Neonatal General 9: Hematology, Bilirubin and Feeding
Session: Neonatal General 9: Hematology, Bilirubin and Feeding
695 - Impact of a new anti-Xa based neonatal ECMO heparin management guideline on therapeutic anticoagulation and clinical outcomes: a single center experience
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 695.5471
Adriana Phillips, UPMC Childrens Hospital of Pittsburgh, Pittsburgh, PA, United States; John Ibrahim, UPMC Childrens Hospital of Pittsburgh, Pittsburgh, PA, United States; Burhan Mahmood, UPMC Childrens Hospital of Pittsburgh, Pittsburgh, PA, United States

Adriana Phillips, MD
Fellow Physician
UPMC Childrens Hospital of Pittsburgh
Pittsburgh, Pennsylvania, United States
Presenting Author(s)
Background: Hemostatic complications are a significant cause of morbidity and mortality during neonatal ECMO, with 30-40% of deaths attributed to hemorrhage or thromboembolism. Anticoagulation management of neonates is particularly challenging due to developmental immaturity of the hematologic system, coagulopathy secondary to underlying disease process, and the effect of the non-endothelial surface of the ECMO circuit.
Objective: We describe outcomes following implementation of a new anti-Xa based ECMO anticoagulation guideline in our NICU.
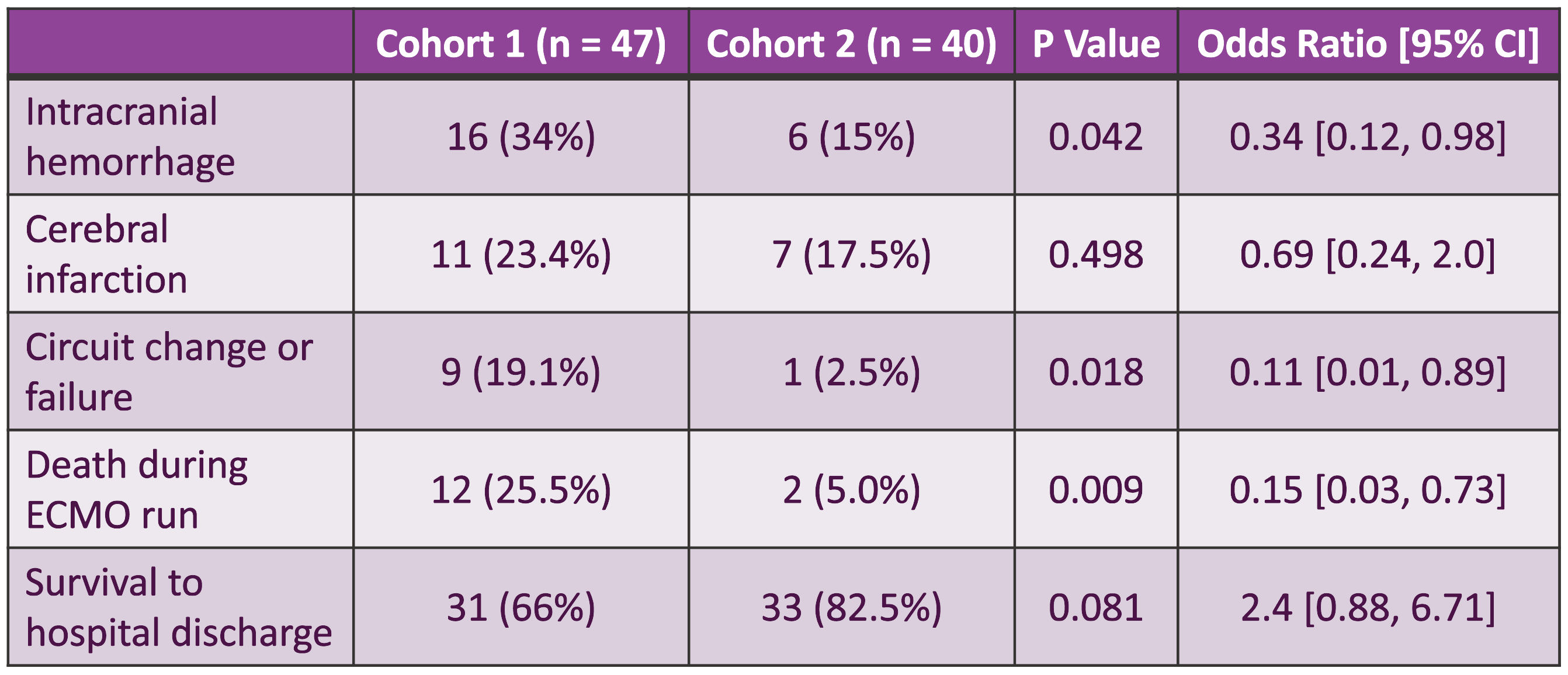
Design/Methods: We performed a retrospective, single-center chart review of neonatal ECMO patients admitted to our NICU from Jan 2013-Dec 2022, comparing anticoagulation management and clinical outcomes before and after implementation of a new anti-Xa based ECMO anticoagulation protocol. Patients were divided into Cohort-1 (pre-guideline) from Jan 2013-early Sept 2018 (n=47), and Cohort-2 (post-guideline) from late Sept 2018-Dec 2022 (n=40). Our primary outcome assessed adequacy of therapeutic heparin anticoagulation during ECMO. Secondary outcomes were incidence of intracranial hemorrhage, cerebral infarction, circuit change/failure, death during ECMO, and survival to hospital discharge.
Results: The demographics of the two cohorts were similar, with the only notable difference being duration of ECMO support, which was slightly shorter in Cohort-2 (5.3 vs 7.9 days, p=0.053). Patients in Cohort-2 (post-guideline) were significantly more likely to reach goal anti-Xa levels (97.5% vs 46.8%, p= < 0.001). For patients who achieved therapeutic anti-Xa levels, those in Cohort-2 reached that goal much sooner (27.4 vs 91.8 hours, p= < 0.001). Average heparin dose was higher in Cohort-2 (34.7 vs 27.9 units/kg/hour, p= < 0.001). Average PTT (136 vs 84.3, p= < 0.001) and anti-Xa level (0.32 vs 0.17, p= < 0.001) were also significantly higher in Cohort-2. Intracranial hemorrhage was lower in Cohort-2 (15% vs 34%, p=0.042). Incidence of cerebral infarction was lower in Cohort-2, although not statistically significant (17.5% vs 23.4%, p=0.498). Circuit change/failure was significantly lower in Cohort-2 (2.5% vs 19.1%, p=0.018). Risk of death while on ECMO was lower in Cohort-2 (5% versus 25.5%, p=0.009). Survival to hospital discharge was higher in Cohort-2, although not statistically significant (82.5% vs 66%, p=0.081).
Conclusion(s): In neonatal ECMO patients managed in our NICU, implementation of a new anti-Xa based heparin management guideline resulted in enhanced anticoagulation, reduced hemostatic complications, and improved clinical outcomes.
Patient Demographics
.png)
Anticoagulation Management
.png)
Clinical Outcomes