Neonatal General 9: Hematology, Bilirubin and Feeding
Session: Neonatal General 9: Hematology, Bilirubin and Feeding
696 - Is there utility in testing CBC and Reticulocyte count in DAT positive ABO incompatible Neonates?
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 696.5955
Riley Phyu, Rowan Virtua School of Osteopathic Medicine, Clementon, NJ, United States; Caitlin Armstrong, Nemours Children's Hospital, Mullica Hill, NJ, United States; Ashish O. Gupta, Nemours Children's Hospital, Wilmington, DE, United States

Riley Phyu (she/her/hers)
Medical Student
Rowan Virtua School of Osteopathic Medicine
Clementon, New Jersey, United States
Presenting Author(s)
Background: ABO incompatibility occurs in 15-25% of pregnancies, yet only 1-5% of cases lead to significant hemolytic disease of the newborn (HDN). While some infants develop conditions such as anemia or hyperbilirubinemia, only a small percentage require major interventions. Despite this, routine testing—including CBC and reticulocyte counts—is widely performed in Direct Antiglobulin Test (DAT) positive neonates. Given the low incidence of severe complications, the necessity of these tests in the absence of clinical correlation is uncertain. We hypothesize that selective testing based on bilirubin levels could optimize care by reducing unnecessary labs, improving cost-effectiveness, and conserving resources without compromising outcomes.
Objective: To evaluate the utility of CBC and reticulocyte count in DAT positive ABO incompatible neonates.
Design/Methods: A retrospective study was conducted at a community hospital system with around 3000 births per year. Data was collected from 2018 to 2024, DAT+ ABO incompatible neonates born at ≥35 weeks of gestation were included in the study. Exclusion criteria included neonates who were DAT+ neonates with Rh-negative mothers or who had no ABO incompatibility. Data was collected from electronic medical records, including CBC, reticulocyte counts, bilirubin levels, need for phototherapy, IVIG or exchange transfusion. The project was approved by the hospital QI committee.
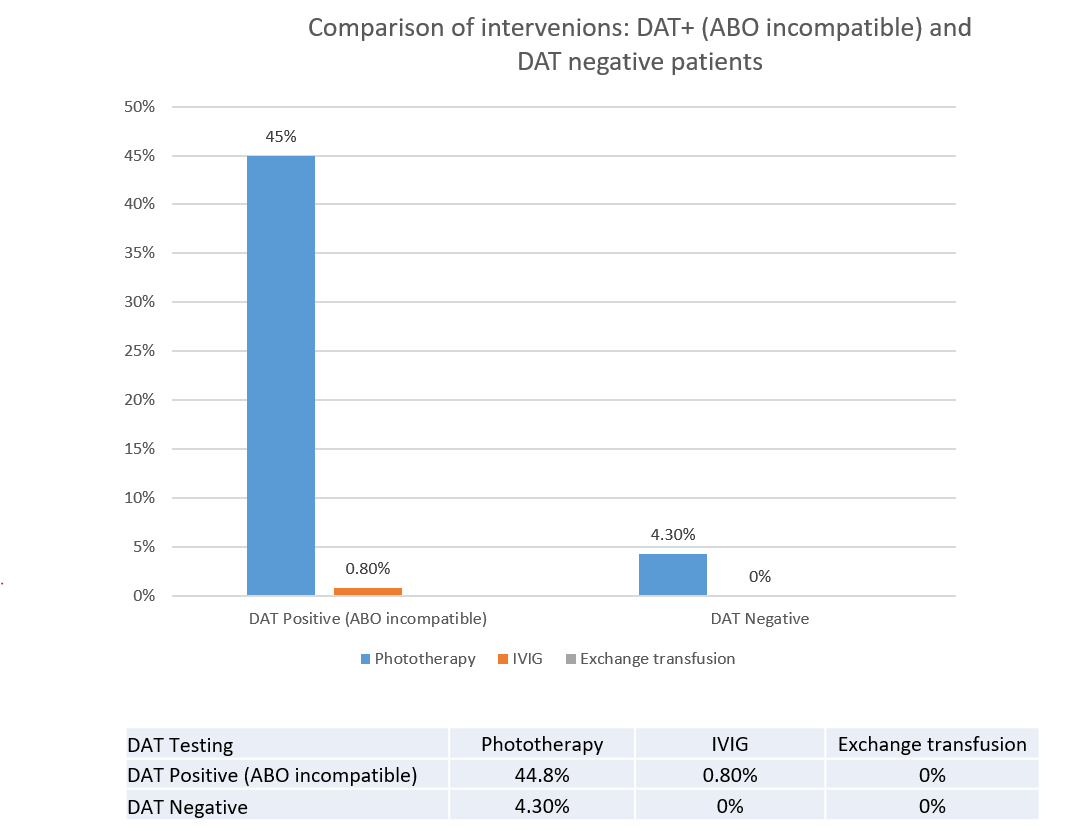
Results: Among 18,645 infants evaluated 781 (4.2%) were ABO incompatible and DAT+, and born at ≥35 weeks of gestation (Figure 1). CBC and reticulocyte counts were obtained in 96% of these infants. Seven of these infants (0.9%, 7/781) had laboratory signs of hemolysis (both hematocrit < 35% and reticulocyte count >6%). All seven infants exhibited elevated bilirubin levels requiring phototherapy by 12 hours of life. Overall, 45% ABO incompatible, DAT+ neonates required phototherapy (347/781), 6 received IVIG (0.8%), none required blood or exchange transfusion (Figure 2).
Conclusion(s): All DAT+ ABO incompatible infants with laboratory signs of hemolysis had hyperbilirubinemia-requiring phototherapy by 12 hrs of life. Routine lab testing with CBC and retic count does not add much value in clinical management of ABO incompatible infants. A change in clinical practice is warranted to reduce blood draws, heel pricks and potential cost savings.
Phyu_Riley Verification.pdf
Comparison of Interventions: DAT+ (ABO Incompatible) vs. DAT- Patients