Hospital Medicine 4: Medical Education
Session: Hospital Medicine 4: Medical Education
167 - Worried About What the Parents Will Say? Resident Led Rounding on the Hospital Medicine Service
Sunday, April 27, 2025
8:30am - 10:45am HST
Publication Number: 167.7020
Monisha Sachdev, University of Michigan Medical School, Ann Arbor, MI, United States; Simran Sinha, University of Michigan, Ann Arbor, MI, United States; Julie Sturza, University of Michigan Medical School, Ann Arbor, MI, United States; Jocelyn H. Schiller, C.S. Mott Children's Hospital, Ann Arbor, MI, United States; Jodi Ehrmann, University of Michigan Medical School, Ann Arbor, MI, United States

Monisha Sachdev, MD (she/her/hers)
Pediatric Hospital Medicine Fellow
University of Michigan Medical School
Ann Arbor, Michigan, United States
Presenting Author(s)
Background: Senior resident led rounds (SLRs) can help in the development of leadership skills by allowing for autonomy in a low-stakes environment. Research has shown improved resident satisfaction with SLRs without worse patient outcomes. However, there is no data on the experience of patients and families with SLRs. As the landscape of pediatric resident education changes, it is important to understand the patient and family experience of SLRs to understand the full impact of the practice.
Objective: Our goal was to describe the family experience of communication during SLRs on the hospital medicine service.
Design/Methods: Senior residents rounded without an attending present once per week on the hospital medicine service. Surveys assessing the quality of morning rounds with a 1 - 5 Likert scale (1 - worst, 5 - best) were administered to family members of patients. Survey content and wording was reviewed by representatives from our institution’s parent and family advisory committee. Length of rounding time, total number of patients and number of new patients seen, and which team member led rounds (attending or senior) was recorded by clinical assistants. Survey results, rounding times, total number of patients and number of new patients seen were compared on days with and without an attending present.
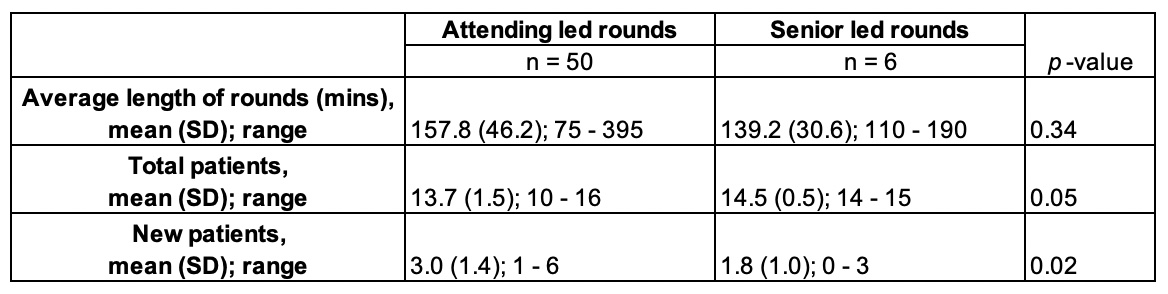
Results: Data was collected from April 2024 through October 2024 on days when attendings (n = 50) and senior residents (n = 6) led rounds. 127 parents were invited to participate; 100 surveys were completed (response rate 83%). The mean score for quality of SLRs (4.7) was not different from attending led rounds (4.5), where the acceptable margin of inferiority was 0.5 on the Likert scale (p < 0.0001) (Figure 1). Average length of rounds was not significantly different between groups (157.8 minutes for attending led rounds vs 139 minutes for resident led rounds, p = 0.34). Average number of patients rounded on was higher when seniors led rounds (14.5 vs 13.7, p = 0.02); however average number of new patients rounded on did not differ between groups (3.0 for attending led rounds vs 1.8 for resident led rounds, p= 0.05) (Figure 2).
Conclusion(s): Senior resident led rounds did not impact the quality of communication with patients and families or rounding time. Analysis of the number of patients seen and the length of rounding time demonstrates that SLRs is an efficient and effective rounding strategy even when hospital team census is high.
Figure 1: Mean score of quality of rounds when led by attendings vs senior residents
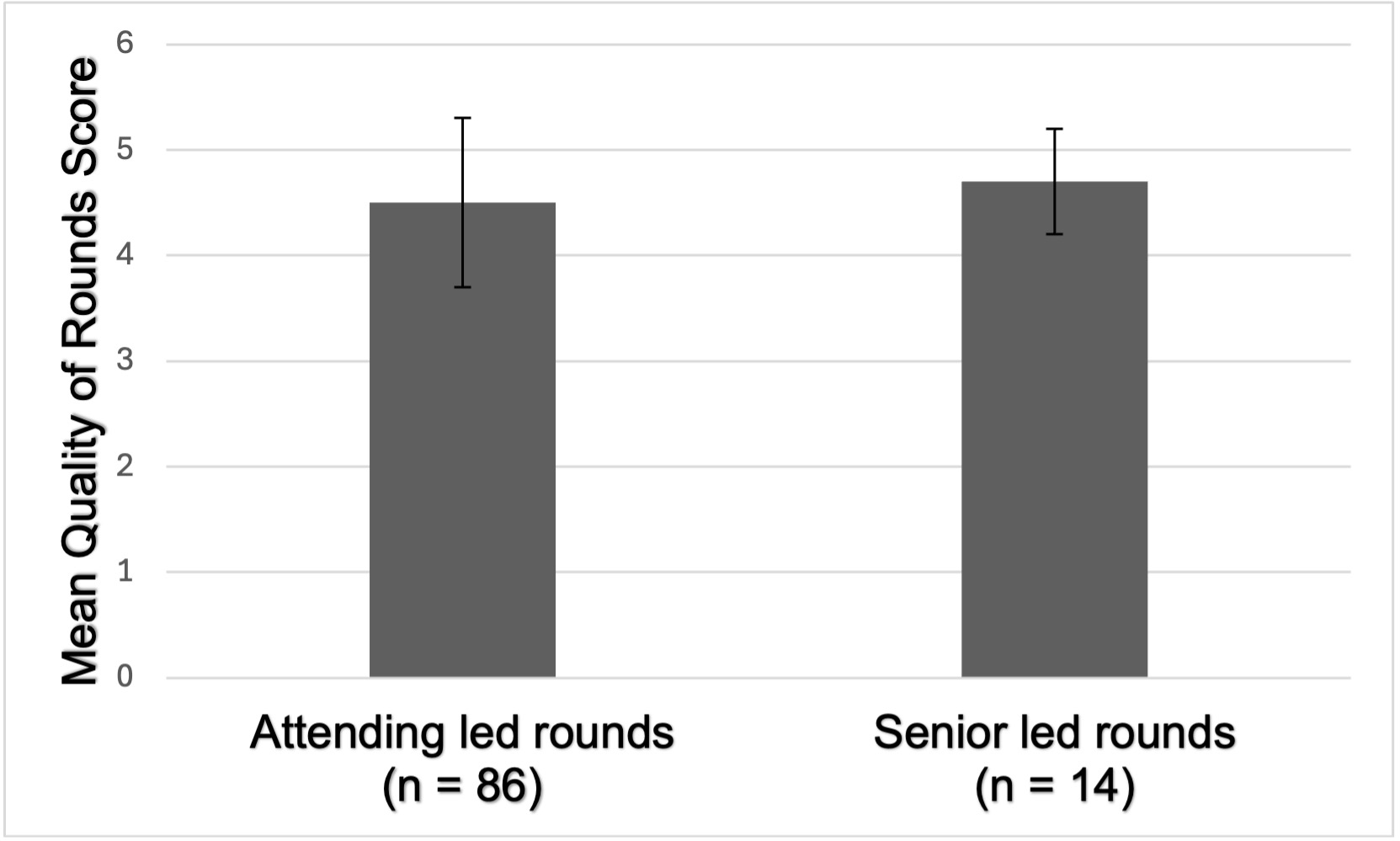
Figure 2: Average length of rounds and number of patients seen on rounds
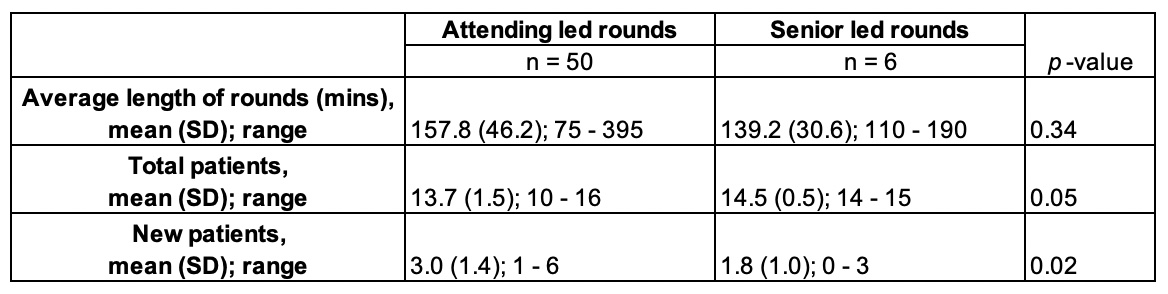
Figure 1: Mean score of quality of rounds when led by attendings vs senior residents
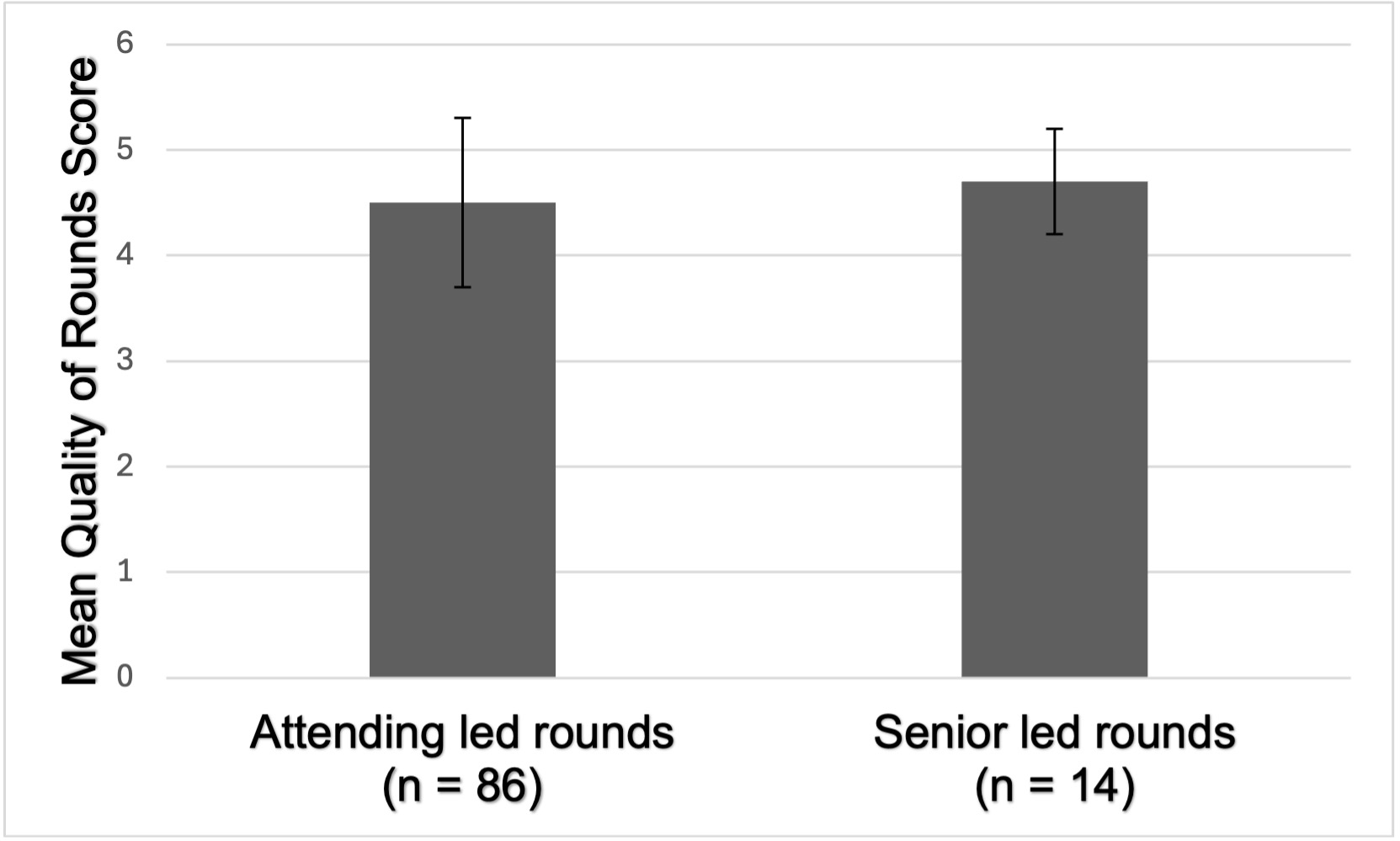
Figure 2: Average length of rounds and number of patients seen on rounds