Emergency Medicine 8
Session: Emergency Medicine 8
119 - Practice Variation in Clinical Management of Simple and Complex Febrile Seizures at a Children’s Hospital: A Retrospective Study
Sunday, April 27, 2025
8:30am - 10:45am HST
Publication Number: 119.6198
Katherine Genet, Akron Children's Hospital, Akron, OH, United States; Pelletier Jonathan, Akron Children's Hospital, Akron, OH, United States; Karen C. Willis, Akron Children's Hospital, Akron, OH, United States; Sarah Kline-Krammes, Akron Children's Hospital, Akron, OH, United States

Katherine R. Genet, MD
Pediatric Emergency Medicine Fellow
Akron Children's Hospital
Akron, Ohio, United States
Presenting Author(s)
Background: Febrile seizures (FS) are the most common cause of seizures in patients under 5- years-old. FS are categorized as simple (SFS) or complex (CFS) based on duration, focality, and recurrence. An AAP guideline is available for management of SFS, but not CFS.
Objective: To identify practice variation in the clinical management of FS at a tertiary children’s hospital and the clinical impact of excess variation as targets for improvement.
Design/Methods: Single-center retrospective study of ED visits between 1/1/2020–12/31/2022 for children 6-60 months of age with an index diagnosis of FS. Children with pre-existing complex diseases, intracranial shunts, metabolic derangements, toxic ingestions, or trauma were excluded. Patients were classified as SFS or CFS.
Patients with CFS were further classified as “low-risk” if they had two generalized seizures within 24 hours and a non-focal neurologic examination. Patients with 3 or more seizures within 24 hours or focality were classified as “high-risk.” The cohort was subdivided according to seizure type and described with summary statistics.
Results: There were 513 encounters. Median age was 19-months, 59% males. In total, 77% were SFS, 9% were low-risk CFS, and 14% were high-risk CFS (figure 1). Table 1 provides data on the medical procedures and encounter cost for patients with all FS, SFS, low-risk CFS, and high-risk CFS.
The data shows a trend where the suspected severity of the illness is associated with increased usage of medical procedures and higher encounter costs (SFS < low-risk CFS < high-risk CFS). Neuroimaging use rises from 1% in SFS to 45% in high-risk CFS (figure 2). Of the high-risk CFS patients who had neuroimaging, 2/33 (6%) showed meningeal enhancement. No structural lesions were identified.
EEG use rises from 1% in SFS to 41% in high-risk CFS. Admission rates increase from 5% in SFS to 66% in high-risk CFS. Of all LPs, one patient had CSF pleocytosis, and no bacterial meningitis was identified.
The median cost of the encounter rises sharply. The interquartile range for encounter costs widens for both types of CFS, suggesting greater variability in cost.
Conclusion(s): This single-center retrospective study demonstrated considerable practice variation in the management of FS. Patients with CFS incur more intensive medical resource usage, higher admission rates and costs compared to those with SFS. Limiting neuroimaging and LPs to patients with high-risk CFS would have substantially reduced testing without missing any cases with abnormal results. Implementation of an institution-specific guideline may decrease variation in the management of FS.
Figure 1
.jpg) Total patient encounters with type of febrile seizure, neurologic exam, and the subsequent neuroimaging (if obtained).
Total patient encounters with type of febrile seizure, neurologic exam, and the subsequent neuroimaging (if obtained).Table 1
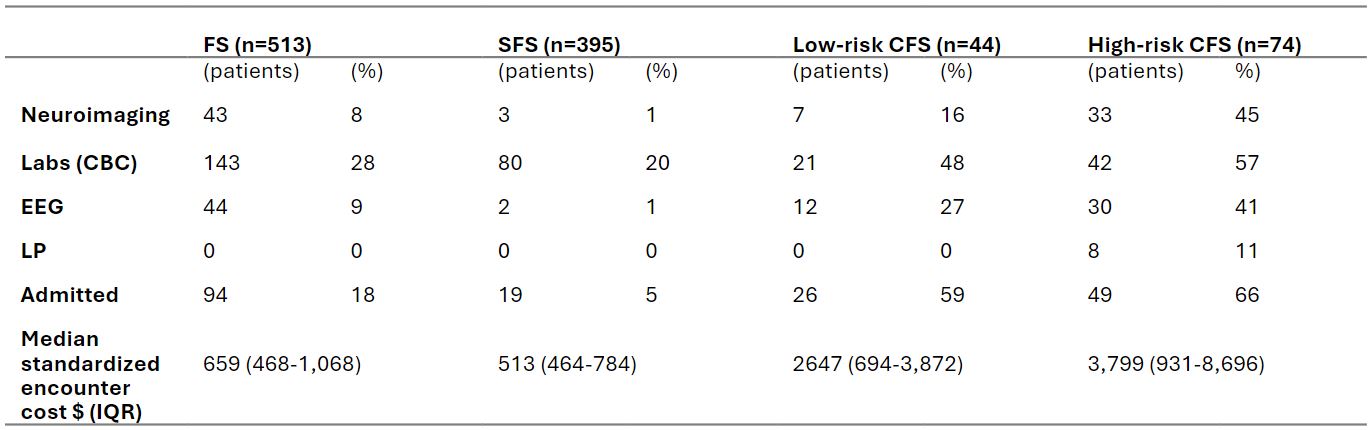 Number of patients to have neuroimaging, labs (CBC), EEGs, LP, admitted to the hospital, and median encounter cost of total FS, SFS, low-risk CFS, and high-risk CFS.
Number of patients to have neuroimaging, labs (CBC), EEGs, LP, admitted to the hospital, and median encounter cost of total FS, SFS, low-risk CFS, and high-risk CFS.Figure 2
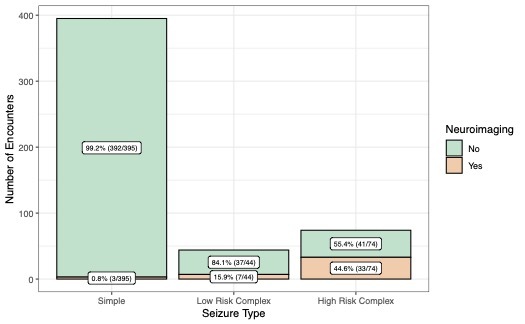 Number of encounters representing patients who had neuroimaging obtained classified by type of febrile seizure.
Number of encounters representing patients who had neuroimaging obtained classified by type of febrile seizure. 
