Infectious Diseases 3: Acute respiratory infections
Session: Infectious Diseases 3: Acute respiratory infections
126 - Estimating the Burden of RSV-Associated Hospitalization in Children by Capture-Recapture Analysis
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 126.4830
Tyler Stephen, University of Rochester School of Medicine and Dentistry, Rochester, NY, United States; Brenda Tesini, University of Rochester School of Medicine and Dentistry, Rochester, NY, United States; Kevin Popham, University of Rochester School of Medicine and Dentistry, Rochester, NY, United States; Wende Fregoe, University of Rochester School of Medicine and Dentistry, Rochester, NY, United States; Peter Szilagyi, UCLA, Los Angeles, California, CA, United States; Geoffrey A. Weinberg, University of Rochester School of Medicine and Dentistry, Rochester, NY, United States
- TS
Tyler Stephen, MD (he/him/his)
Fellow
University of Rochester School of Medicine and Dentistry
Rochester, New York, United States
Presenting Author(s)
Background: Respiratory syncytial virus (RSV) infection is a leading cause of pediatric hospitalization but measuring the burden is difficult due to limitations in surveillance platforms. Enrollment-based platforms may not enroll all cases and laboratory-based ones will miss cases without a clinician-ordered test. Capture-recapture methods combine data from multiple platforms to produce a more accurate burden estimate.
Objective: Estimate the burden of pediatric RSV-associated hospitalization using capture-recapture methods.
Design/Methods: We analyzed data from two population-based RSV surveillance networks in Monroe Co, NY: the New Vaccine Surveillance Network (NVSN) & the Respiratory Virus Hospitalization Surveillance Network (RESP-NET). NVSN actively enrolls children hospitalized with defined respiratory symptoms and performs research lab RSV PCR testing of nasal swabs from all enrollees. RESP-NET receives all clinician-ordered clinical lab PCR tests positive for RSV. The study included all county residents < 18 y of age hospitalized during Oct.-April of 2018-2020, and then all months Oct. 2020-Sept. 2023. We excluded nosocomial RSV infections & those admitted and discharged during weekends. We adjusted NVSN case estimates for non-enrollment of eligible screened patients. We matched cases from each surveillance system and performed capture-recapture analysis by the Petersen method. We calculated seasonal hospitalization rates using US Census data, with imputation of excluded weekend days.
Results: Pediatric RSV hospitalizations declined during the peak COVID-19 pandemic years and rose above pre-pandemic levels in 2022-23; each surveillance system detected these changes (Fig. 1). Hospitalization rates (per 100,000 children < 18 y of age per season) showed similar trends: 143 in 2018-19, 84 in 2020-21, and 250.4 in 2022-23 (Fig. 2). Each individual surveillance system captured similar proportions of the estimated true total of RSV cases, but neither did so completely. The proportion of all cases captured by RESP-NET appeared to be increasing over the study seasons (Fig. 3).
Conclusion(s): Neither NVSN nor RESP-NET surveillance platforms captured the full burden of RSV hospitalizations, but the proportions estimated by RESP-NET were increasing. This might be explained by changes in clinical testing practices over time (increased use of multiplex PCR panels containing RSV). Ongoing surveillance using multiple platforms remains important to understand the full burden of RSV hospitalization, especially given external factors such as new diagnostic practices, intervening pandemics, and new RSV preventive therapeutics.
Figure 1
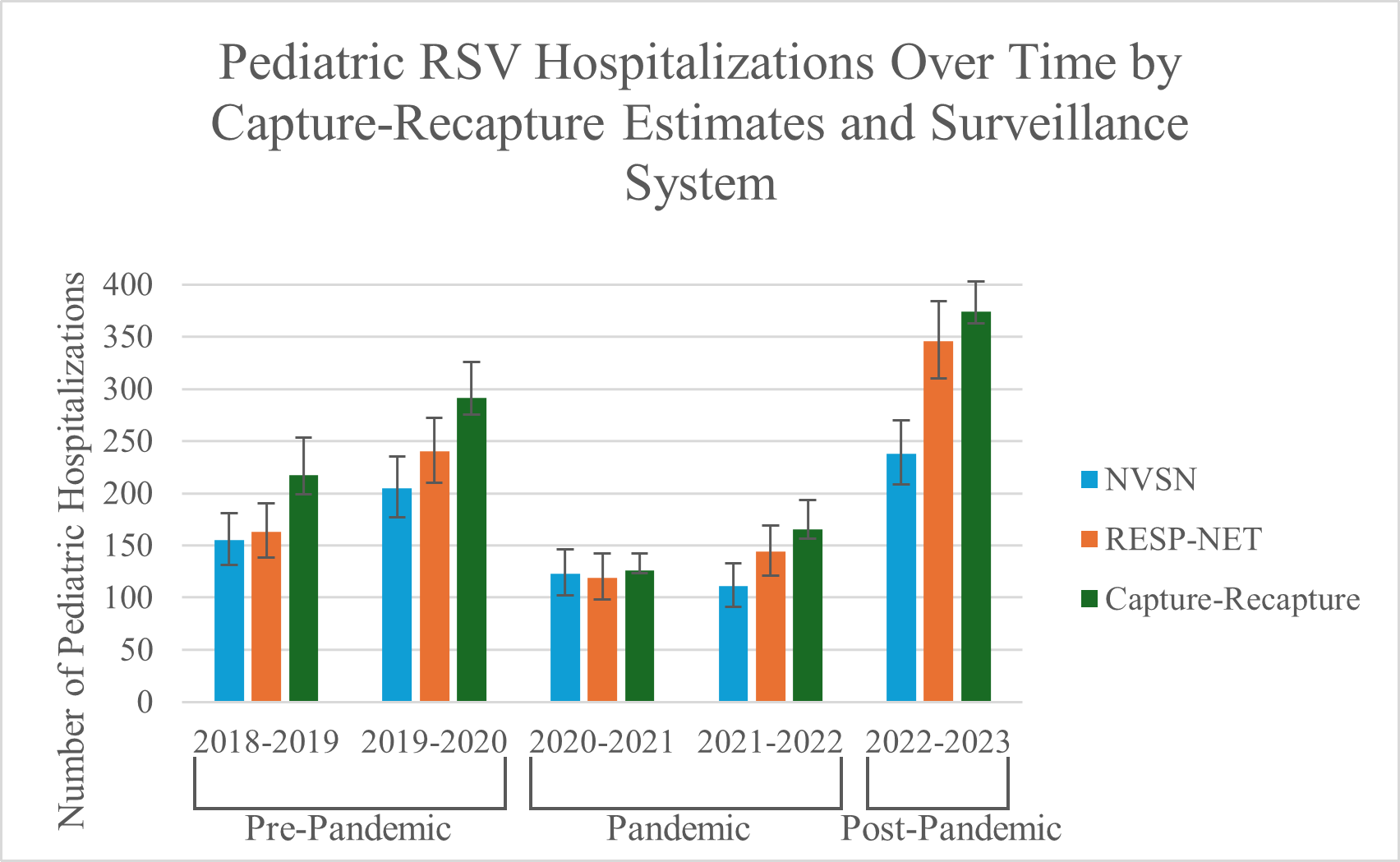 Pediatric RSV Hospitalizations Over Time by Capture-Recapture Estimates and Surveillance System
Pediatric RSV Hospitalizations Over Time by Capture-Recapture Estimates and Surveillance System Figure 2
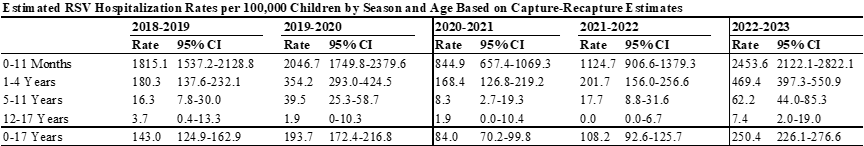 Estimated RSV Hospitalization Rates per 100,000 Children by Season and Age Based on Capture-Recapture Estimates
Estimated RSV Hospitalization Rates per 100,000 Children by Season and Age Based on Capture-Recapture EstimatesFigure 3
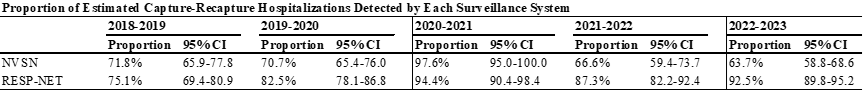 Proportion of Estimated Capture-Recapture Hospitalizations Detected by Each Surveillance System
Proportion of Estimated Capture-Recapture Hospitalizations Detected by Each Surveillance System
