Neonatal General 8: Growth, Nutrition and Feeding
Session: Neonatal General 8: Growth, Nutrition and Feeding
687 - Impact of glucose gel on NICU admissions in SGA vs LGA infants with hypoglycemia.
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 687.5203
Navnoor Singh, Southern Illinois University School of Medicine, Springfield, IL, United States; Navnoor Singh, Southern Illinois University School of Medicine, Springfield, IL, United States; Melanie Nielsen, Southern Illinois University School of Medicine, Carbondale, IL, United States; Venkata S. Majjiga, SIU School of Medicine, Chatham, IL, United States; Sheref Unal, Southern Illinois University School of Medicine, Springfield, IL, United States; Sean McGinity, Southern Illinois University School of Medicine, Springfield, IL, United States; Erin M. Bauer, Southern Illinois University School of Medicine, Springfield, IL, United States; Mohamed F. Ahamed, SIU Medicine, Springfield, IL, United States

Navnoor Singh, MD
Resident
Southern Illinois University School of Medicine
Springfield, Illinois, United States
Presenting Author(s)
Background: Neonatal hypoglycemia (NH) is commonly seen in high risk newborns, i.e. those born premature, small or large for gestational age (SGA/LGA), or to diabetic mothers (IDM). Oral glucose gel is used to treat hypoglycemia, reduce NICU admissions, and promote mother-baby bonding and breastfeeding in these infants. However, there has been no study that compares the effect of glucose gel based on risk factors in the subgroups of infants born SGA vs LGA.
Objective: We will compare the rate of NICU admission and exclusive breastfeeding in
1. Infants born at ≥34 weeks GA requiring glucose gel for hypoglycemia based upon their being born SGA vs LGA, and
2. IDM with mothers on insulin vs diet control/oral medications.
Design/Methods: This is a retrospective cohort study of infants at risk for hypoglycemia born at a tertiary regional perinatal center (~2600 deliveries annually). Infants born between 3/2022-5/2024 who were SGA/LGA/IDM and underwent blood sugar monitoring were identified. Data was collected on those infants who developed hypoglycemia requiring glucose gel. Analyzed data included baseline characteristics, volume and number of doses of glucose gel administered, need for NICU admission, rates of exclusive breastfeeding at the time of discharge, and maternal comorbidities such as diabetes mellitus (DM) and treatment type for DM. Data was analyzed using Fischer’s exact test, Welch 2 sample t-test, and Pearson’s Chi square test with p< 0.05 considered as significant.
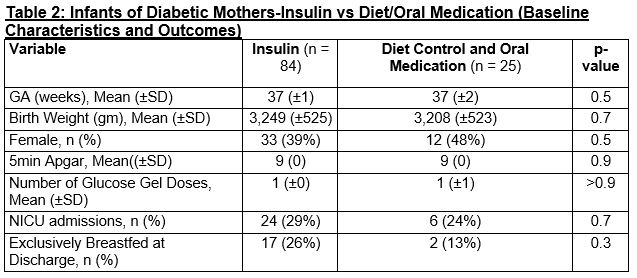
Results: A total of 445 babies required glucose gel, of which 76 were SGA and 63 were LGA. The mean GA was 37 weeks for both groups. Rate of maternal diabetes was higher in LGA group (21% vs 50%, p< 0.001) but other baseline characteristics were similar (Table 1). The rate of NICU admission did not differ between the two groups (24% vs 27%, p=0.6), however, LGA babies required glucose gel twice as frequently but this was not found to be statistically significant (p=0.2). The rates of exclusive breastfeeding at discharge were similar (p=0.7). 84 of the 109 IDM’s were born to mothers receiving insulin. Baseline variables, NICU admission, and breast-feeding rates between the infants whose mothers received insulin vs oral medications/diet controlled were similar (Table 2).
Conclusion(s): Of the babies requiring glucose gel for hypoglycemia, no significant differences were found in the rate of NICU admissions or exclusive breastfeeding rates in SGA vs LGA infants though LGA infants require twice as many doses of glucose gel to achieve this.
Table 1. SGA vs LGA (Baseline characteristics and outcomes)
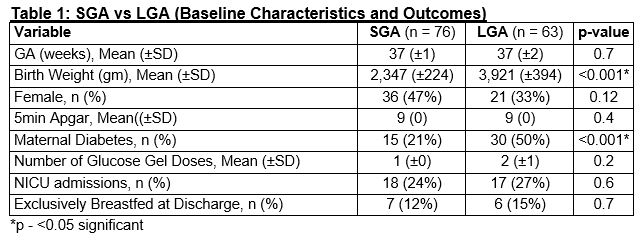
Table 2. Infants of Diabetic Mothers- Insulin vs Diet/Oral Medication (Baseline Characteristics and Outcomes)
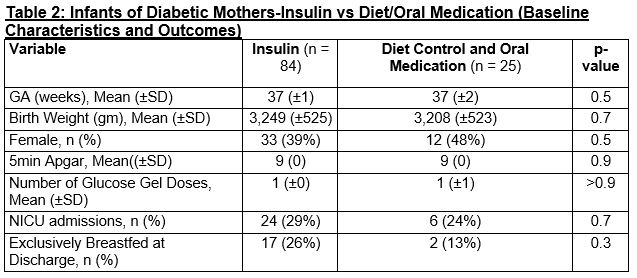
Table 1. SGA vs LGA (Baseline characteristics and outcomes)
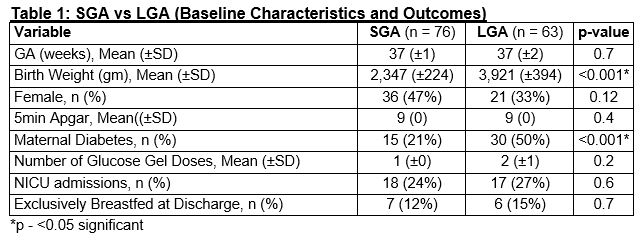
Table 2. Infants of Diabetic Mothers- Insulin vs Diet/Oral Medication (Baseline Characteristics and Outcomes)