Endocrinology 2
Session: Endocrinology 2
316 - Salty Squared: Two Cases of ROHHAD(NET) Presenting with Severe Hypernatremia
Sunday, April 27, 2025
8:30am - 10:45am HST
Publication Number: 316.6399
Rachel L. Palting, Oregon Health & Science University, Portland, OR, United States; Kara Connelly, Oregon Health & Science University School of Medicine, Portland, OR, United States; Lindsey nicol, OHSU, Portland, OR, United States

Rachel L. Palting, DO (she/her/hers)
Pediatric Endocrinology Fellow
Oregon Health & Science University
Portland, Oregon, United States
Presenting Author(s)
Background: ROHHADNET (rapid-onset obesity with hypoventilation, hypothalamic, autonomic dysregulation, and neuroendocrine tumor) is a rare and complex syndrome. Patients can present with a range of endocrinopathies, like diabetes insipidus.
Objective: To report two cases of ROHHADNET presenting with hypernatremia.
Design/Methods: A 5-year-old (patient 1) and a 3-year-old (patient 2) present with weight gain and hypernatremia.
Results: Patient 1 presented with 16.6 kg weight gain over two years without hyperphagia. Labs showed hypothyroidism, ACTH deficiency, and hyperprolactinemia, indicating hypothalamic dysfunction. Adipsic hypernatremia (160 mmol/L), high urine output, and low urine concentration indicated ADH deficiency. He initiated levothyroxine, hydrocortisone with stress dosing, and DDAVP with a fluid prescription. Daily fevers without infection suggested autonomic dysregulation. Brain MRI showed an incidental Rathke’s cleft cyst with normal pituitary signal; a follow-up MRI after seizure-like activity showed decreased brain volume. He developed hypercarbic respiratory failure and hypoventilation, managed initially with BiPAP, later escalated to average volume assured pressure support (AVAPS), but ultimately required tracheostomy for sustained ventilation. PHOX2B testing was negative. He gained 16 kg over five months and started dextroamphetamine-amphetamine for hypothalamic obesity, slowing weight gain to 6 kg over 13 months.
Patient 2 presented with severe hypernatremia (170 mmol/L) and an 8.9 kg weight gain over two years without hyperphagia. He was diagnosed with ADH deficiency due to adipsic hypernatremia and high urine output, and he was started on DDAVP and a fluid goal. Hypernatremia and difficult IV access led to altered mental status requiring ICU admission. A multidisciplinary discussion led to port placement, later removed due to MRSA bacteremia and a jugular thrombus, managed with antibiotics and anticoagulation. A peak cortisol of 14.5 µg/dl prompted stress-dose steroids and later maintenance hydrocortisone due to ACTH deficiency risk. He began CPAP for sleep apnea and underwent adenotonsillectomy. Initial CT showed a 2 cm adrenal mass, confirmed as ganglioneuroma post-resection. After gaining 13.2 kg over seven months, dextroamphetamine-amphetamine and lifestyle interventions slowed weight gain to 2 kg over three months.
Conclusion(s): The differential for rapid weight gain in children should include ROHHADNET. These cases highlight the range of interventions to manage this disorder. They underscore the need for multidisciplinary coordination and evidence-based guidelines for best treatment.
Labs at diagnosis.
.png) Both patients presented with hypernatremia and hyperprolactinemia. Patient 1 was diagnosed with hypothyroidism based on decreased Free T4 from prior and cortisol deficiency based on ACTH stimulation test.
Both patients presented with hypernatremia and hyperprolactinemia. Patient 1 was diagnosed with hypothyroidism based on decreased Free T4 from prior and cortisol deficiency based on ACTH stimulation test. Weight Chart for Patient 1
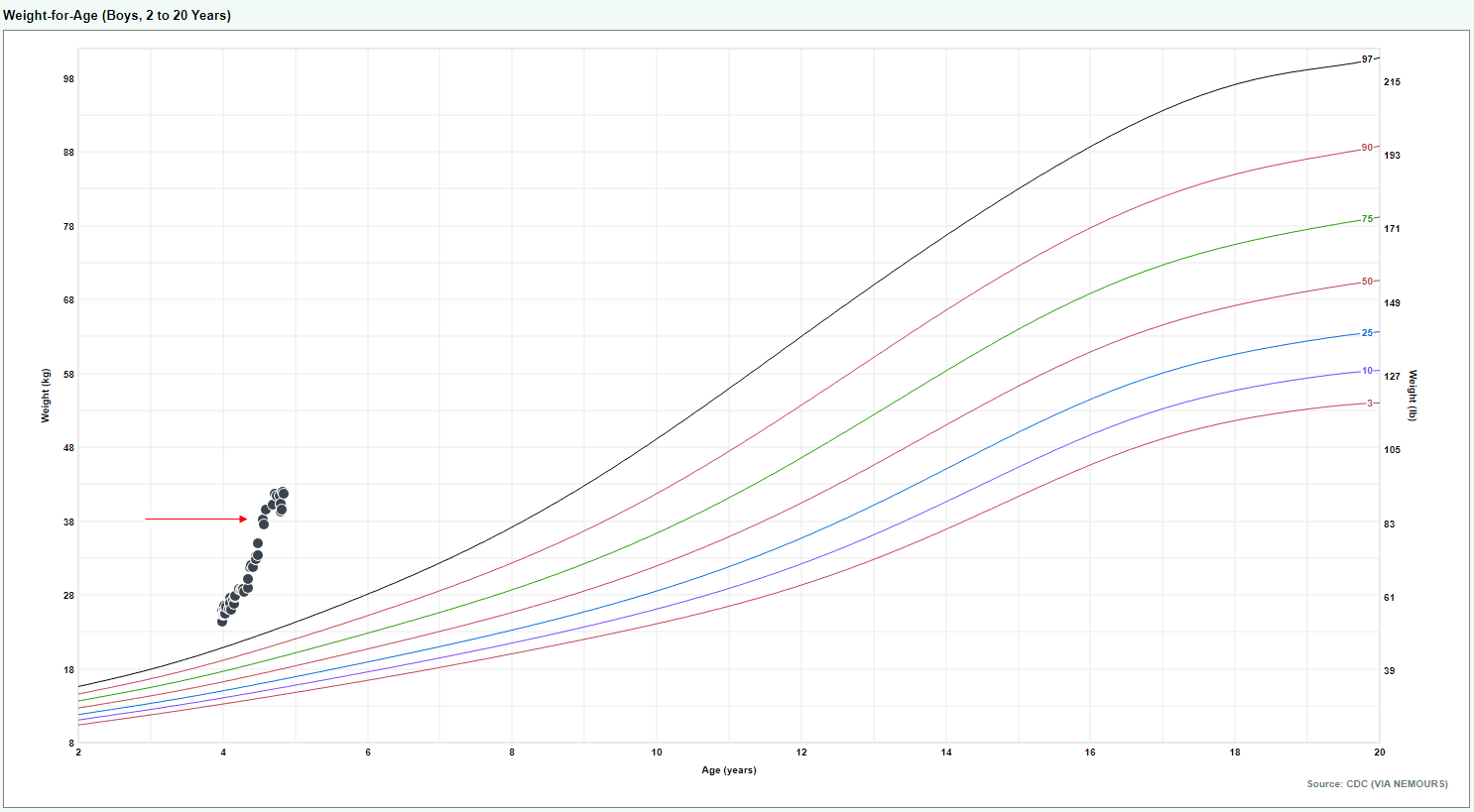
.png) Patient 1 had rapid increase in weight after diagnosis (16 kg over 5 months). Red arrow indicates initiation of dextroamphetamine-amphetamine. Rate of weight gain decreased after this intervention (6 kg over 13 months).
Patient 1 had rapid increase in weight after diagnosis (16 kg over 5 months). Red arrow indicates initiation of dextroamphetamine-amphetamine. Rate of weight gain decreased after this intervention (6 kg over 13 months).Weight Chart for Patient 2
 Patient 2 had rapid increase in weight after diagnosis (13.2 kg over 7 months). Red arrow indicates initiation of dextroamphetamine-amphetamine. Rate of weight gain decreased after this intervention (2 kg over 3 months).
Patient 2 had rapid increase in weight after diagnosis (13.2 kg over 7 months). Red arrow indicates initiation of dextroamphetamine-amphetamine. Rate of weight gain decreased after this intervention (2 kg over 3 months).
