Breastfeeding/Human Milk 1
Session: Breastfeeding/Human Milk 1
638 - Investigating the Impact of Health Disparities on the Provision of Parent’s Own Milk in a Level IV NICU
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 638.5270
Kathryn Devadoss, University of Washington School of Medicine, Seattle, WA, United States; Katie M. Strobel, University of Washington School of Medicine, Seattle, WA, United States; D. Taylor Hendrixson, University of Washington School of Medicine, Seattle, WA, United States
- KD
Kathryn Devadoss
Medical Student
University of Washington School of Medicine
Seattle, Washington, United States
Presenting Author(s)
Background: The provision of parent’s own milk (POM) to infants in the neonatal intensive care unit (NICU) decreases their risk of rehospitalization, mortality, and various morbidities. POM composition is customized to meet the infant’s needs. However, there are numerous disparities involved in the provision of POM to NICU patients for a variety of economic and logistical reasons.
Objective: We aimed to identify disparities that impact the provision of POM to infants during their level IV NICU hospitalization and by discharge.
Design/Methods: This was an observational, retrospective cohort study. Infants admitted to the Seattle Children’s NICU within their first week of life for at least two weeks from January 2020 to December 2023 were included in the study. Information on birthing parent demographics, home zip code, parent insurance status at NICU admission, infant feeding type (POM, donor milk, formula) given weekly, and markers of severity of infant illness were collected. Median household incomes by zip code were determined using US Census data. LASSO and stepwise variable selection were performed to select the models. Multivariable linear and logistic regression modeling were performed. Models were adjusted for gestational age, total antibiotic days, median household income, parent insurance status, and bronchopulmonary dysplasia.
Results: The cohort included 134 infants (Table 1). 46% of parents had Medicaid insurance and 52% of parents had private insurance on admission. Parent Medicaid insurance is negatively associated with the total percentage of POM received during NICU hospitalization (estimate: –16.7, 95% CI [–33.4, -0.11], p=0.048) (Table 2). Parent Medicaid was associated with decreased unadjusted odds of provision of exclusive POM at NICU discharge (OR 0.40[0.19, 0.84], p=0.0164) and adjusted odds (OR 0.36[0.15, 0.86], p=0.0318) (Figure 1). Additionally, parent Medicaid insurance was associated with decreased unadjusted odds of providing any POM by NICU discharge (OR 0.20[0.07, 0.52], p=0.0011) and adjusted odds (OR 0.21[0.07, 0.58] p=0.0077) (Figure 1).
Conclusion(s): Parent Medicaid insurance was negatively associated with total percentage of POM received during NICU hospitalization and by NICU discharge at a level IV NICU. Given the protective benefits of human milk use, strategies should be developed to address disparities in POM provision in the NICU to improve outcomes for critically ill infants.
Table 1.
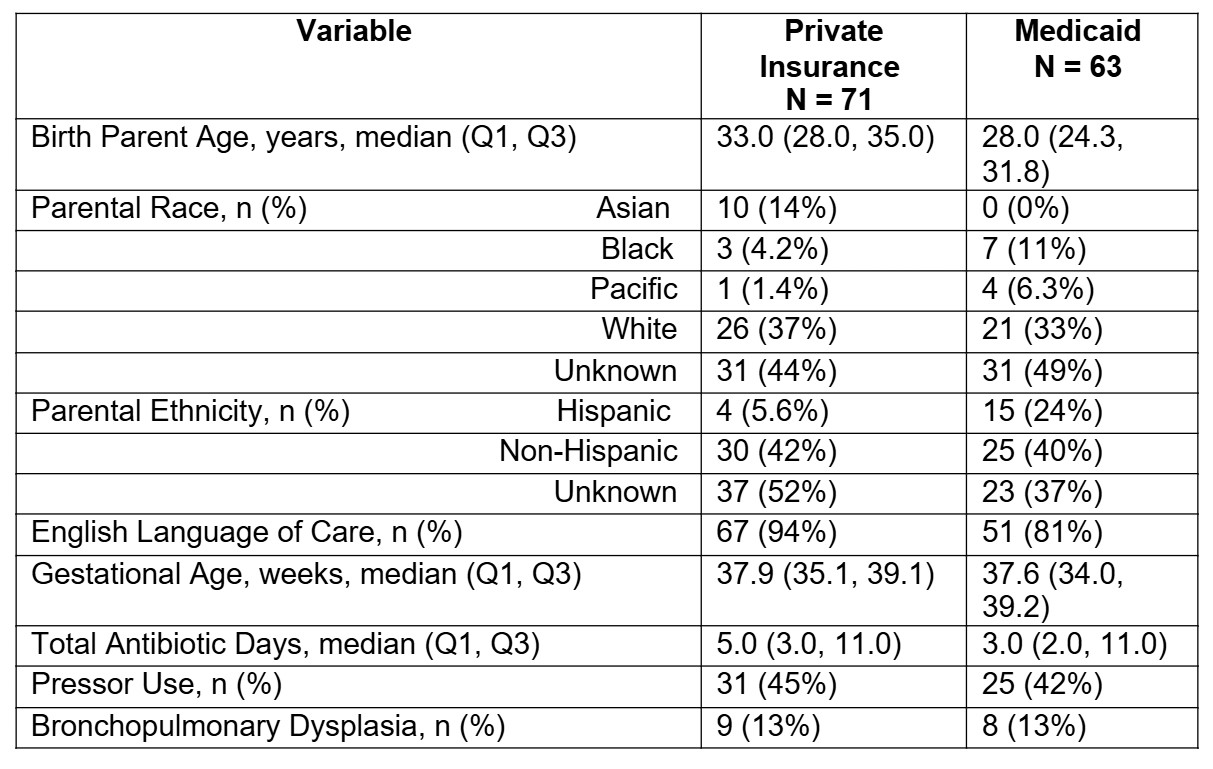 Cohort characteristics by parent insurance status on admission. Continuous variables are represented by median (IQR) and categorical variables by n (%). Bronchopulmonary dysplasia (BPD) was defined as a chronic lung disease that affects newborns, particularly those who are premature and require oxygen.
Cohort characteristics by parent insurance status on admission. Continuous variables are represented by median (IQR) and categorical variables by n (%). Bronchopulmonary dysplasia (BPD) was defined as a chronic lung disease that affects newborns, particularly those who are premature and require oxygen.Table 2.
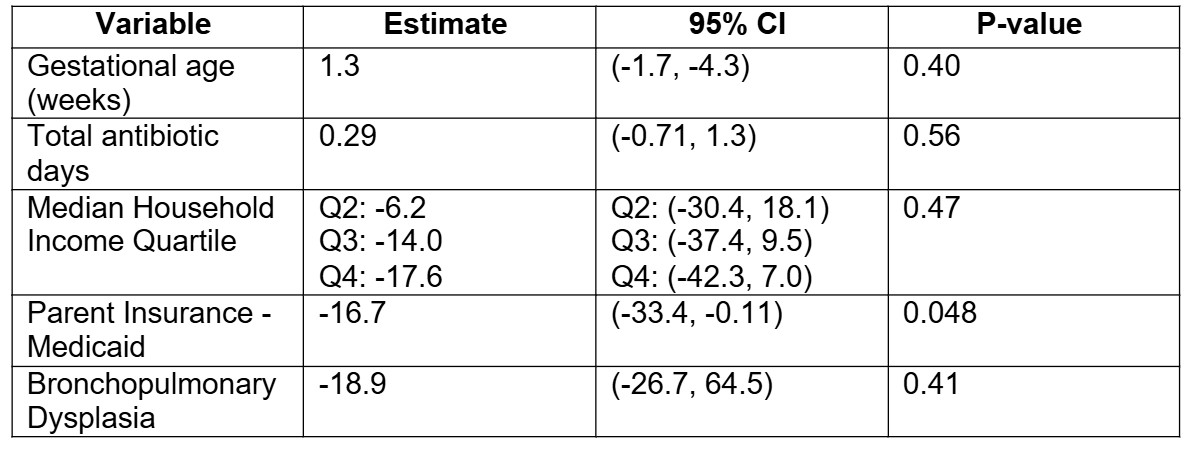 Multivariable linear regression model of total percentage of parent’s own milk during NICU hospitalization. Bronchopulmonary dysplasia (BPD) was defined as a chronic lung disease that affects newborns, particularly those who are premature and require oxygen. Median household income quartile was determined from zip code data obtained from the United States Census data.
Multivariable linear regression model of total percentage of parent’s own milk during NICU hospitalization. Bronchopulmonary dysplasia (BPD) was defined as a chronic lung disease that affects newborns, particularly those who are premature and require oxygen. Median household income quartile was determined from zip code data obtained from the United States Census data. Figure 1.
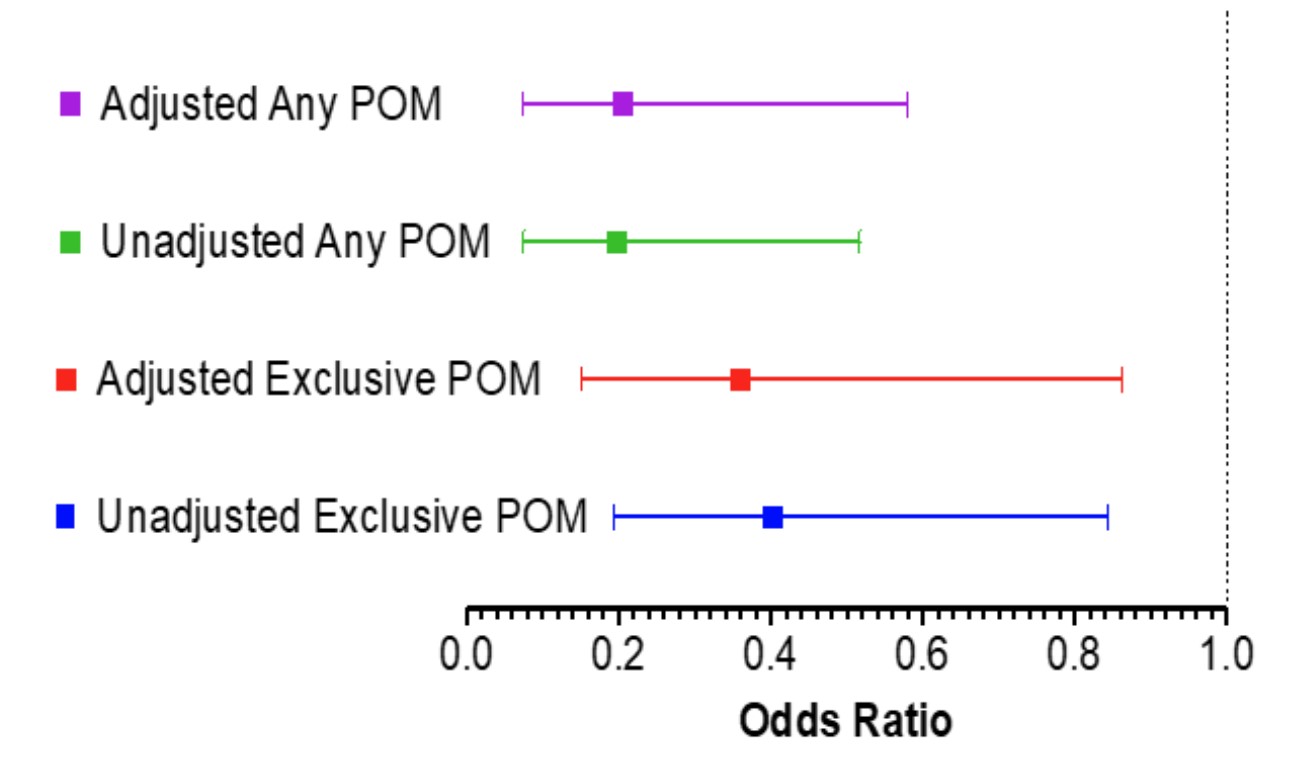 Forest plot of unadjusted and adjusted models of exclusive POM or any POM at NICU discharge. Models adjusted for gestational age, total antibiotic days, median household income, parent insurance status, and bronchopulmonary dysplasia.
Forest plot of unadjusted and adjusted models of exclusive POM or any POM at NICU discharge. Models adjusted for gestational age, total antibiotic days, median household income, parent insurance status, and bronchopulmonary dysplasia. 
