Hospital Medicine 5: Clinical
Session: Hospital Medicine 5: Clinical
534 - What will others think of me? Drivers of Overuse by Pediatric Hospitalists
Sunday, April 27, 2025
8:30am - 10:45am HST
Publication Number: 534.7016
Lyubina Yankova, Yale-New Haven Children's Hospital, New Haven, CT, United States; Monisha Sachdev, University of Michigan Medical School, Ann Arbor, MI, United States; Nirali Butala, Boston Children's Hospital, Boston, MA, United States; Alexa Allotta, Yale-New Haven Children's Hospital, Staten Island, NY, United States; Rachel Osborn, Yale School of Medicine, New Haven, CT, United States; David N. Berg, Yale School of Medicine, New Haven, CT, United States; Jaspreet Loyal, Yale-New Haven Children's Hospital, Trumbull, CT, United States
- LY
Lyubina Yankova, MD (she/her/hers)
Pediatric Hospital Medicine Fellow
Yale-New Haven Children's Hospital
New Haven, Connecticut, United States
Presenting Author(s)
Background: Healthcare overuse in pediatrics costs an estimated 27 million dollars per year. Although evidence supports the safety of reducing certain practices (as indicated by Choosing Wisely recommendations), the reasons for overuse are not well understood.
Objective: To understand the perspectives of pediatric hospitalists on drivers of overuse.
Design/Methods: Using qualitative methodology, we conducted semi-structured interviews with pediatric hospitalists in 2 institutions in New England and the Midwest. Data was coded using the constant comparative method to elucidate themes. We applied the open systems theory levels of analysis framework from organizational psychology.
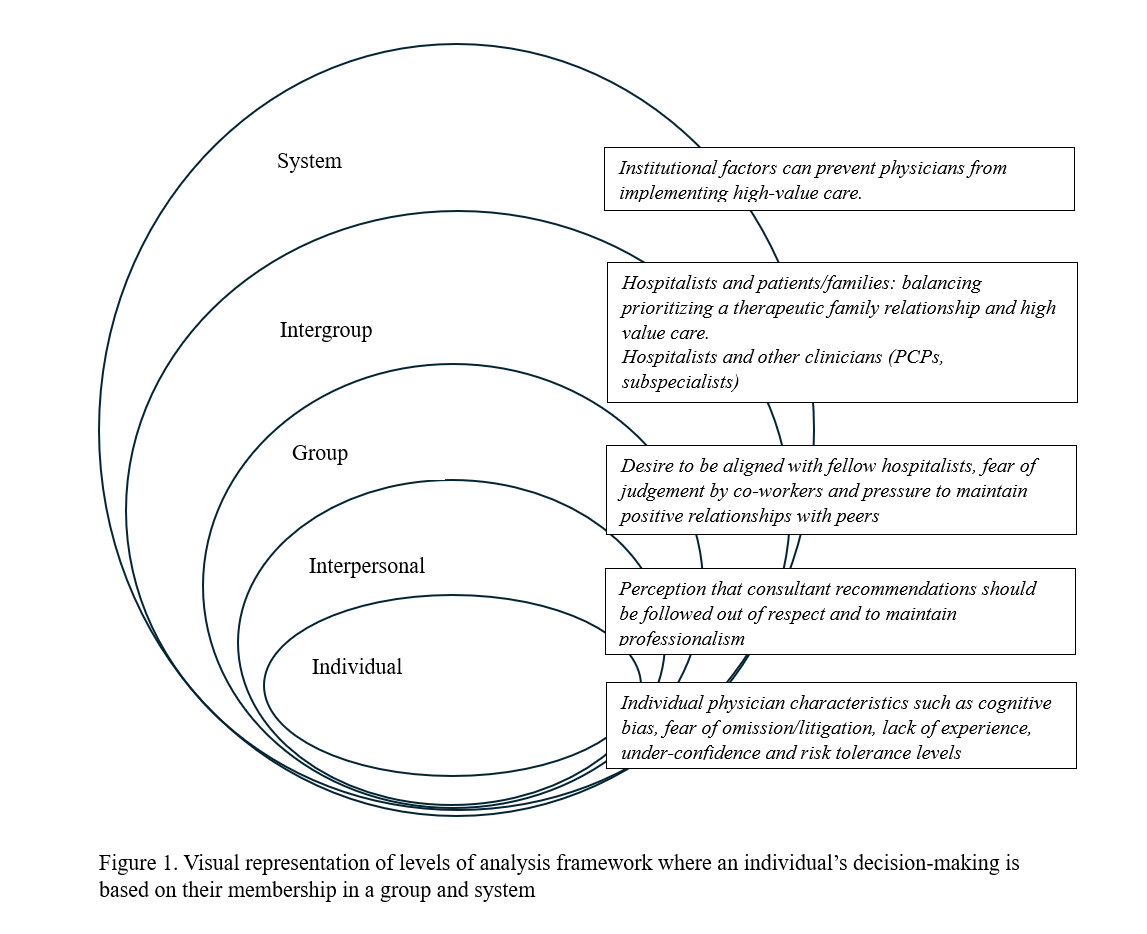
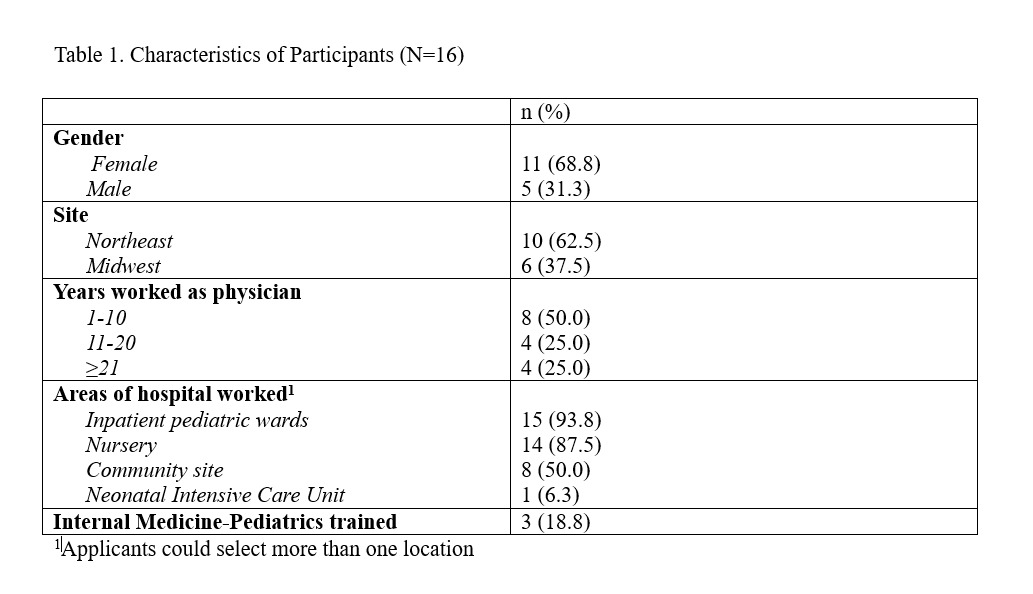
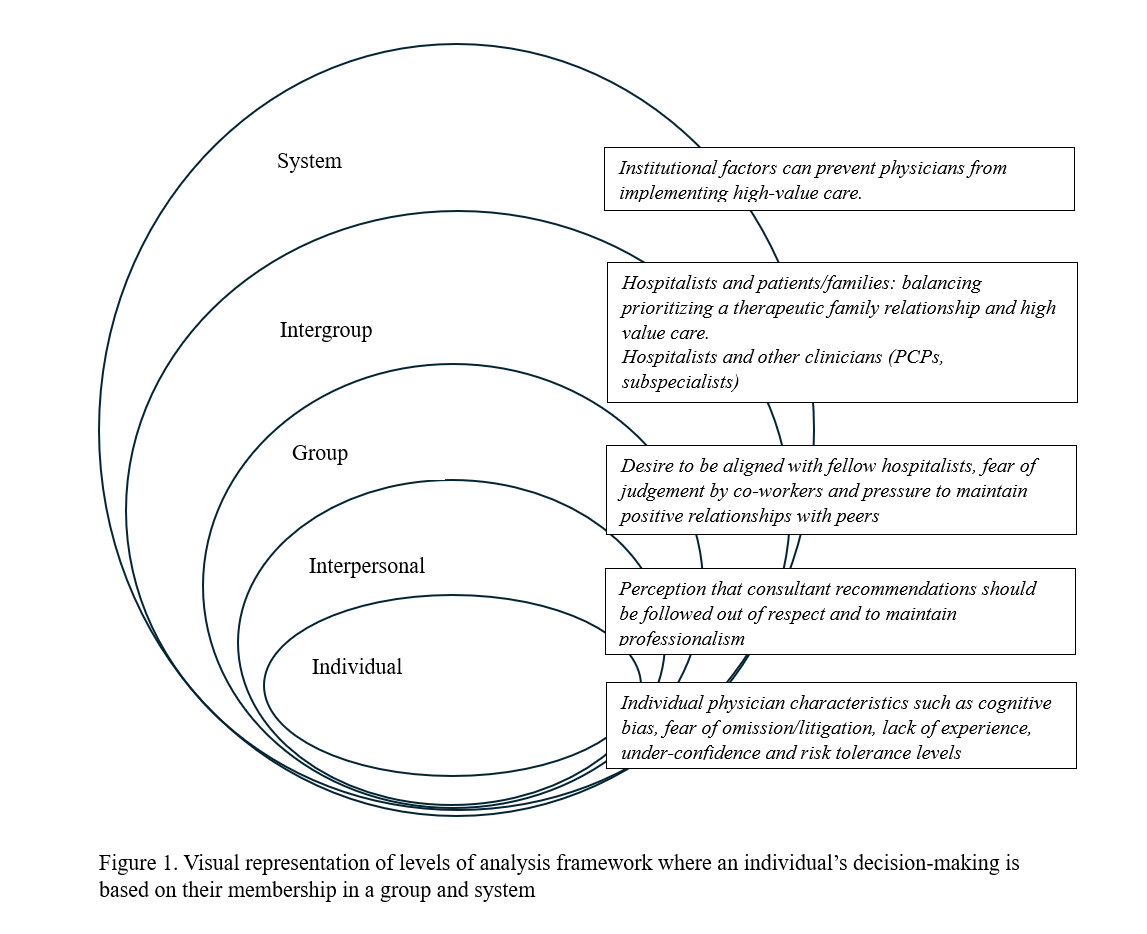
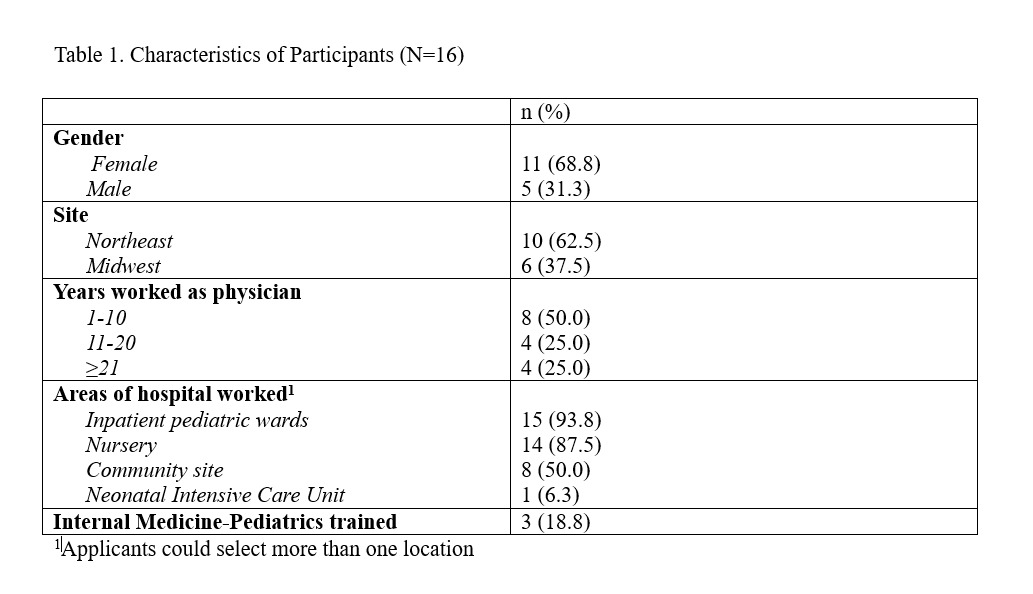
Results: We interviewed 16 pediatric hospitalists (Table 1). Applying the levels of analysis framework revealed individual, interpersonal, group, intergroup and system institutional factors contributing to overuse (Figure 1). 5 themes emerged:
1) Individual: Physician traits like cognitive bias, fear of omission or litigation, inexperience, lack of confidence, and risk tolerance. “It's the spirit of being wrong, fear of not being perfect, fear of missing something.”
2) Interpersonal: A perception that recommendations from consultants or primary care clinicians should be followed out of respect, professionalism, and to honor expertise. “I find it hard to not do those recommendations…I just find it pretty disrespectful…people are like, “Well, then why did you consult me if you’re not gonna follow what I say?”
3) Group: A desire to be aligned, fear of judgement and pressure to maintain positive relationships with peers. “I found that I was practicing differently, knowing who was coming on the next day…getting more blood work and more testing.”
4) Intergroup: The combination of inter-group dynamics (hospitalists and parents or other clinicians). “I'm pretty confrontation-averse, so that whole dynamic…I don't deal with well… The encounter might be over quickly but that, I would be thinking about for hours...It might be easier to not fight them.”
5) System institutional factors can prevent physicians from implementing high-value care due to competing priorities. “We do it because we don't have enough time to stop and think about what the right thing is to do.”
Conclusion(s): In this study, the individual pediatric hospitalist’s role and agency in contributing to overuse is a function of the group and system they belong to. Meaningful change to combat overuse needs to start from awareness of group dynamics within institutions and tailor efforts such as open communication, team-building and system fixes such as staffing to not overextend hospitalists.
Characteristics of participants (N=16)
Visual representation of levels of analysis framework where an individual's decision-making is based on their membership in a group or system
Characteristics of participants (N=16)
Visual representation of levels of analysis framework where an individual's decision-making is based on their membership in a group or system