Developmental and Behavioral Pediatrics 3: Autism 1
Session: Developmental and Behavioral Pediatrics 3: Autism 1
789 - Evaluating an Educational Training Program for Pediatric Primary Care Clinicians to Diagnose Autism
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 789.4665
Carol Weitzman, Harvard Medical School, Woodbridge, CT, United States; Julie Bickel, Boston Children's Hospital, Ashland, MA, United States; Jonathan Hatoun, Pediatric Physicians' Organization at Children's, Wellesley, MA, United States; Ashley Coop, Boston Children’s Hospital, Andover, MA, United States; Laura B. Patane, Boston Childrens' Hospital, Cambridge, MA, United States; Margaret W. Fry, Pediatric Physicians' Organization at Children's, Wellesley, MA, United States

Carol Weitzman, MD (she/her/hers)
Co-Director Autism Spectrum Center
Harvard Medical School
Woodbridge, Connecticut, United States
Presenting Author(s)
Background: Autism Spectrum Disorder (ASD) affects 2.8% of children. Wait times for an evaluation are lengthy, often delaying access to treatments requiring an ASD diagnosis. The AAP has stated that a pediatric primary care clinician (PPCC) can diagnose ASD, but little is known about the optimal length and type of training needed.
Objective: To evaluate a novel, 8-session educational training program for PPCCs to diagnose children ≤ 36 months of age at high risk for an ASD diagnosis due to a failed ASD screen or clinician concern.
Design/Methods: PPCCs (physicians, nurse practitioners, physician assistants) were invited from a network of 80 pediatric primary care practices with approximately 600 PPCCs. Two cohorts of PPCCs were enrolled in an 8-session, 12-hour, training program conducted over 9 months (Table 1), in which they learned to complete the Brief Autism Structured Observation In Children (BASIC) and use their observations to score the Childhood Autism Rating Scale-Second Edition Standard Version (CARS-2ST). PPCCs were surveyed at baseline and 3-months after training completion. The survey included 16 statements with a 5-point Likert scale ranging from strongly disagree (1) to strongly agree (5). Information was collected about demographics, practice characteristics, practice patterns, and attitudes, confidence, and knowledge regarding ASD.
Results: A total of 36 PPCCs from 24 practices enrolled in the training and 29 (81%, N=26 physicians, 2 nurse practitioners, 1 physician assistant) completed pre- and post-surveys. Provider demographics and practice characteristics are shown in Table 2. Ninety percent of PPCCs had no prior training in diagnosing ASD. After completing the training program, PPCCs reported significant increases in their mean Likert scale scores from baseline to post-assessment for knowledge about ASD (3.59 vs. 4.38, p< 0.001), their competence in taking an ASD history (2.48 vs. 4.28, p< 0.001), completing the BASIC (2.17 vs. 3.90, p< 0.001), and scoring the CARS2-ST (1.83 vs. 4.00, p< 0.001). PPCCs also reported significantly greater comfort in making a diagnosis of ASD in children ≤ 36 months of age with mild ASD (2.31 vs. 3.02, p< 0.001), moderate ASD (3.03 vs. 3.83, p< 0.001), and severe ASD (3.45 vs. 4.34, p< 0.001).
Conclusion(s): After an 8-session educational training to learn to diagnose young children ≤ 36 months of age at high risk for ASD, PPCCs reported significant increases in their knowledge of ASD, as well as their competence and confidence evaluating and diagnosing children. PPCCs can potentially extend the workforce and reduce delays for children with ASD to obtain services.
Table 1
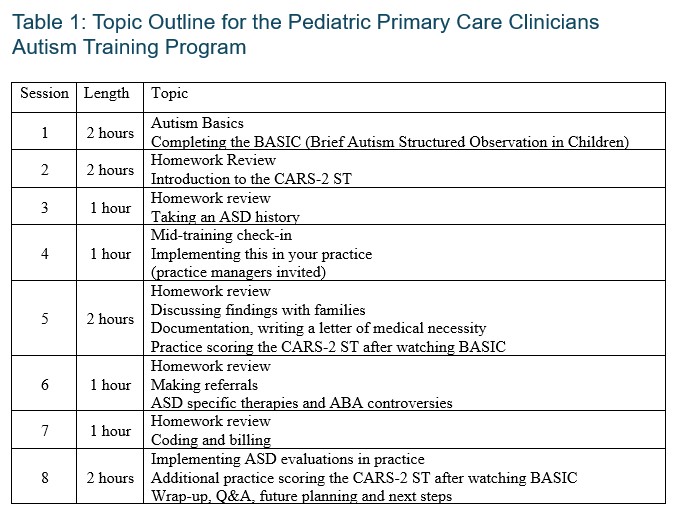 Topic Outline Pediatric Primary Care Clinicians Autism Training Program
Topic Outline Pediatric Primary Care Clinicians Autism Training ProgramTable 2
.jpg) Provider Demographics and Practice Characteristics
Provider Demographics and Practice Characteristics Table 1
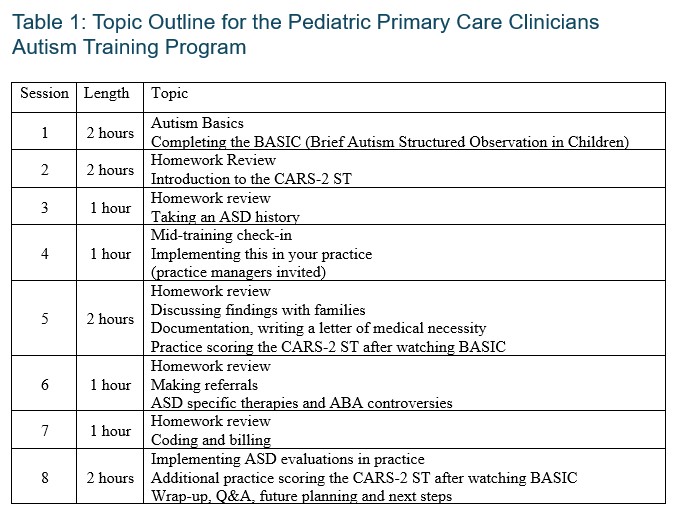 Topic Outline Pediatric Primary Care Clinicians Autism Training Program
Topic Outline Pediatric Primary Care Clinicians Autism Training ProgramTable 2
.jpg) Provider Demographics and Practice Characteristics
Provider Demographics and Practice Characteristics 
