Breastfeeding/Human Milk 2
Session: Breastfeeding/Human Milk 2
653 - Impact of Tongue Mobility on Breastfeeding Function: A Combined Clinical and Ultrasound Study
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 653.5452
Diklah Zipora. Barak, Schneider Children's Medical Center of Israel, Koranit, HaZafon, Israel; Sigal Portnoy, Tel Aviv University, Tel Aviv, Tel Aviv, Israel; Liat Ashkenazi Hoffnung, Schneider Children's Medical Center, Patach Tikva, Tel Aviv, Israel; Ron Berant, Schneider Children's Medical Center of Israel, Givat Shmuel, HaMerkaz, Israel
- DB
Diklah Zipora Barak, MSc OT, IBCLC (she/her/hers)
Occupational Therapist
Schneider Children's Medical Center of Israel
Koranit, HaZafon, Israel
Presenting Author(s)
Background: The complex biomechanical process of breastfeeding involves different anatomical and physiological components of the mother-infant dyad. The infant’s tongue is the shared organ in both oral and pharyngeal phases of feeding. Previous studies either correlated tongue anatomy with clinical measures, or evaluated tongue biomechanics using ultrasound with limited clinical measures.
Objective: To examine the function of breastfeeding via correlations between clinical assessments and ultrasound biomechanic measurements. Specifically, we focused on milk transfer rate, pain, gastroesophageal reflux symptoms, and both existing and novel ultrasound US measurements.
Design/Methods: Twenty-one dyads of mothers and 3-6 weeks old infants were recruited for the study. Three categories of measurements were collected in a single session. The Lingual Frenulum Protocol for Infants (LFPI) was used to assess mouth anatomy and tongue motility, with an additional novel emphasis on lateralization using a modified lateralization scale. Breastfeeding difficulties were assessed using reflux, nipple pain and self-efficacy questionnaires. Real-time ultrasound imaging (POCUS) was used to measure tongue motility.
Results: Milk transfer rate was predicted by pain at attachment and ultrasound measurement of the angle between the hard-soft-palate junctions with the tongue in its superior position. These measures explained 59.8% of the milk transfer rate variance (p=0.002). Infants who used a pacifier (n=14) showed lower lateralization scores (z=-2.7, p=0.006). The Infant Gastroesophageal Reflux Questionnaire-revised (I-GERQ-R) scores correlated with the change in nipple diameter (r=-0.598, p=0.009).
Conclusion(s): This study combined various clinical and imaging variables that were previously measured separately, allowing to discover novel correlations and clinical implications. Notably, reflux symptoms might originate from suboptimal latch and this etiology should be explored. Milk transfer rate emerged as a promising clinical measure linked to the biomechanical aspects of breastfeeding. Angle measurements in the ultrasound are a novel quantity that was correlated to clinical measures. Pacifier use was associated with decreased tongue mobility, indicating potential impacts on feeding mechanics. These insights could affect clinical practices in breastfeeding support and highlight the importance of tongue assessments in early infancy.
Example ultrasound of two subjects
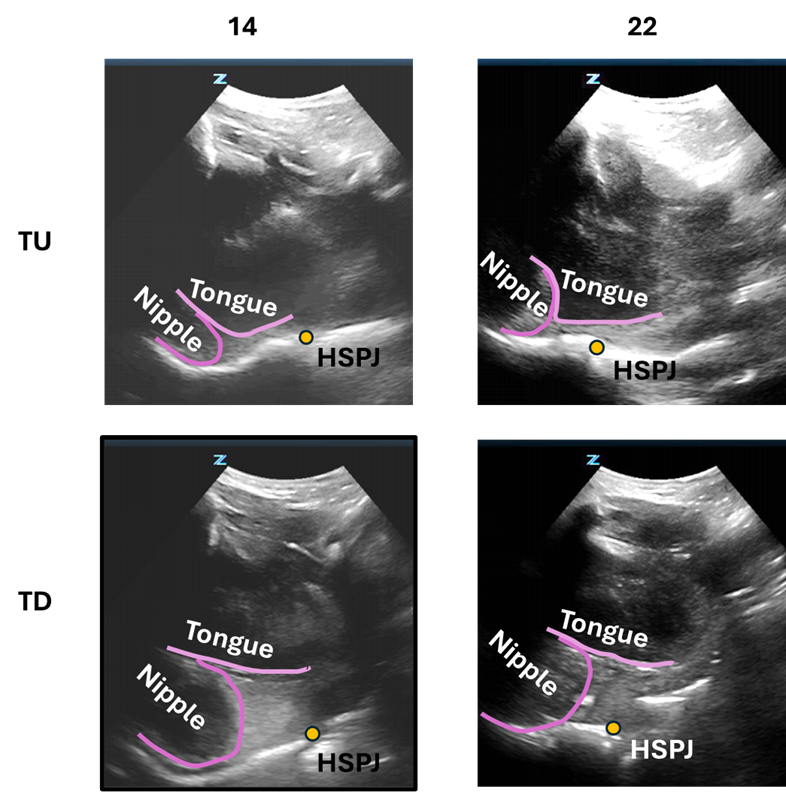 Subjects 14 (left) and 22 (right) exemplify differences in both ultrasound and clinical parameters. Subject 22 displays several clinical difficulties, compared with subject 14, among which are low milk transfer rate, poor lateralization, poor LFPI score. The mother experiences nipple pain, and shows less confidence in her breastfeeding (Table 2). In the ultrasound, subject 22 shows a small change in nipple diameter. Rows show the tongue up (TU) and tongue down (TU) positions. Nipple and tongue contours are shown in pink. The Hard-soft palate junction (HSPJ) is depicted with a yellow dot.
Subjects 14 (left) and 22 (right) exemplify differences in both ultrasound and clinical parameters. Subject 22 displays several clinical difficulties, compared with subject 14, among which are low milk transfer rate, poor lateralization, poor LFPI score. The mother experiences nipple pain, and shows less confidence in her breastfeeding (Table 2). In the ultrasound, subject 22 shows a small change in nipple diameter. Rows show the tongue up (TU) and tongue down (TU) positions. Nipple and tongue contours are shown in pink. The Hard-soft palate junction (HSPJ) is depicted with a yellow dot.Two example subjects with high and low milk transfer rate
.png) Two example subjects with high and low milk transfer rate. Abbreviations: Infant Gastroesophageal Reflux Questionnaire- revised (I-GERQ-R), Lingual frenulum protocol for infants (LFPI), Breastfeeding self-efficacy short form (BSES-SF), tongue up (TU), tongue down (TD).
Two example subjects with high and low milk transfer rate. Abbreviations: Infant Gastroesophageal Reflux Questionnaire- revised (I-GERQ-R), Lingual frenulum protocol for infants (LFPI), Breastfeeding self-efficacy short form (BSES-SF), tongue up (TU), tongue down (TD).Pacifier use and lateralization difficulties.
.png) Histogram of lateralization scores (0 – best, 3 – worst) split according to pacifier use. Infants who use a pacifier had higher lateralization scores.
Histogram of lateralization scores (0 – best, 3 – worst) split according to pacifier use. Infants who use a pacifier had higher lateralization scores.
