Emergency Medicine 7
Session: Emergency Medicine 7
101 - Predictors of Bronchodilator Therapy in Bronchiolitis in Pediatric Emergency Care: a Multicenter PEDSnet Study
Sunday, April 27, 2025
8:30am - 10:45am HST
Publication Number: 101.6183
Andrea Rivera-Sepulveda, Nemours Children's Health, ORLANDO, FL, United States; Timothy Maul, Nemours Children's Hospital, Orlando, FL, United States; Cara Reedy, Nemours Children's Hospital, Troy, NY, United States; Matthew M. Davis, Nemours Children's Hospital, Wilmington, DE, United States; Todd A. Florin, Ann & Robert H. Lurie Children's Hospital of Chicago, Chicago, IL, United States; Kathryn Blake, Nemours Children's Health, Jacksonville, FL, United States; Kenneth A. Alexander, The University of Central Florida, Orlando, FL, United States

Andrea Rivera-Sepulveda, MD, MSc
Associate Professor
Nemours Children's Health
ORLANDO, Florida, United States
Presenting Author(s)
Background: Although guidelines advise against routine bronchodilator use in bronchiolitis, practices vary across U.S. pediatric emergency departments (EDs). This variability may arise from differing institutional protocols, provider preferences, inconsistent adherence to guidelines, and patient demographics and clinical characteristics across regions that may influence treatment decisions.
Objective: To evaluate demographic, clinical, and outcome factors associated with bronchodilator use in bronchiolitis across multiple U.S. sites, and develop a predictive model to identify children more likely to receive bronchodilator treatment in the ED.
Design/Methods: This multicenter, retrospective, cross-sectional study analyzed data from PEDSnet, covering nine large academic medical centers (January 1, 2019, to December 31, 2019). Children aged 3 to 24 months with bronchiolitis were included; those with comorbidities were excluded. Data included demographics, clinical variables, diagnostics, therapeutics, and disposition. Comparisons in demographics, clinical, and site characteristics were analyzed using Cramer’s V chi-square and one-way ANOVA, as appropriate. A random forest model was developed to predict bronchodilator use, with two-thirds of the data for training and one-third for testing, targeting an 80% accuracy.
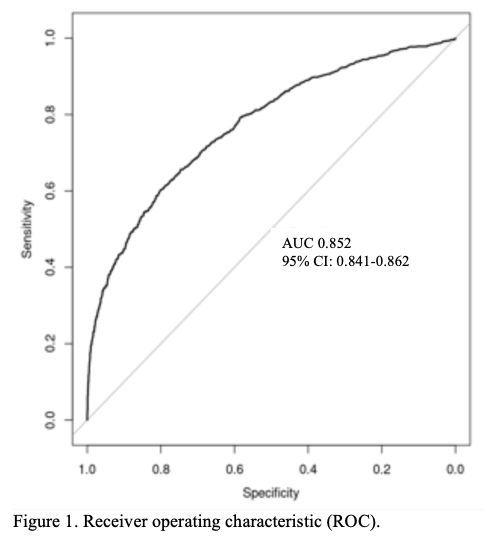
Results: We identified 14,213 encounters involving 12,158 unique patients. Demographics, including age, race, ethnicity, language, and insurance type, varied significantly across sites (p < 0.001), while sex did not. Significant site-specific differences were observed in clinical variables such as bronchodilator, steroid, and radiograph use, as well as length of stay (p < 0.001). Bronchodilator use correlated with factors including sex, insurance type, race, ethnicity, language, site, atopic dermatitis, wheezing, and history of pneumonia (p < 0.01). Key predictors for bronchodilator use included steroid use, site, age, and respiratory rate, with the model achieving 85% accuracy (p < 0.001), 25% sensitivity, 98% specificity, 71% positive predictive value, and 86% negative predictive value.
Conclusion(s): The predictive model reveals significant variability in bronchiolitis management across nine children’s hospitals, highlighting the need to investigate geographic disparities in bronchiolitis care. Future research should explore a targeted treatment approach that considers regional patient demographics, comorbidities, and resources, potentially enhancing guideline adherence and allowing for personalized adjustments.
Receiver operating characteristic (ROC) curve.