Neonatal Fetal Nutrition & Metabolism 2
Session: Neonatal Fetal Nutrition & Metabolism 2
623 - Can we improve interpretation of early Zinc (Zn) levels with the use of a regression equation in very preterm (VPT), <33 Weeks Gestational Age (GA) or Very Low Birthweight (VLBW, <1,500 g) newborns?
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 623.4209
Dimitrios Angelis, University of Texas Southwestern Medical School, Dallas, TX, United States; Tina A. Seidu, University of Texas Southwestern Medical School, Dallas, TX, United States; Roy Heyne, University of Texas Southwestern Medical School, Southlake, TX, United States; L. Steven Brown, Parkland Health, Dallas, TX, United States; Audrey Edwards, Parkland Health, Dallas, TX, United States; Cheryl S. Lair, Parkland Health & Hospital System, Arlington, TX, United States; Myra H. Wyckoff, UT Southwestern, Dallas, TX, United States; David B. Nelson, University of Texas Southwestern Medical School, Dallas, TX, United States; Luc (middle name P) P. Brion, University of Texas Southwestern Medical School, Dallas, TX, United States
- DA
Dimitrios Angelis, MD (he/him/his)
Neonatologist
University of Texas Southwestern Medical School
Dallas, Texas, United States
Presenting Author(s)
Background: Zn deficiency is frequently encountered in premature infants, since most of Zn accretion in the fetus occurs in the 2nd and 3rd trimesters. The normal range of serum Zn levels in preterm infants is 0.74-1.46 mcg/ml (ASPEN, ESPGHAN). Zn deficiency can be associated with growth failure in preterm infants. Serum Zn levels at birth decline with gestational age (GA) secondary to a variety of poorly defined factors (inverse Zn clearance with GA, high Zn turnover etc.), and as result, the above defined normative levels might not be accurate for premature infants. Low serum Zn level at birth could result from maternal Zn deficiency, decreased placental transport, decreased fetal storage and/or delivery factors.
Objective: To describe 1. a regression equation of early Zn (defined as < 48hrs postnatal) in relation to GA in a population of VPT/VLBW and 2. factors associated with low ratio of measured (M) to predicted (P) values, which could be a possible marker of early Zn deficiency.
Design/Methods: Early serum Zn levels obtained in VLBW-VPT infants born at Parkland hospital between 01/2022 till 07/2023 were analyzed by GA. We then calculated the ratio of M to P values as a possible marker of early Zn deficiency. Statistical analysis included nonlinear regression analysis and logistic regression analysis using SPSS and SAS.
Results: Early Zn was available in 218/348 of infants. Baseline characteristics in this cohort were shown in Table 1. The median level of Zn was 0.98 mcg/ml (0.85, 1.19). The level decreased with increasing GA (Figure 1); this decrease fitted best quadratic regression (Table 1a). The individual M/P ratio was calculated using P estimated from the formula at the same GA (Table 2a). In multivariable stepwise analysis, the M/P ratio was lower in association with race/ethnicity (other vs Non-Hispanic Black, non-Hispanic White and Hispanic), high ZIP code-related poverty index, high maternal BMI, and exposure to antenatal steroids, and higher in association with prenatal care. It was not associated with medical insurance, maternal diabetes mellitus, sex, small for GA, multiple pregnancy (Table 2b). Similar associations were not significant if only M was used.
Conclusion(s): Early Zn level is usually normal-high based on currently suggested normative levels, especially in newborns of lower GA. The ratio of initial Zn level to expected level for GA as described by the quadratic equation here might be a promising marker of early Zn assessment in premature newborns but needs further validation. The significance of low Zn levels currently is unclear. Our study could ignite further research on this area.
Early Serum Zinc levels (first 48 hours of life) by gestational age.
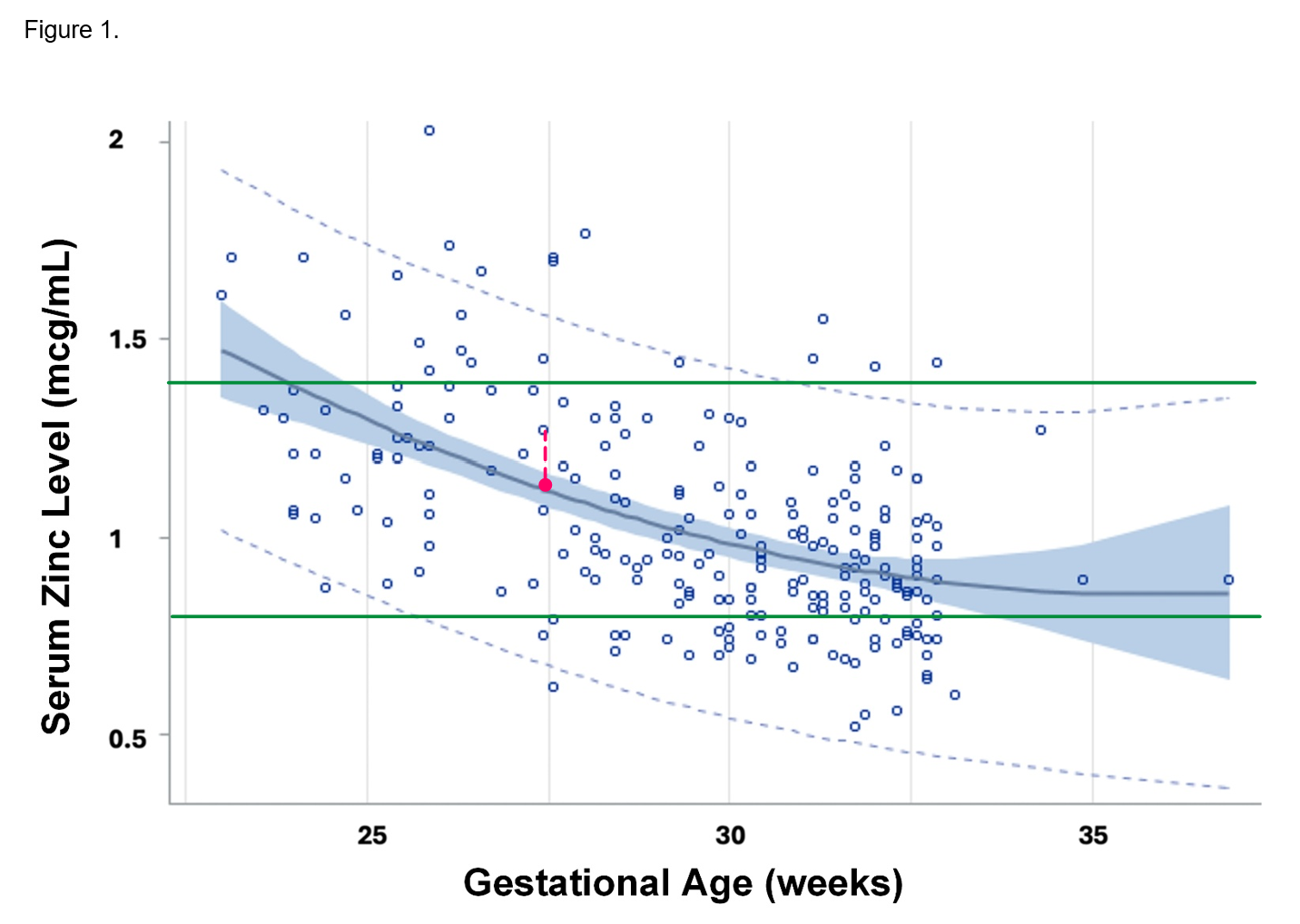 95% confidence and prediction intervals of first zinc level during the first 48 hours of life versus gestational age among infants <33 weeks gestational age or <1500 g birth weight, excluding those without congenital anomalies or comfort care only. Quadratic regression analysis. Adjusted R2=0.2921, n=228, P<0.0001. Equation: Zn = 5.63727 -0.26622 X GA +0.00370 x GA2. Green lines: currently accepted normative Zn values (0.74-1.46 mcc/dl). Red dashed line connects a measured Zn value (M) with its corresponding predicted (P- red dot). The M/P Zn ratio was calculated for each premature infant. Abbreviations: Zn, serum zinc concentration; GA, gestational age (weeks)
95% confidence and prediction intervals of first zinc level during the first 48 hours of life versus gestational age among infants <33 weeks gestational age or <1500 g birth weight, excluding those without congenital anomalies or comfort care only. Quadratic regression analysis. Adjusted R2=0.2921, n=228, P<0.0001. Equation: Zn = 5.63727 -0.26622 X GA +0.00370 x GA2. Green lines: currently accepted normative Zn values (0.74-1.46 mcc/dl). Red dashed line connects a measured Zn value (M) with its corresponding predicted (P- red dot). The M/P Zn ratio was calculated for each premature infant. Abbreviations: Zn, serum zinc concentration; GA, gestational age (weeks)Table 1. Baseline maternal and neonatal characteristics in the cohort.
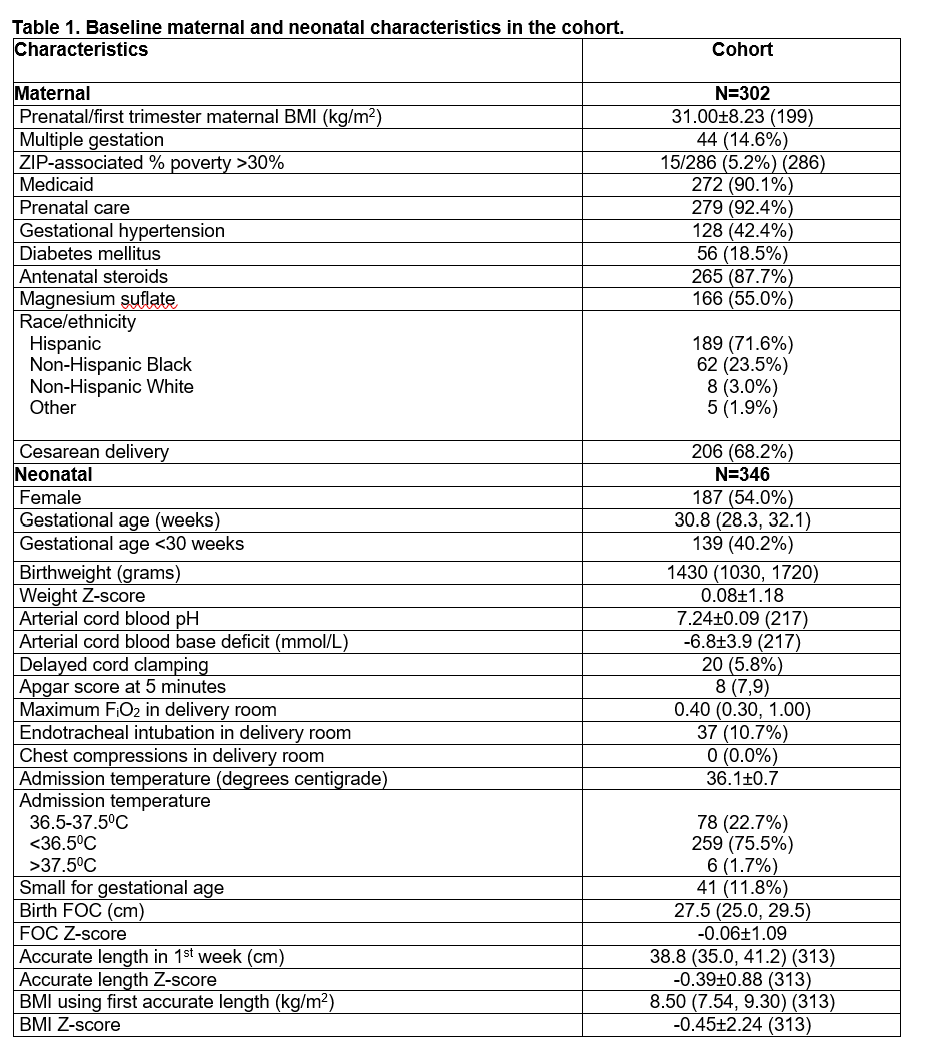
The discrepancy between the number of maternal and neonatal characteristics corresponds to multiple pregnancies. Values are mean ± SD (n if less than N in top row), median (IQR) (n if number < N in upper row) or number (%). Abbreviations: BMI, body mass index; FiO2, fractional inspiration level of oxygen; FOC, fronto-occipital circumference
Table 2. Initial serum zinc level: First serum zinc concentration within the first 48 hours among infants born at Parkland excluding infants on comfort care only and those with severe congenital anomalies Table 2a. Quadratic normative regression vs gestational age. Table 2b. Multivariable analysis of the ratio of initial serum zinc concentration to GA-expected value from quadratic regression versus prenatal and early neonatal variables
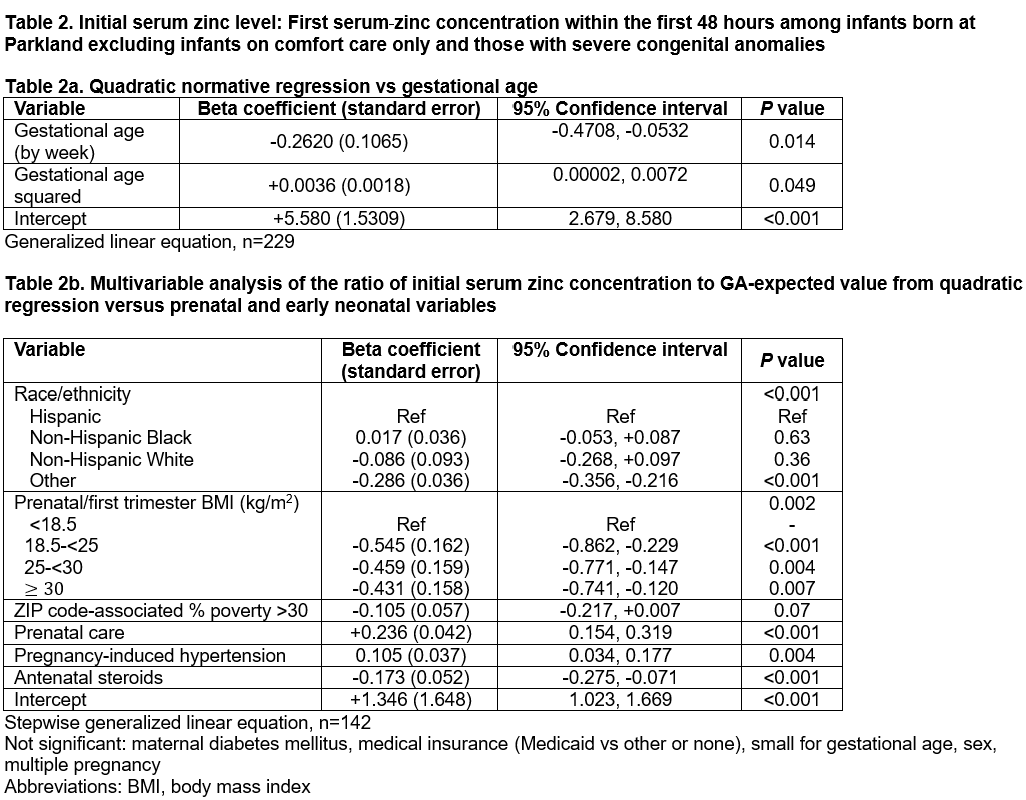 Stepwise generalized linear equation, n=142
Stepwise generalized linear equation, n=142Not significant: maternal diabetes mellitus, medical insurance (Medicaid vs other or none), small for gestational age, sex, multiple pregnancy
Abbreviations: BMI, body mass index

