Quality Improvement/Patient Safety 6
Session: Quality Improvement/Patient Safety 6
496 - VPS Nutrition Collaborative Quality Improvement Project
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 496.7074
Theresa Mikhailov, Medical College of Wisconsin, Milwaukee, WI, United States; Lece Webb, University of Alabama School of Medicine, Birmingham, AL, United States; Gerardo Soto-Campos, VPS, LLC, Los Angeles, CA, United States; Corcoran Downey, Miller Children's & Women's Hospital Long Beach, Long Beach, CA, United States; Sarah Kustra, Miller Children's & Women's Hospital Long Beach, Orange, CA, United States; Brittany M. Critcher, Miller Children's & Women's Hospital Long Beach, Fleetwood, NC, United States; Christopher J.. Babbitt, MemorialCare, Long Beach, CA, United States; Nicole Fabus, Children's Hospital of Wisconsin, Milwaukee, WI, United States; Martin K. Wakeham, Medical College of Wisconsin/Children's Wisconsin, Milwaukke, WI, United States; Mudit Mathur, Kaiser Permanente Bernard J. Tyson School of Medicine, Fontana, CA, United States; Danielle L. Destefano, Kaiser Permanente Pediatric Care Center, Riverside, CA, United States; Mellissa Mahabee, Dayton Children's Hospital, Dayton, OH, United States; Maddie Van Dorpe, Dayton Children's Hospital - - Dayton, OH, Dayton, OH, United States; Alyssa Price, Dayton Children's Hospital, Cincinnati, OH, United States; Kristin Mikolajewski, Dayton Children's Hospital, Piqua, OH, United States; Aphton Lane, Uniformed Services University of the Health Sciences F. Edward Hebert School of Medicine, San Antonio, TX, United States; Leigh B. Hardy, Children's Hospital of Alabama, Birmingham, AL, United States; Janah Stewart, Registry Partners, Hanover, VA, United States; Marquita Gregory, Children's Hospital, Birmingham, AL, United States; Daniel Garros, University of Alberta Faculty of Medicine and Dentistry, Edmonton, AB, Canada; Lydia Fong, Alberta Health Service, Edmonton, AB, Canada; Christine L. MacDonald, Stollery Children Hospital, Edmonton, AB, Canada; Cheryl Hulbert, Virtual Pediatric Systems, LLC, Saint Helena Island, SC, United States; Nancy K. Brundage, Virtual Pediatric Systems, (VPS, LLC), Kansas City, MO, United States; Ramesh Sachdeva, Children's Hospital of Michigan, Detroit, MI, United States; Thomas B. Rice, Medical College of WI, Arena, WI, United States
- LW
Lece Webb, MD
Assistant Professor
University of Alabama School of Medicine
Birmingham, Alabama, United States
Presenting Author(s)
Background: Malnutrition has been linked to increased morbidity and mortality in hospitalized patients, leading to higher health care costs. The VPS (Virtual Pediatric Systems, LLC) Nutrition Module includes data for three pediatric nutrition metrics (nutrition screening, nutrition assessment, and caloric goal documentation) developed by the Pediatric Measurement Center of Excellence, an AHRQ initiative. VPS brought together five interested PICU teams in Phase 1 beginning January 2023 to form a Nutrition Collaborative (NC) with the goal of improving the nutrition care of the critically ill children under our care. A sixth PICU team joined the NC in Phase 2 beginning January 2024.
Objective: To improve the proportion of PICU patients with a nutrition screen documented within 24 hours of admission from the baseline (64.6%) to a goal of 80%.
Design/Methods: Each team consisted of a physician, a nursing leader, and a dietitian. The NC met virtually each month to review data, share knowledge, and discuss opportunities to improve nutrition care. VPS aggregated data monthly for each nutrition metric and for each anthropometric measure for each participating unit. VPS tracked monthly unit aggregate points via control charts. The NC identified opportunities in three areas and developed interventions to improve the proportion of patients with a nutrition screen documented within 24 hours of PICU admission: 1) standardized education on the impact of malnutrition on outcomes in critically ill children, 2) review of screening process to identify and implement improvement changes, 3) rescreening of patients admitted to the PICU from other inpatient units. Each site chose which interventions to adopt and at what time through PDSA cycles. VPS provided analysis of deidentified aggregate data, identified rule violations, and calculated changes in center lines following Nelson’s rules.
Results: The 6 VPS NC sites from the US and Canada systematically reviewed and shared successful improvement methods and implemented individualized interventions based on site-specific data. These interventions were associated with an increase in the proportion of PICU patients with a documented nutrition screen within 24 hours of admission from 64.6% in January 2024 to 73.8% by September of 2024 for Phase 1 and from 50.7% to 68.7% for Phase 2.
Conclusion(s): Data driven collaboration between PICU teams while implementing site-specific interventions can impact successful nutrition screening at admission, enhance documentation, and improve the nutrition care of critically ill children. The Phase 2 unit may have benefited from joining Phase 1 in progress.
Phase 1 Control Chart for the Percent of Completed Screens for Five Original Units.
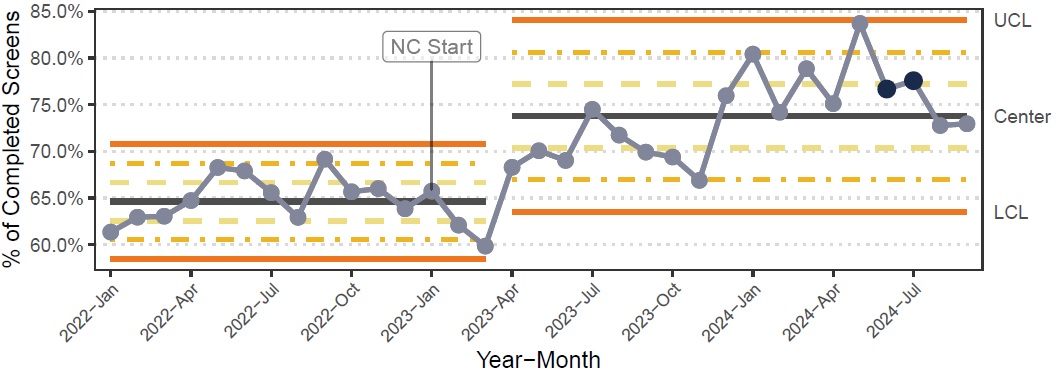 The annotation “NC Starts” at January 2024 shows the beginning of the nutrition collaborative for the five original units. The baseline comprises the period January 2022 to March 2023. Centerline (CL) changes were implemented through Nelson’s rule (Reynolds et al, 2021) when nine or more points fall above/below a CL.
The annotation “NC Starts” at January 2024 shows the beginning of the nutrition collaborative for the five original units. The baseline comprises the period January 2022 to March 2023. Centerline (CL) changes were implemented through Nelson’s rule (Reynolds et al, 2021) when nine or more points fall above/below a CL.Phase 2 Control Chart for Percent of Completed Screens for the Sixth Unit.
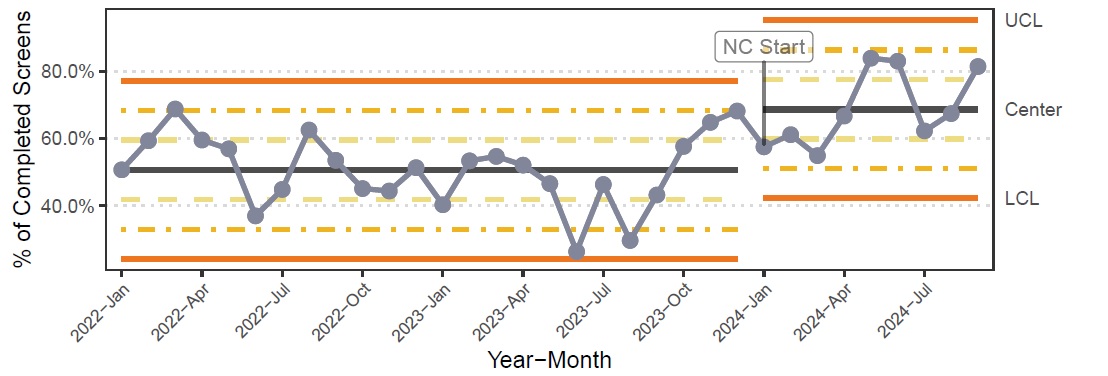 While the sixth unit started nutrition data collection as early as January 2022, its inclusion into the collaborative started on January 2024. This has been captured in the plot with the annotation “NC Starts”. Centerline changes were implemented though Nelson’s rules (Reynolds et al, 2021).
While the sixth unit started nutrition data collection as early as January 2022, its inclusion into the collaborative started on January 2024. This has been captured in the plot with the annotation “NC Starts”. Centerline changes were implemented though Nelson’s rules (Reynolds et al, 2021).

