Emergency Medicine 7
Session: Emergency Medicine 7
104 - The Impact of Respiratory Pathogen Panel Testing on Pediatric Emergency Department Return Visits and Management
Sunday, April 27, 2025
8:30am - 10:45am HST
Publication Number: 104.6598
Alexander M. Stephan, Weill Cornell Medicine, Brooklyn, NY, United States; Jaime Perez Lizardi, NewYork-Presbyterian Komansky Children’s Hospital, New York, NY, United States; Lana M. Stern, Weill Cornell Medicine, New york, NY, United States; Jennifer Jonas, Donald and Barbara Zucker School of Medicine at Hofstra/Northwell, New York, NY, United States; Charlene Thomas, Weill Cornell Medicine, New York, NY, United States; Nicole Gerber, NewYork-Presbyterian Komansky Children’s Hospital, New York, NY, United States; Karen Acker, Weill Cornell Medicine, New York, NY, United States; Deborah A. Levine, Weill Cornell Medical College - New York, NY, Port Washington, NY, United States
Alexander M. Stephan, MD (he/him/his)
Assistant Professor of Clinical Emergency Medicine / Assistant Professor of Clinical Pediatrics
Weill Cornell Medicine
Brooklyn, New York, United States
Presenting Author(s)
Background: In 2022, the AAP’s Choosing Wisely initiative recommended that physicians forego routine comprehensive respiratory pathogen panel (RPP) testing in children with a clinically diagnosed viral illness due to lack of impact on patient management or outcomes. An updated study of the impact of RPP testing on healthcare resource utilization in the pediatric emergency department (PED) is needed, as the scientific literature supporting this guideline pre-dates the COVID-19 pandemic.
Objective: To determine whether limited vs comprehensive RPP testing in patients with a clinically diagnosed viral illness affects 1) PED return visits and 2) subsequent patient management.
Design/Methods: We conducted a retrospective chart review of children aged >60 days to 18 years who were discharged from New York Presbyterian-Weill Cornell PED between Jun 1, 2023 – Aug 31, 2023, and Dec 1, 2023 – Feb 29, 2024, and received RPP testing for a clinically diagnosed viral illness. Subjects were classified as having received limited (COVID-19, influenza A/B, and respiratory syncytial virus) or comprehensive (21 pathogens) RPP testing. We recorded patient demographics, Emergency Severity Index (ESI) assignments, 7-day PED returns, and any additional interventions conducted at patients’ return visits. Analyses included univariate tests of association and multivariable logistic regression modelling.
Results: 2,346 patients met study inclusion criteria; 1,417 (60.4%) received limited RPP testing and 929 (39.6%) received comprehensive RPP testing (Table 1). No difference was found in 7-day PED return visit rate based on the type of RPP testing performed at patients’ initial visit (limited = 6.2% vs comprehensive = 6.7%; p = 0.7). No difference was found in 7-day PED return visit rate for limited testing compared to comprehensive testing after controlling for age, sex, race/ethnicity, insurance, ESI level, and visit season (summer vs winter) (OR 0.96, 95% CI 0.67-1.37; Table 2). On return visits, patients who had received limited RPP testing were more likely to undergo additional urine studies (limited = 28% vs comprehensive = 15%; p = 0.045); no differences were found in additional blood tests, throat swabs, chest x-rays, IV placement, medication administration, antibiotic prescribing, or disposition (Table 3).
Conclusion(s): Limited RPP testing may be sufficient to perform for children with a clinically diagnosed viral illness in the PED, as comprehensive RPP testing confers no benefit in reducing 7-day return visits and has limited impact on subsequent patient management.
Table 1: Patient Demographics
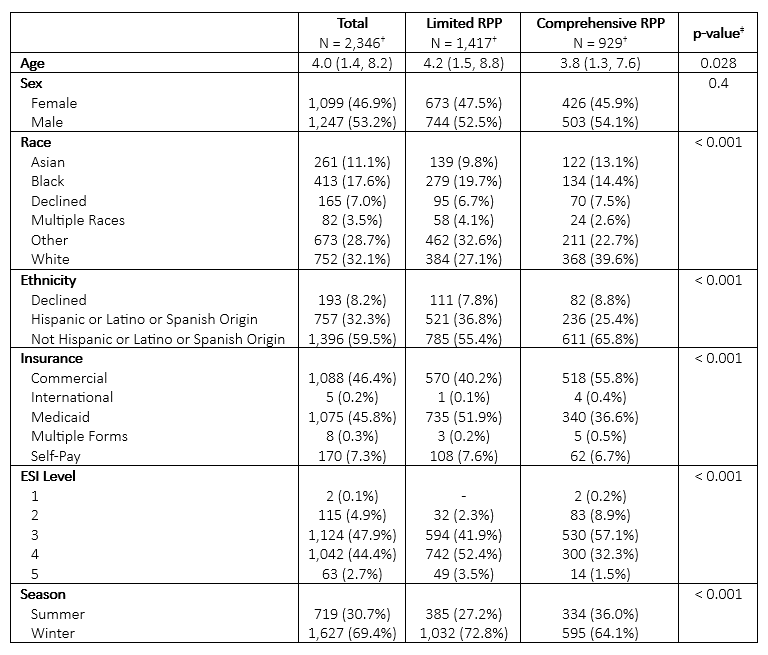 †Median (IQR); n (%)
†Median (IQR); n (%)‡Wilcoxon rank sum test; Pearson’s Chi-squared test; Fisher’s exact test
Table 2: Multivariable Logistic Regression Model for 7-Day PED Returns
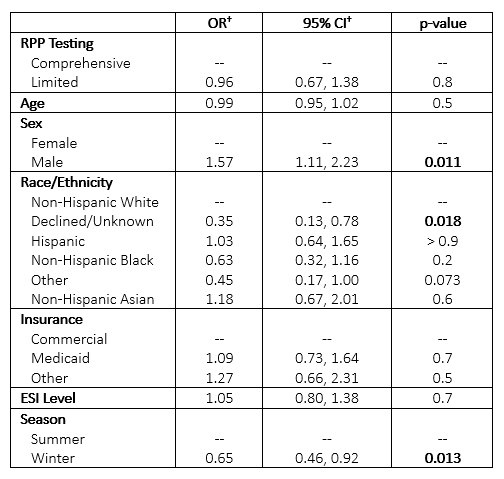 †OR = Odds Ratio, CI = Confidence Interval
†OR = Odds Ratio, CI = Confidence IntervalTable 3: Return Visit Management
 †n (%)
†n (%)‡Pearson’s Chi-squared test; Fisher’s exact test
Table 1: Patient Demographics
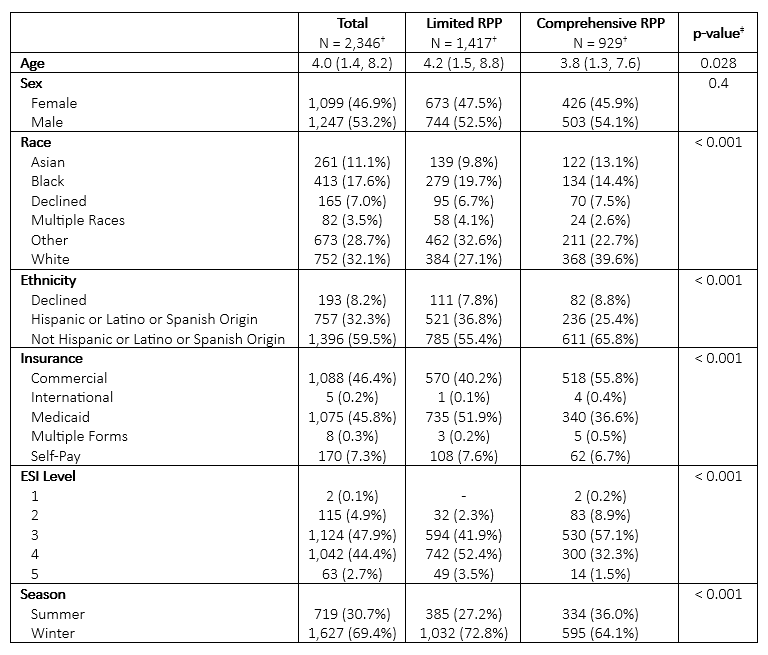 †Median (IQR); n (%)
†Median (IQR); n (%)‡Wilcoxon rank sum test; Pearson’s Chi-squared test; Fisher’s exact test
Table 2: Multivariable Logistic Regression Model for 7-Day PED Returns
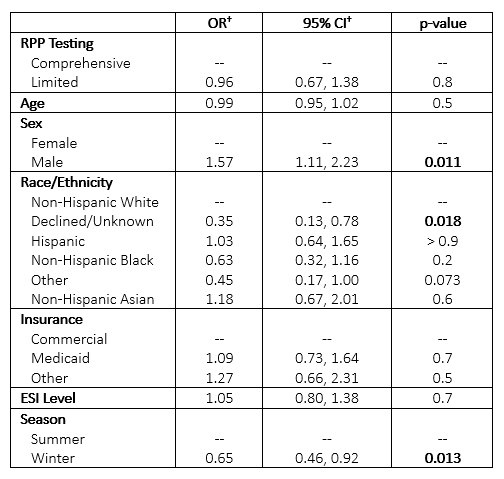 †OR = Odds Ratio, CI = Confidence Interval
†OR = Odds Ratio, CI = Confidence IntervalTable 3: Return Visit Management
 †n (%)
†n (%)‡Pearson’s Chi-squared test; Fisher’s exact test

