Neonatal GI Physiology & NEC 1
Session: Neonatal GI Physiology & NEC 1
711 - Primary Anastomosis versus Ostomy as Primary Surgical Intervention for Surgical Necrotizing Enterocolitis in Preterm Neonates: A Retrospective Cohort Study
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 711.6515
Dwayne Mascarenhas, The Hospital for Sick Children, Toronto, ON, Canada; Doaa Al-Dweik, The hospital of Sick Children, Toronto, ON, Canada; Jordan Mann, The Hospital for Sick Children, Toronto, ON, Canada; Telford Yeung, University of Calgary, Calgary, AB, Canada; Mary A. Woodward, The Hospital for Sick Children, Toronto, ON, Canada; Bonny Jasani, The Hospital for Sick Children, Toronto, ON, Canada
.jpg)
Dwayne Mascarenhas, MBBS, MD (Paeds), DM (Neonatology) (he/him/his)
Clinical Fellow
The Hospital for Sick Children
Toronto, Ontario, Canada
Presenting Author(s)
Background: Ostomy with or without mucous fistula is the standard of care in the management of surgical necrotizing enterocolitis (sNEC) in preterm infants. Although primary anastomosis (PA) is being increasingly utilized for sNEC, there is limited data on outcomes and complications compared to ostomy in preterm neonates.
Objective: To compare the mortality, morbidities and short-term outcomes of primary anastomosis versus ostomy as initial surgical modality in preterm infants with sNEC.
Design/Methods: We conducted a retrospective cohort study of preterm infants ≤30 weeks with sNEC at a single quaternary neonatal intensive care unit between January 1, 2016 and June 30, 2024 who underwent PA or ostomy. The pre-specified outcomes included mortality (NEC-attributable and all-cause), need for >1 laparotomy, post-procedural complications, nutritional outcomes, neonatal morbidities, anthropometric indices (weight, length, head circumference z-scores) at 36 weeks postmenstrual age. Mann-Whitney U test and Fisher’s exact test were used for comparing continuous and categorical data respectively between the two groups. Multi-logistic regression analysis was conducted to compare the outcomes between the two groups, adjusted for confounders.
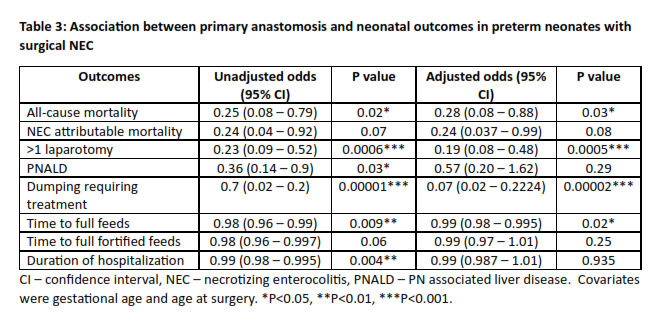
Results: Of the 139 preterm infants with sNEC, 79 (57%) infants underwent ostomy and 35 (25%) infants underwent PA. The baseline characteristics, details of surgical procedure, neonatal morbidities, and nutritional and anthropometric outcomes are outlined in Table 1. Compared to the PA group, the infants in the ostomy group were smaller (686 vs 836 g; p=0.002), younger (25 vs 25.9 weeks; p=0.004), had higher postnatal age at surgery (19 vs 8 days; p=0.02), increased need for >1 laparotomy (70 vs 34%; p=0.00), and had higher incidence of cholestasis (72 vs 48%; p=0.028), time to reach full feeds (85.5 vs 50.5 days; p=0.006), dumping needing loperamide (71 vs 13%; p = 0.00), mortality (33 vs 11%; p = 0.016), duration of hospital stay (141.5 vs 94 days; p=0.001) (Table 2). Post-adjusted analysis, the odds of all-cause mortality, NEC-attributable mortality, need for >1 laparotomy, dumping requiring treatment, and time to full feeds were significantly lower in PA group compared to ostomy (Table 3).
Conclusion(s): Primary anastomosis may have numerous short-term benefits with no increase in complications compared to ostomy in preterm infants with surgical NEC, though selection bias cannot be ruled out. Peri-operative considerations such as severity of NEC, intra-operative findings, and hemodynamic stability could be important factors for decision regarding initial surgical modality.
Table 1: Baseline characteristics
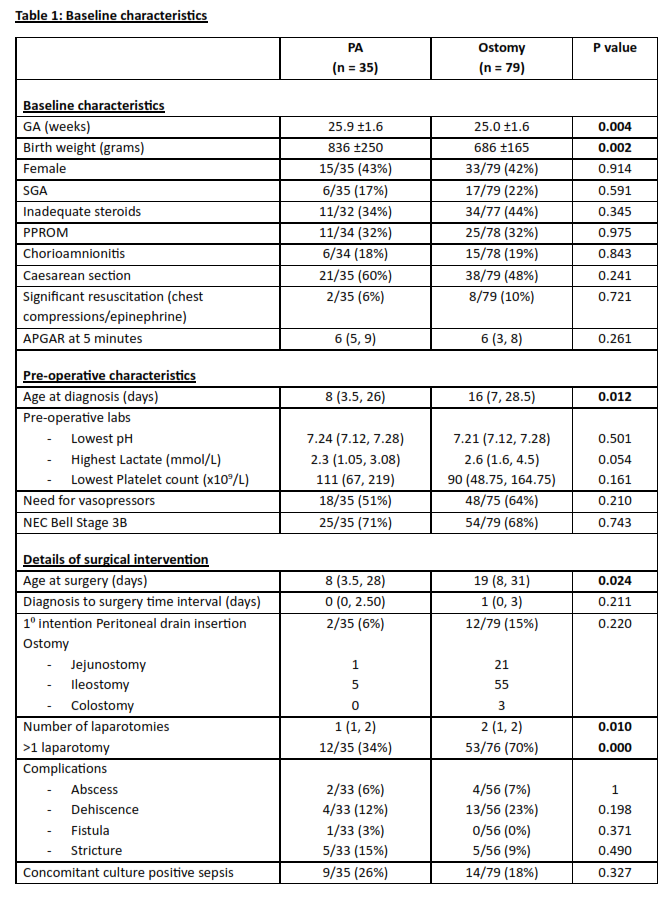
Table 2: Mortality, nutritional, cardio-respiratory, growth outcomes
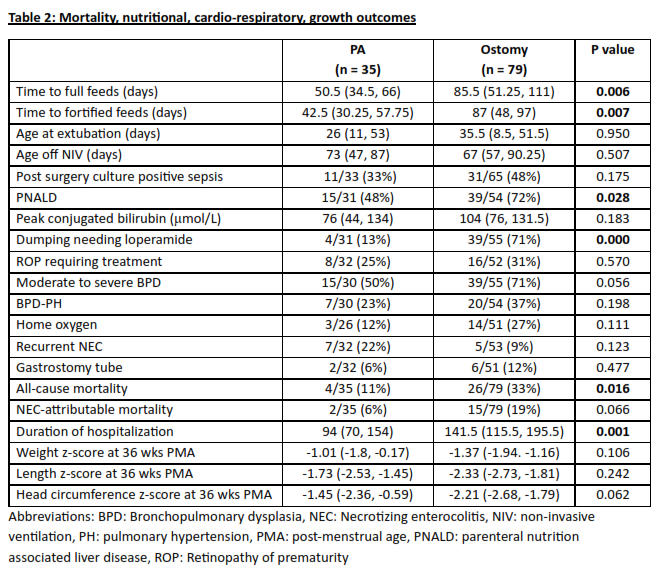
Table 3: Association between primary anastomosis and neonatal outcomes in preterm neonates with surgical NEC