Neonatal GI Physiology & NEC 1
Session: Neonatal GI Physiology & NEC 1
710 - Bowel Ultrasound for Necrotizing Enterocolitis: Availability, Usage, and Challenges
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 710.4156
Alain Cuna, Children's Mercy Hospitals and Clinics, Kansas City, MO, United States; Amina M. Bhatia, Children’s Healthcare of Atlanta, Atlanta, GA, United States; Amy E.. O'Connell, Boston Children's Hospital, Boston, MA, United States; Bhuvaneshwari Jagadesan, University of Tennessee Health Science Center College of Medicine, Memphis, TN, United States; Catalina Le Cacheux, UPMC Childrens Hospital of Pittsburgh, Pittsburgh, PA, United States; Catherine J. Hunter, Oklahoma Children's Hospital, Nichols Hills, OK, United States; Hala Chaaban, Oklahoma University health sciences, Okl, OK, United States; Irfan Ahmad, CHOC Children's Hospital of Orange County, Tustin, CA, United States; Julie Thai, Children's Hospital Los Angeles, Los Angeles, CA, United States; Kate Louise M. Mangona, University of Texas Southwestern Medical School, Dallas, TX, United States; Katie Huff, Indiana University School of Medicine, Indianapolis, IN, United States; Kera McNelis, Emory University School of Medicine, Atlanta, GA, United States; Lauren Frazer, UNC Chapel Hill, Chapel Hill, NC, United States; Leeann Pavlek, Nationwide Children's Hospital, Columbus, OH, United States; Loren Berman, Nemours Children's Hospital, Wilmington, DE, United States; Mohan Pammi, Baylor College of Medicine, Houston, TX, United States; Muralidhar Premkumar, Baylor College of Medicine, Houston, TX, United States; Parvesh Garg, Wake Forest School of Medicine of Wake Forest Baptist Medical Center, Winston salem, NC, United States; Pritha Nayak, UTSW, Dallas, TX, United States; Toby D. Yanowitz, University of Pittsburgh School of Medicine, Pittsburgh, PA, United States

Alain Cuna, MD (he/him/his)
Neonatologist
Children's Mercy Hospitals and Clinics
University of Missouri Kansas City
Kansas City, Missouri, United States
Presenting Author(s)
Background: Bowel ultrasound (BUS) is increasingly reported as a valuable tool for evaluating necrotizing enterocolitis (NEC), yet there is limited knowledge regarding its actual use in clinical practice.
Objective: To assess the availability, clinical use, and perceived barriers to implementing BUS for NEC.
Design/Methods: An online survey was distributed to the 46 members of Children’s Hospitals Neonatal Consortium, a network of level IV NICUs in the United States and Canada. Responses were obtained from neonatologists, pediatric radiologists, and pediatric surgeons at each site.
Results: A total of 39 out of 46 sites (85%) provided 80 responses: 32 from neonatologists, 25 from pediatric surgeons, and 23 from pediatric radiologists (Table 1).
Availability: BUS was available in 90% (35/39) of primary level IV NICU sites and 41% (24/54) of affiliated level III NICUs. About 60% of level IV NICUs reported having 24/7 BUS availability and 40% having limited availability during nights or weekends.
Usage: BUS was universally used to supplement radiographs on a per-case basis; and was primarily requested by neonatologists, followed by pediatric surgeons then radiologists (Fig 1A). BUS was most often used to assess cases with questionable pneumatosis or gasless abdomen on radiographs, occasionally used to guide decisions regarding surgery, and rarely used to manage decisions regarding feeding or antibiotics (Fig 1B). Point-of-care BUS for NEC by neonatologists or surgeons was rare (4%). Radiologists were more likely to be aware of clinical guidelines for BUS use compared to neonatologists and surgeons (Fig 1C). Pediatric radiologists had the most training and expertise in BUS, while neonatologists had the least (Fig 1D).
Challenges: Sites using BUS cited the lack of guidelines and education as primary barriers, while non-using sites highlighted the lack of trained personnel (Table 2). Both using and non-using sites acknowledged the lack of high-quality evidence as a moderate barrier.
Conclusion(s): BUS availability for evaluating NEC remains concentrated in level IV NICUs of children’s hospitals. Neonatologists are the main users of BUS; however, neonatologists also have minimal training in directly performing or interpreting BUS. BUS is mainly used as an adjunct to radiographs for diagnosing NEC and occasionally to guide surgical management. The biggest barrier for sites not using BUS is the lack of trained personnel, while guidelines and education represent key opportunities for improvement at sites already using it. Further studies are needed to confirm if adding BUS to radiographs leads to improved outcomes.
Table 1. Participant Characteristics and Availability of BUS
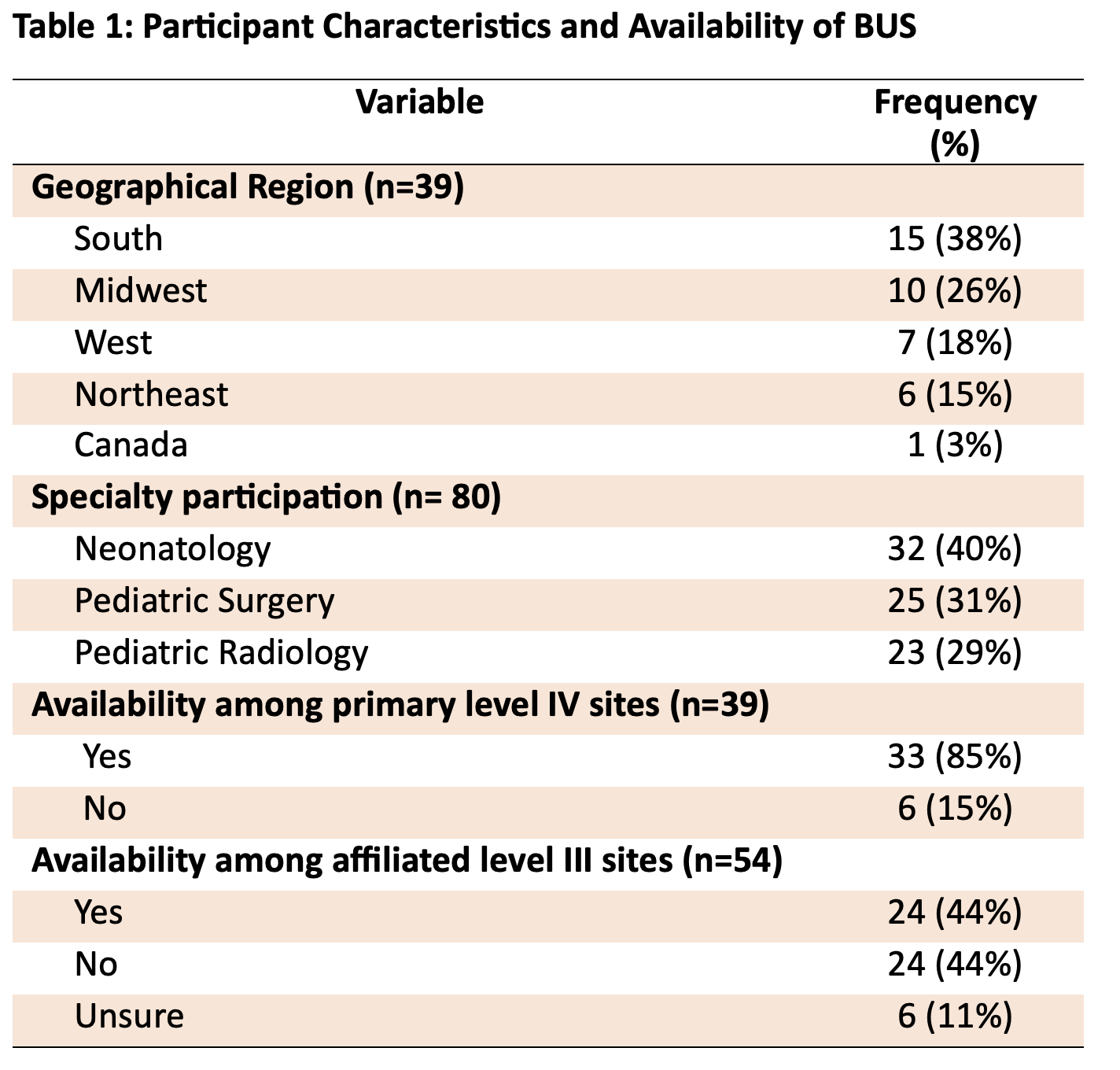
Figure 1. Use of BUS among the Level IV NICU Sites.
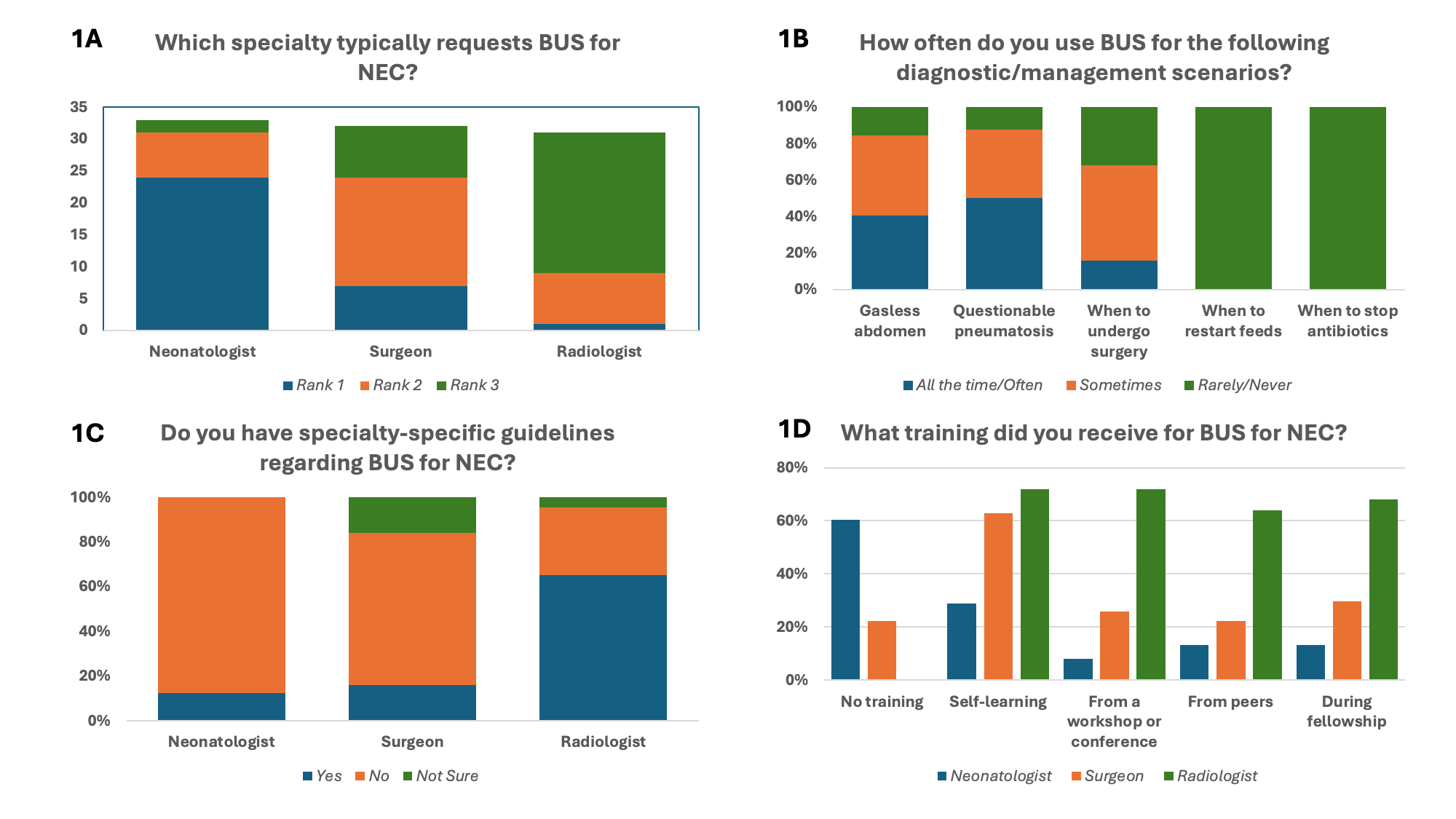 A: Users of BUS for NEC. Each responder was asked to rank which specialty typically requests BUS for NEC evaluations, with 1 being the most common and 3 being the least common B. Case-scenarios when BUS is used. C. Guidelines for using BUS across specialties. D. Training received regarding the use of BUS.
A: Users of BUS for NEC. Each responder was asked to rank which specialty typically requests BUS for NEC evaluations, with 1 being the most common and 3 being the least common B. Case-scenarios when BUS is used. C. Guidelines for using BUS across specialties. D. Training received regarding the use of BUS.Table 2: Challenges to Implementing BUS.
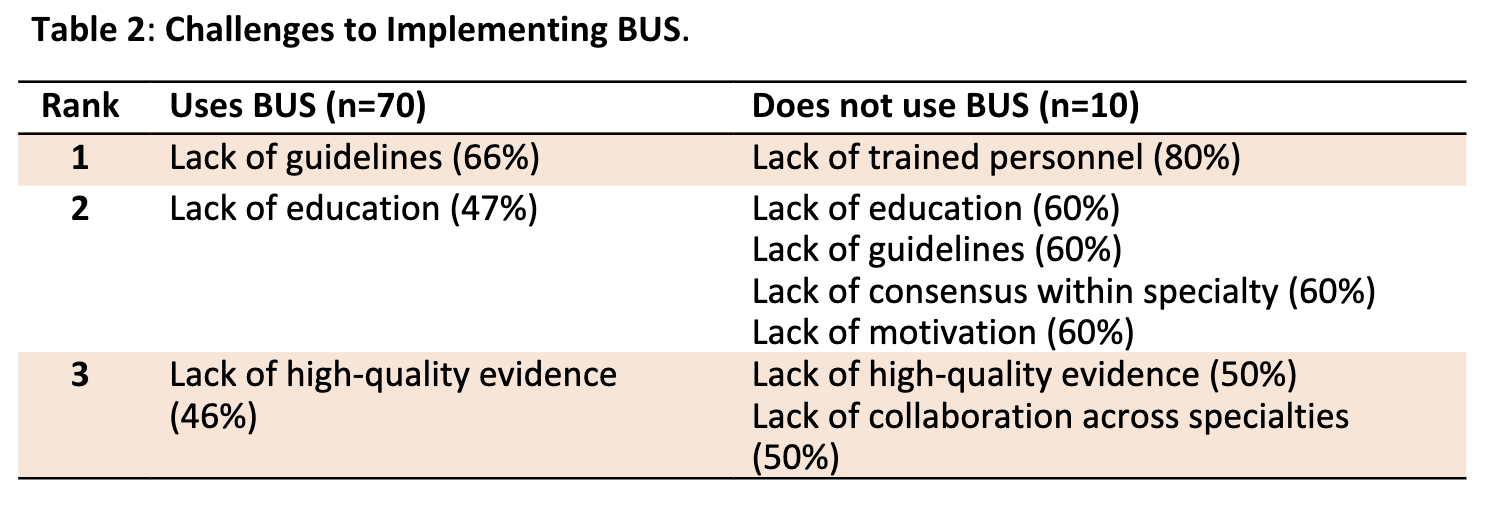 Top 3 perceived barriers to BUS among responders that use and do not use BUS at their site.
Top 3 perceived barriers to BUS among responders that use and do not use BUS at their site.
