Breastfeeding/Human Milk 1
Session: Breastfeeding/Human Milk 1
637 - The Impact of Expanding Donor Human Milk in Neonatal Intensive Care Units to Moderate and Late Preterm Infants
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 637.6925
Sarah Mahoney, Yale School of Medicine, New Haven, CT, United States; Veronika Shabanova, Yale School of Medicine, New Haven, CT, United States; Sarah Taylor, Yale School of Medicine, New Haven, CT, United States

Sarah Mahoney, BS, BA (she/her/hers)
MD-PhD Candidae
Yale School of Medicine
New Haven, Connecticut, United States
Presenting Author(s)
Background: Feeding donor human milk (DHM), when maternal milk (MM) is not available, is recommended for infants at risk for necrotizing enterocolitis. DHM provision is limited by cost and chronic shortages, therefore often reserved for primarily very early and early preterm infants. However, many hospitals have expanded DHM supplementation to moderate and late preterm infants to avoid formula while MM supply is established.
Objective: To evaluate the impact of DHM provision on feed exposures and feeding-related outcomes for infants in the NICU born 32-35 weeks’ gestational age (GA).
Design/Methods: This multicenter retrospective cohort study includes EMR data from 11/2018-4/2022 from two institutions—one who initiated a DHM program (Bridgeport) for 32-35 weeks GA infants (the test group) and one who did not (YNHH) (the control). Infants were grouped by birth pre- and post-intervention intervals defined by DHM at Bridgeport. Outcomes include feed exposures, length of parenteral nutrition (PN), time to regain birth weight (BW), and breastfeeding at discharge. We used difference-in-differences (logistic, Poisson, and negative binomial models) and Cox regressions to compare outcomes, adjusting for race and length of stay (LOS). Statistical significance was set at a two-sided alpha of 0.05.
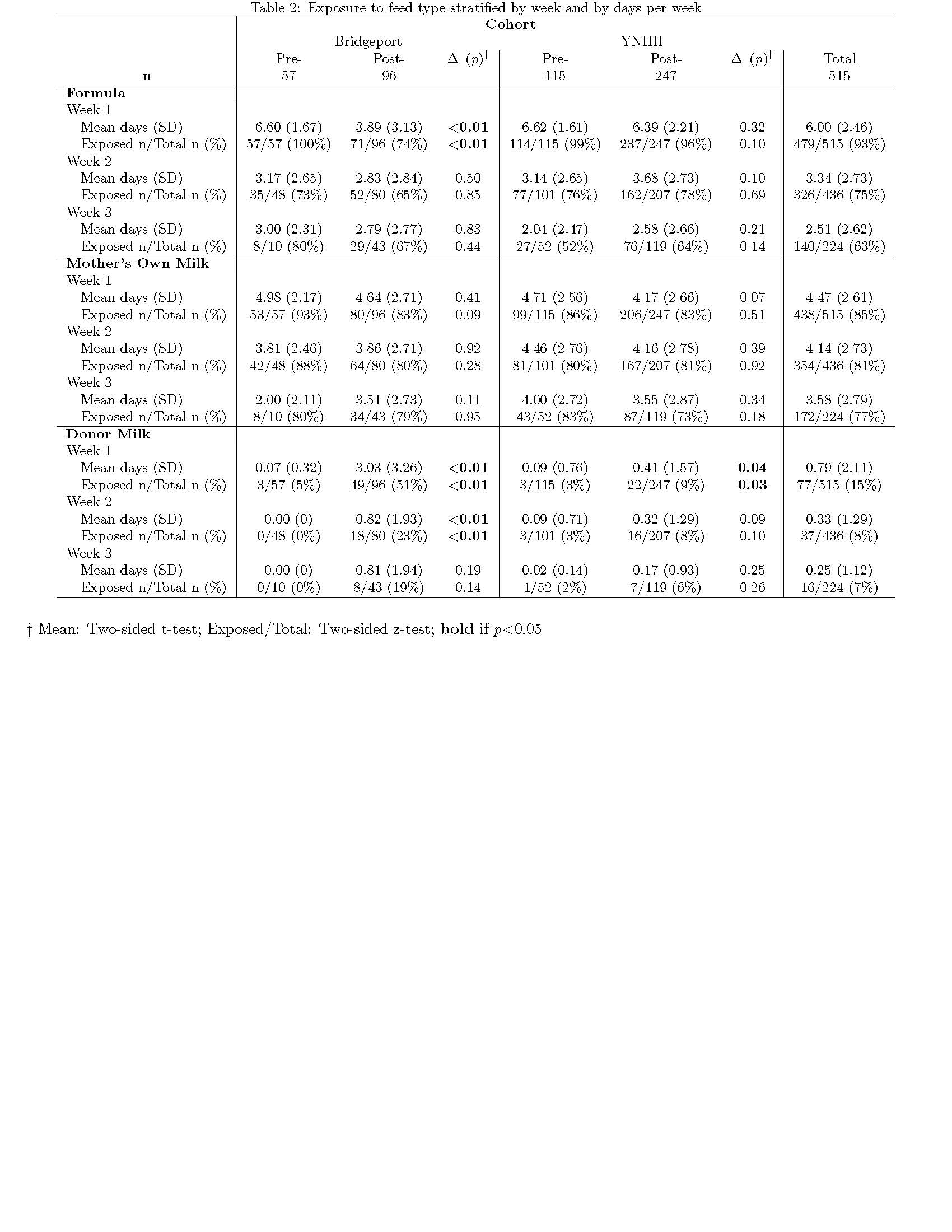
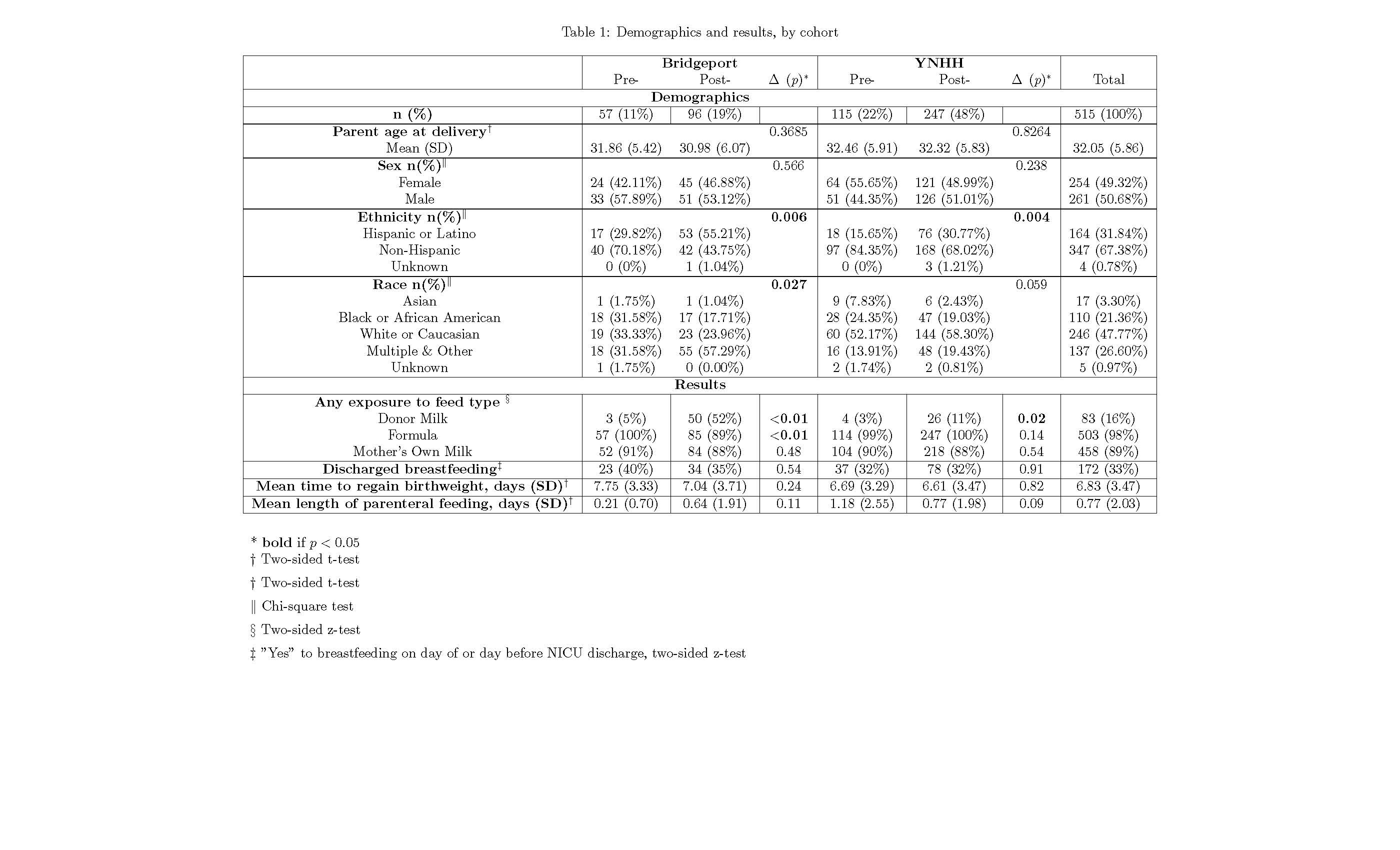
Results: Comparing infant outcomes at YNHH with those at Bridgeport in the pre- vs post-intervention time periods, 515 infants met inclusion criteria and differed between groups in race and ethnicity but not sex or parent age (Table 1). In adjusted analyses, YNHH infants were more likely to be exposed to formula [relative risk (RR) 1.46 (95% confidence interval 1.18-1.81)], and infants at both YNHH and Bridgeport were more likely to be exposed to DHM [RR 7.69 (2.52-23.42)], though this association was greater at Bridgeport than YNHH [RR 5.26 (3.23-8.33)]. Infants at YNHH were more likely to be exposed to MM [RR 1.33 (1.06- 1.66)]. LOS was associated with greater likelihood of DHM [RR 1.04 (1.02-1.06)] and MM [RR 1.00 (1.00-1.01)] exposure. The weekly feeding exposure differences at Bridgeport were less formula in week 1 and more DHM in weeks 1-2 (Table 2). Breastfeeding at discharge and length of PN did not differ between groups. Infants at YNHH were faster to regain BW (HR 1.64 [1.01-2.65]) (Figure 1).
Conclusion(s): A program to supplement MM with DHM was associated with increased DHM exposure and reduced formula use, but did not impact breastfeeding rates at discharge or length of PN. At the hospital with the DHM program, infants regained BW more slowly and had lower MM exposure.
Demographics and results, by cohort
Time to Regain Birthweight
Screenshot 2024-11-04 at 10.43.16.jpeg
Exposure to feed type stratified by week and by days per week