Pleasant, SC, United States; myla Ebeling, Medical University of South Carolina College of Medicine, Charleston, SC, United States; Carol L. Wagner, Medical University of South Carolina College of Medicine, Charleston, SC, United States

Anjali Borsum, BS (she/her/hers)
Medical Student
Medical University of South Carolina College of Medicine
Charleston, South Carolina, United States
Presenting Author(s)
Background: Maternal vitamin D (vitD; 25(OH)D) status plays a role in skeletal developmental and calcium homeostasis and has been shown to influence maternal and fetal health outcomes. Optimal 25(OH)D during pregnancy is ~40 ng/mL, where conversion to 1,25(OH)2D is directly linked (Wagner & Hollis, 2020). Debate about the specific benefits of 25(OH)D supplementation in pregnancy is ongoing and recommendations for supplementation and monitoring vary among providers. While adequate 25(OH)D levels are linked with better birth outcomes, causal relationship between maternal 25(OH)D and preterm birth remains unclear.
Objective: To investigate the association between maternal 25(OH)D status and gestational age at delivery.
Design/Methods: We conducted a retrospective chart review of 15,506 women who had 25-hydroxyvitamin D [25(OH)D] concentrations measured during pregnancy and delivered from January 2016 to March 2024 via electronic medical records (Epic). Women with cancer, HIV, or participation in vitD supplementation trials were excluded. 25(OH)D concentrations were compared to the gestational age at delivery.
Results: Of the mothers, 29.3% were Black American, 8.9% were Hispanic, and 50.7% were White. The overall mean ± SD 25(OH)D concentration was 34.2±17 ng/mL. Mothers delivering < 37 wks had significantly lower 25(OH)D (30.4±17.4 ng/mL) compared to those delivering at ≥37 wks (34.8±17.3 ng/mL), with a mean difference of -4.4 ng/mL (95% CI: -5.23 to -3.62, p< 0.0001). This difference was accentuated among mothers delivering < 32 weeks (26.3±14.9 ng/mL) compared to those delivering at ≥32 wks (34.4±17.4 ng/mL), with a mean difference of 8.2 ng/mL (95% CI: 6.43 to 9.94, p< 0.0001). Of the 687 moms with 25(OH)D < 10 ng/mL,v151 (22.0%) delivered at < 37 wks, and compared to the 14,801 moms with 25(OH)D >10 ng/mL, only 1,886 (12.7%) delivered at < 37 wks (p < 0.0001).The relative risk of delivering < 37 wks is 1.43 (95% CI: 1.30 to 1.56, p< 0.001) for mothers with 25(OH)D >40 ng/mL compared to those below. These findings were consistent across racial/ethnic groups.
Conclusion(s): Mothers delivering < 37 wks had significantly lower 25(OH)D concentrations compared to those delivering ≥37 wks, and the difference was greater for women delivering 32 wks compared to those delivering at ≥32 wks. The risk of delivering < 37 wks increases as 25(OH)D concentrations decrease. While further research should be conducted to determine a causal relationship between vitD status and preterm birth, this study suggests 25(OH)D screening and supplementation could be a cost-effective strategy in lowering the incidence of preterm birth.
Table 1. Mean 25(OH)D per Gestational Age and Mean Difference.
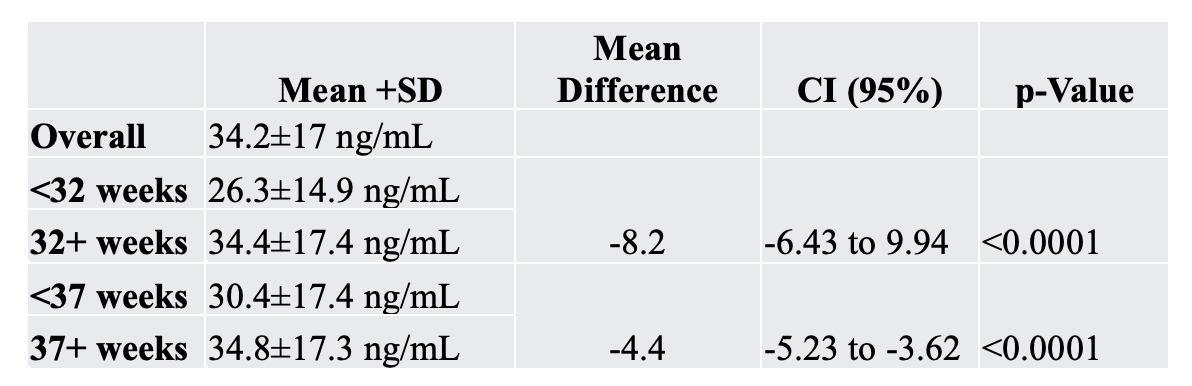 The overall mean ± SD 25(OH)D concentration was 34.2±17 ng/mL. Mothers delivering <37 weeks had significantly lower 25(OH)D (30.4±17.4 ng/mL) compared to those delivering at ≥37 wks (34.8±17.3 ng/mL), with a mean difference of -4.4 ng/mL (95% CI: -5.23 to -3.62, p<0.0001). This difference was accentuated among mothers delivering < 32 weeks (26.3±14.9 ng/mL) compared to those delivering at ≥32 weeks (34.4±17.4 ng/mL), with a mean difference of 8.2 ng/mL (95% CI: 6.43 to 9.94, p<0.0001).
The overall mean ± SD 25(OH)D concentration was 34.2±17 ng/mL. Mothers delivering <37 weeks had significantly lower 25(OH)D (30.4±17.4 ng/mL) compared to those delivering at ≥37 wks (34.8±17.3 ng/mL), with a mean difference of -4.4 ng/mL (95% CI: -5.23 to -3.62, p<0.0001). This difference was accentuated among mothers delivering < 32 weeks (26.3±14.9 ng/mL) compared to those delivering at ≥32 weeks (34.4±17.4 ng/mL), with a mean difference of 8.2 ng/mL (95% CI: 6.43 to 9.94, p<0.0001). Figure 1. Mean 25(OH)D Concentration and Gestational Age at Delivery.
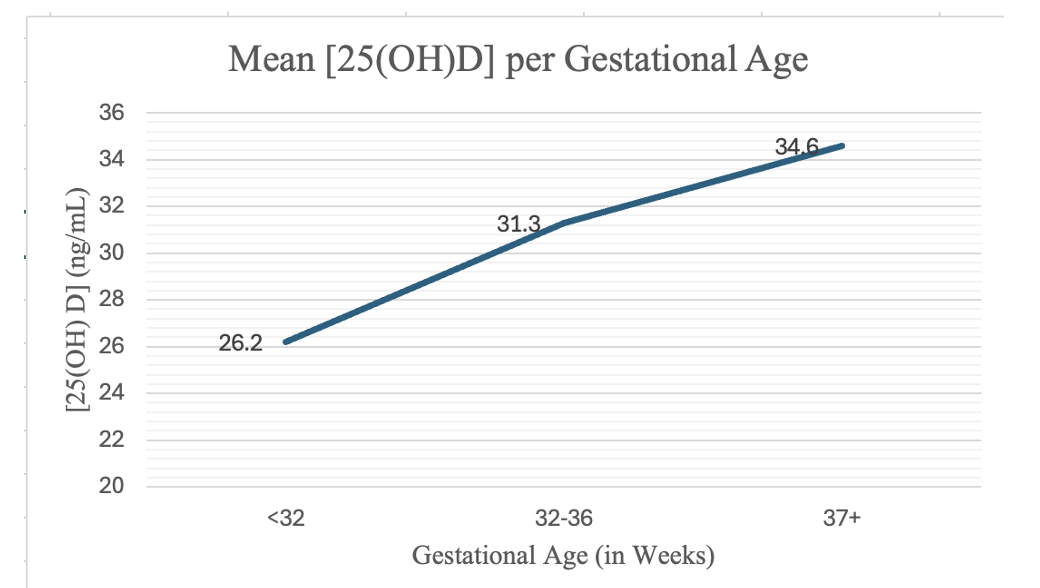 Mothers delivering <37 weeks had significantly lower 25(OH)D concentrations compared to those delivering ≥37 weeks, and the difference was greater for women delivering <32 weeks compared to those delivering at ≥32 weeks.
Mothers delivering <37 weeks had significantly lower 25(OH)D concentrations compared to those delivering ≥37 weeks, and the difference was greater for women delivering <32 weeks compared to those delivering at ≥32 weeks. Table 2. Relative Risk of Delivering Preterm Compared to 25(OH)D Levels.
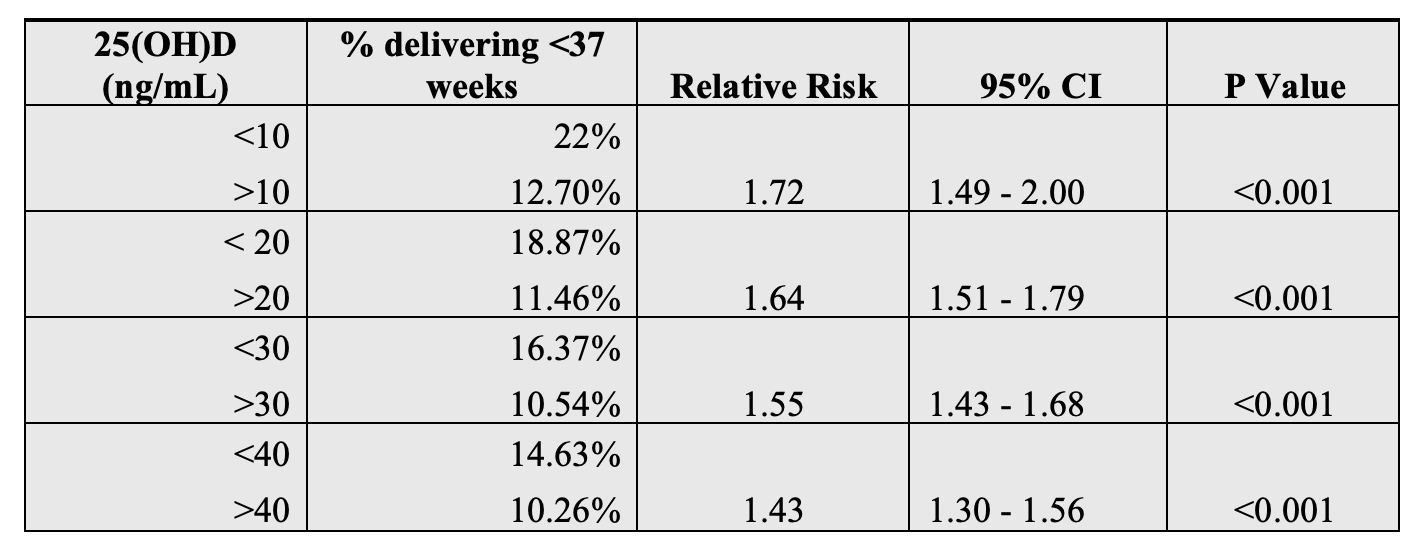 As 25(OH)D levels decrease, the risk of preterm delivery increases. Mothers with severe vitD deficiency ( <10 ng/mL) are 1.72 times more likely to deliver preterm than mothers with 25(OH)D higher than 10 ng/mL.
As 25(OH)D levels decrease, the risk of preterm delivery increases. Mothers with severe vitD deficiency ( <10 ng/mL) are 1.72 times more likely to deliver preterm than mothers with 25(OH)D higher than 10 ng/mL. Table 1. Mean 25(OH)D per Gestational Age and Mean Difference.
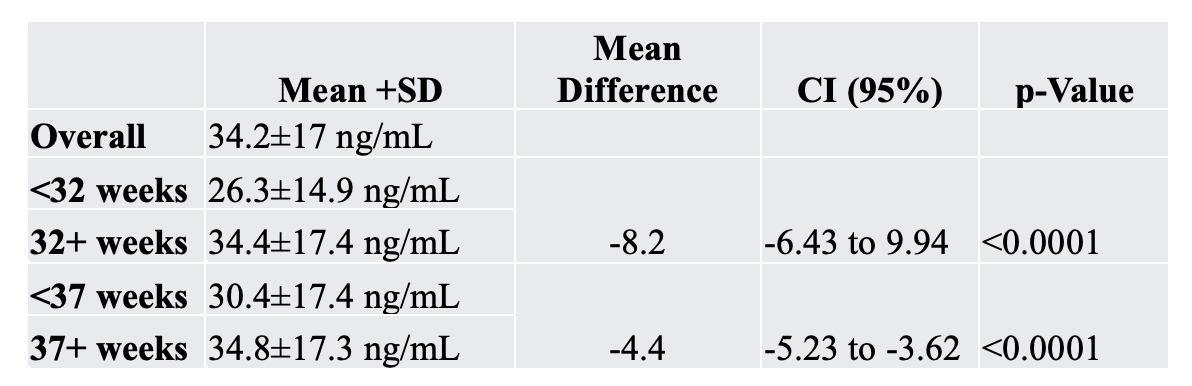 The overall mean ± SD 25(OH)D concentration was 34.2±17 ng/mL. Mothers delivering <37 weeks had significantly lower 25(OH)D (30.4±17.4 ng/mL) compared to those delivering at ≥37 wks (34.8±17.3 ng/mL), with a mean difference of -4.4 ng/mL (95% CI: -5.23 to -3.62, p<0.0001). This difference was accentuated among mothers delivering < 32 weeks (26.3±14.9 ng/mL) compared to those delivering at ≥32 weeks (34.4±17.4 ng/mL), with a mean difference of 8.2 ng/mL (95% CI: 6.43 to 9.94, p<0.0001).
The overall mean ± SD 25(OH)D concentration was 34.2±17 ng/mL. Mothers delivering <37 weeks had significantly lower 25(OH)D (30.4±17.4 ng/mL) compared to those delivering at ≥37 wks (34.8±17.3 ng/mL), with a mean difference of -4.4 ng/mL (95% CI: -5.23 to -3.62, p<0.0001). This difference was accentuated among mothers delivering < 32 weeks (26.3±14.9 ng/mL) compared to those delivering at ≥32 weeks (34.4±17.4 ng/mL), with a mean difference of 8.2 ng/mL (95% CI: 6.43 to 9.94, p<0.0001). Figure 1. Mean 25(OH)D Concentration and Gestational Age at Delivery.
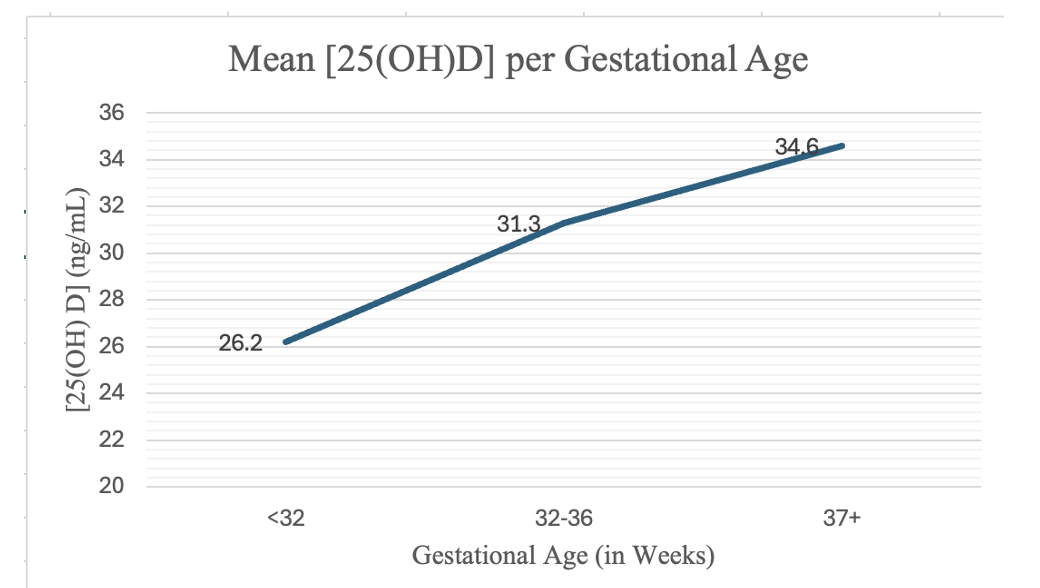 Mothers delivering <37 weeks had significantly lower 25(OH)D concentrations compared to those delivering ≥37 weeks, and the difference was greater for women delivering <32 weeks compared to those delivering at ≥32 weeks.
Mothers delivering <37 weeks had significantly lower 25(OH)D concentrations compared to those delivering ≥37 weeks, and the difference was greater for women delivering <32 weeks compared to those delivering at ≥32 weeks. Table 2. Relative Risk of Delivering Preterm Compared to 25(OH)D Levels.
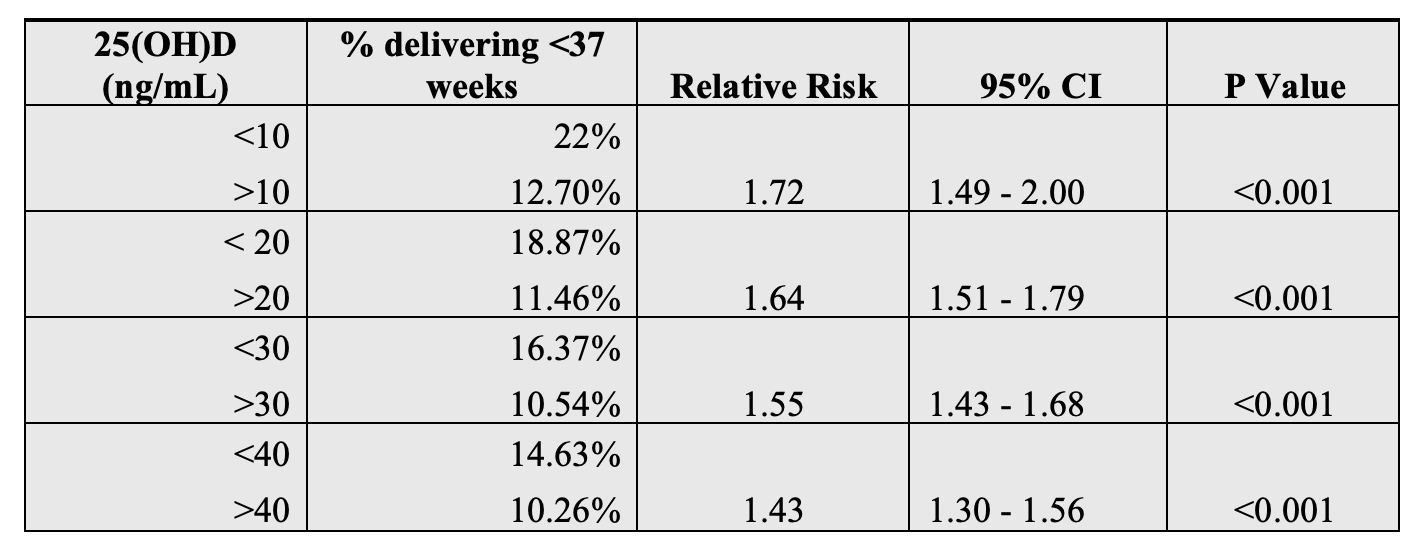 As 25(OH)D levels decrease, the risk of preterm delivery increases. Mothers with severe vitD deficiency ( <10 ng/mL) are 1.72 times more likely to deliver preterm than mothers with 25(OH)D higher than 10 ng/mL.
As 25(OH)D levels decrease, the risk of preterm delivery increases. Mothers with severe vitD deficiency ( <10 ng/mL) are 1.72 times more likely to deliver preterm than mothers with 25(OH)D higher than 10 ng/mL. 
