Hospital Medicine 5: Clinical
Session: Hospital Medicine 5: Clinical
530 - Systemic Steroids in Children with BPD Hospitalized for Bronchiolitis: Beneficial or Harmful?
Sunday, April 27, 2025
8:30am - 10:45am HST
Publication Number: 530.6612
Naseem Alammar, University of Texas Southwestern & Children's Health, Dallas, TX, United States; Matthew Hall, Children's Hospital Association, Lenexa, KS, United States; Vishal Kapadia, University of Texas Southwestern Medical School, Dallas, TX, United States; Jenny Bohorquez, University of Texas Southwestern/Children's Health Dallas, Dallas, TX, United States; Vineeta Mittal, UTSW & Childrens Health, Dallas, TX, United States

Naseem Alammar, MD
Pediatric Hospital Medicine Fellow
University of Texas Southwestern & Children's Health
Dallas, Texas, United States
Presenting Author(s)
Background: The evidence against the use of systemic steroids in management of bronchiolitis in healthy children is well established. However, for children with bronchiolitis in the setting of bronchopulmonary dysplasia (BPD), the role of systemic steroids is less understood and remains unclear.
Objective: To study current practice and outcomes associated with systemic steroid use in premature children with BPD hospitalized for acute bronchiolitis.
Design/Methods: This was a retrospective study using the Pediatric Health Information System database. Children less than 2 years old with a history of prematurity ( < 32 weeks gestational age) and BPD (documented on a prior hospitalization) who were admitted to the general pediatric ward from 2012-2023 with a primary diagnosis of bronchiolitis were included. Secondary diagnoses that would require systemic steroid use (such as croup) or that further affected respiratory status were excluded. Outcomes included length of stay (LOS), readmission rate, ICU use, maximum respiratory support, and time on oxygen. These outcomes were compared between children who received systemic steroids vs. children who did not, using bivariate and multivariable analysis. Sensitivity analysis was done as well to correct for steroid timing in relation to ICU utilization.
Results: Of the 1,239 children who met the study criteria, 35% received systemic steroids (Table 1). Steroid use ranged from 0% to 75% across hospitals (p <.001; Figure 1). Systemic steroid use was associated with older age and home inhaled corticosteroid (ICS) use, but there was no significant difference by gestational age, birth weight, BPD severity, or home oxygen use (Table 1). In bivariate analysis, systemic steroids were associated with a significantly longer LOS, higher ICU use, higher invasive ventilation use, and more time on oxygen (data not shown). However, after multivariable and sensitivity analysis, steroid use only remained associated with longer LOS (2.8 vs. 2.2 days, p<.001) and more time on oxygen (2.7 vs. 2.3 days, p=0.012) (Table 2).
Conclusion(s): Significant variation exists in systemic steroid use for management of children with BPD and bronchiolitis. Systemic steroids were not associated with any improved outcomes and instead were significantly associated with a longer LOS and more time on oxygen. This highlights a need for further investigation into the role of systemic steroids in bronchiolitis and BPD.
Variation in Systemic Steroid Use
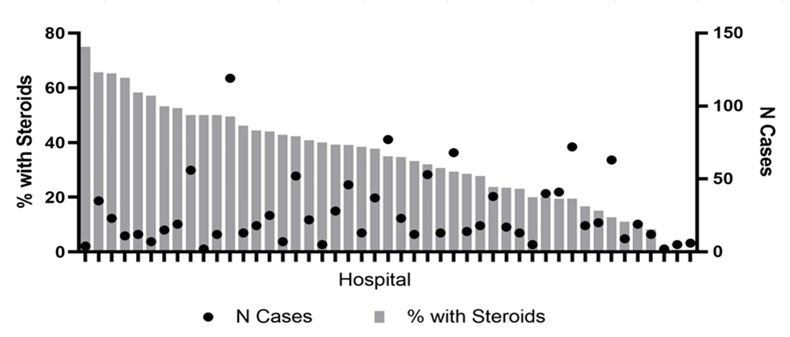 Figure 1. Rates of Systemic Steroid Use By Hospital
Figure 1. Rates of Systemic Steroid Use By HospitalCurrent Practice
.png) Table 1. Sociodemographic and Clinical Characteristics by Systemic Steroid Use
Table 1. Sociodemographic and Clinical Characteristics by Systemic Steroid Use Outcomes
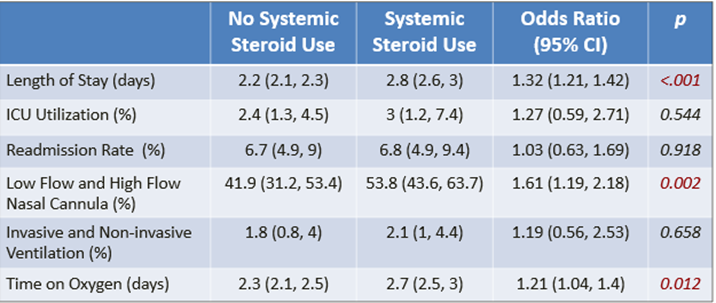 Table 2. Adjusted Outcomes by Systemic Steroid Use
Table 2. Adjusted Outcomes by Systemic Steroid UseVariation in Systemic Steroid Use
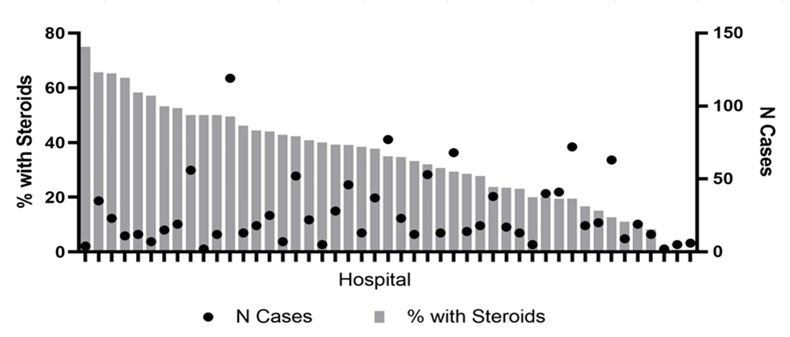 Figure 1. Rates of Systemic Steroid Use By Hospital
Figure 1. Rates of Systemic Steroid Use By HospitalCurrent Practice
.png) Table 1. Sociodemographic and Clinical Characteristics by Systemic Steroid Use
Table 1. Sociodemographic and Clinical Characteristics by Systemic Steroid Use Outcomes
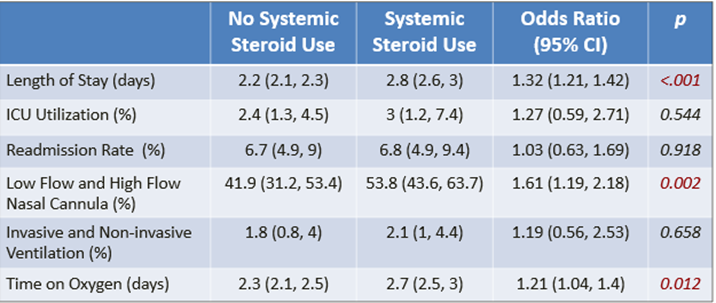 Table 2. Adjusted Outcomes by Systemic Steroid Use
Table 2. Adjusted Outcomes by Systemic Steroid Use
