Emergency Medicine 9
Session: Emergency Medicine 9
136 - Utilizing an Implementation Science Approach to Assess Barriers and Facilitators to Introducing the National Emergency Airway Registry (NEAR4PEM) Pre-Intubation Checklist
Sunday, April 27, 2025
8:30am - 10:45am HST
Publication Number: 136.7023
Robyn Wing, The Warren Alpert Medical School of Brown University, Wrentham, MA, United States; D Grace Smith, The Warren Alpert Medical School of Brown University, Princeton, NJ, United States; E. Ruby Cramer, The Warren Alpert Medical School of Brown University, Wellesley, MA, United States; Rochelle Rosen, Brown University Health, Providence, RI, United States; Hannah E. Frank, The Warren Alpert Medical School of Brown University, Providence, RI, United States; Ariana M. Albanese, The Warren Alpert Medical School of Brown University, Providence, RI, United States; Monica Prieto, Childrens Hospital of Philadelphia, Philadelphia, PA, United States; Emily Greenwald, Duke University School of Medicine, Chapel Hill, NC, United States; Joshua Nagler, Boston Children's Hospital, Boston, MA, United States; Michael P.. Goldman, Yale School of Medicine, New Haven, CT, United States; Kelsey A. Miller, Harvard Medical School, Boston, MA, United States; Benjamin Nti, Indiana University School of Medicine, Carmel, IN, United States; Natalie Napolitano, Children's Hospital of Philadelphia, Philadelphia, PA, United States; Akira Nishisaki, Childrens Hospital of Philadelphia, Philadelphia, PA, United States

Robyn Wing, MD, MPH (she/her/hers)
Associate Professor of Emergency Medicine & Pediatrics
The Warren Alpert Medical School of Brown University
Wrentham, Massachusetts, United States
Presenting Author(s)
Background: NEAR4PEM developed an evidence-based pre-intubation checklist, but translating this quality improvement tool into improved intubation outcomes in the Pediatric Emergency Department (PED) requires attention to implementation. In order to optimize successful implementation, it is essential to understand multilevel implementation determinants. The Consolidated Framework for Implementation Research (CFIR) is a comprehensive conceptual implementation science framework developed to guide systematic assessment of these multilevel implementation contexts including: the intervention, inner and outer setting, the individuals involved, and the process by which implementation is accomplished.
Objective: The objective of this study was to utilize the CFIR to identify and assess key informant perspectives on barriers and facilitators that might influence intervention implementation and effectiveness of the NEAR4PEM checklist in PEDs.
Design/Methods: Data were collected using focus groups, and qualitative analysis was performed using the framework matrix approach. Interprofessional focus groups comprised of physicians, nurses, pharmacists, and respiratory therapists were conducted at four purposely sampled NEAR4PEM sites to represent varying annual visit volume, geographic location, and prior checklist experience. Identified barriers and facilitators were coded using CFIR domains and constructs and grouped into clinically-relevant themes.
Results: Nineteen key informants from 4 hospital systems participated. Participants noted barriers and facilitators from all 5 CFIR domains with most frequent determinants in the “inner setting.” Prominent barriers included high staff turnover, team resistance to change, and perceived lack of need for a checklist. Prominent facilitators included adequate staff training, communication and delivery to all key informants, and adaptability of the checklist.
Conclusion(s): Using the CFIR, we identified that determinants related to the inner setting (i.e., PEDs) were top of mind for participants regarding the implementation of the NEAR4PEM Pre-intubation Checklist. Data about these multilevel implementation determinants will support the creation and use of an implementation blueprint, or comprehensive plan that describes implementation strategies, goals, timelines, and key personnel necessary, to increase the uptake of the NEAR4PEM Pre-Intubation Checklist in PEDs. Additional future steps involve implementation of the Checklist with concurrent evaluation of implementation and patient outcomes.
Table 1. Participating PED Characteristics
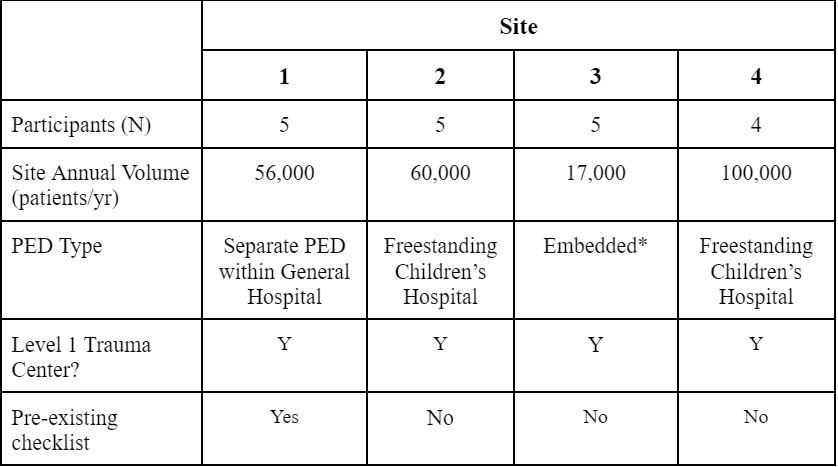 *Embedded - PED situated within a larger general ED, shared RNs and RTs with adult ED
*Embedded - PED situated within a larger general ED, shared RNs and RTs with adult EDTable 2. Barriers to Checklist Implementation
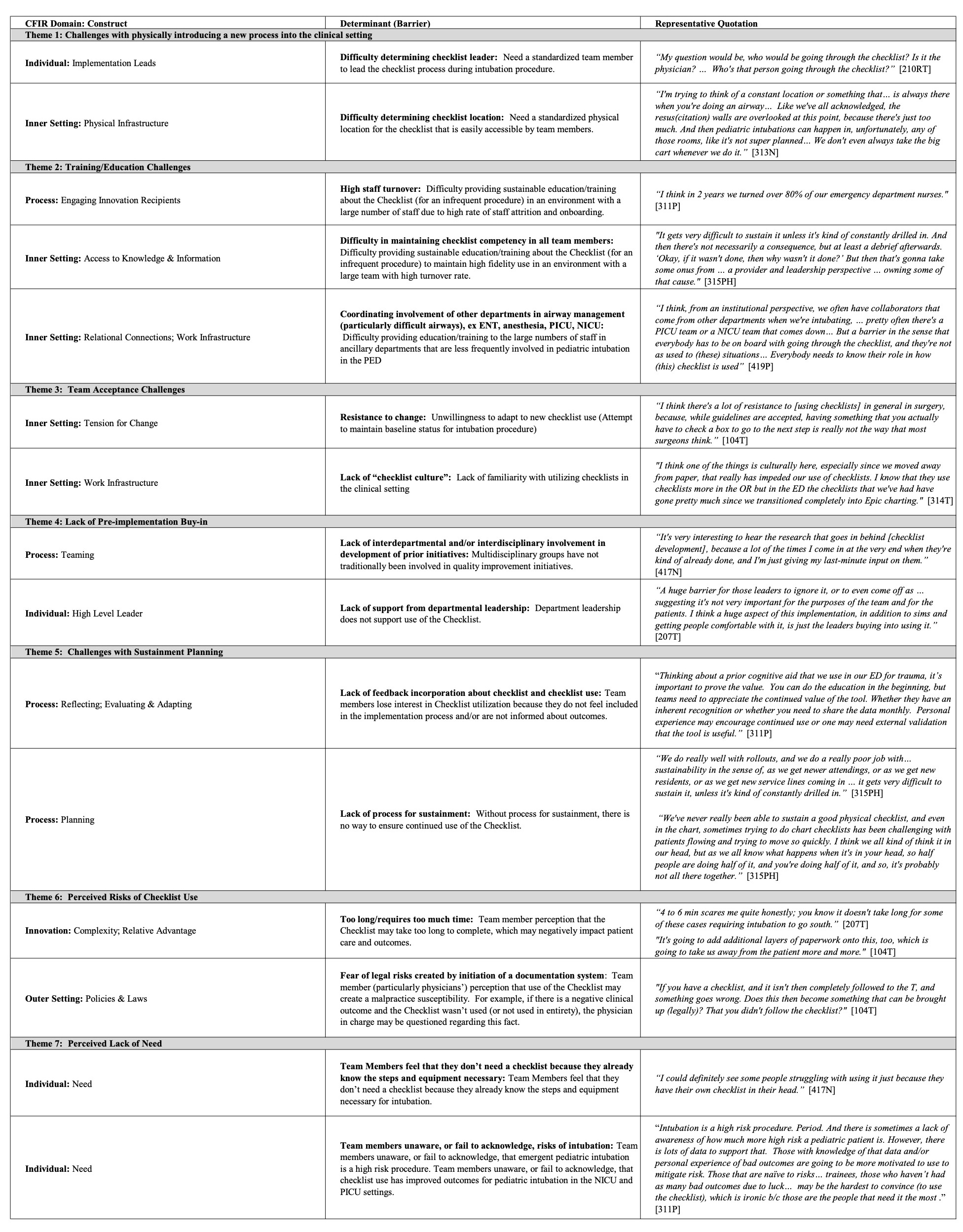 *Discipline of respondent is coded: P = PEM physician, RN = nurse, RT = respiratory therapist, PH = pharmacist, T = trauma team representative
*Discipline of respondent is coded: P = PEM physician, RN = nurse, RT = respiratory therapist, PH = pharmacist, T = trauma team representative Table 3. Facilitators to Checklist Implementation
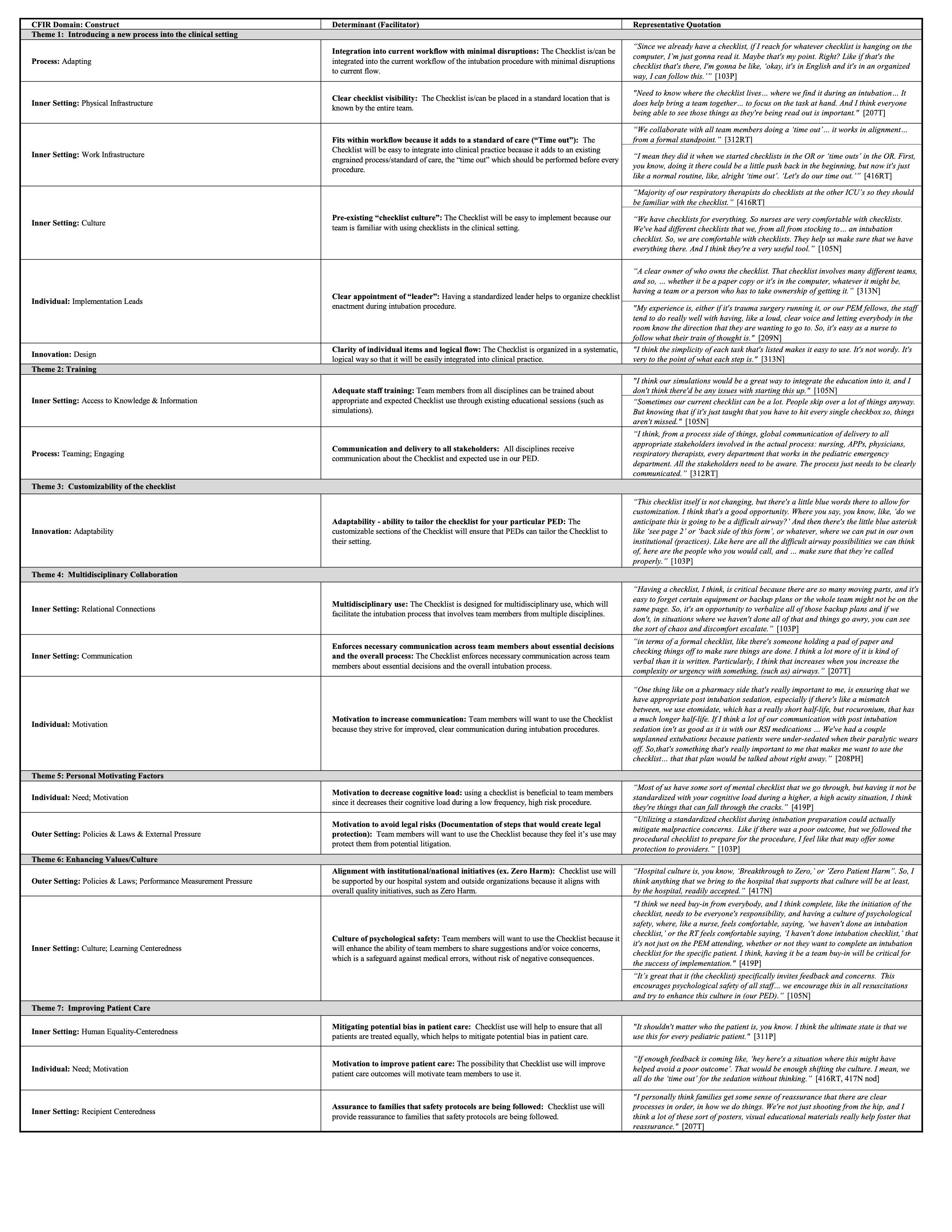 *Discipline of respondent is coded: P = PEM physician, RN = nurse, RT = respiratory therapist, PH = pharmacist, T = trauma team representative
*Discipline of respondent is coded: P = PEM physician, RN = nurse, RT = respiratory therapist, PH = pharmacist, T = trauma team representativeTable 1. Participating PED Characteristics
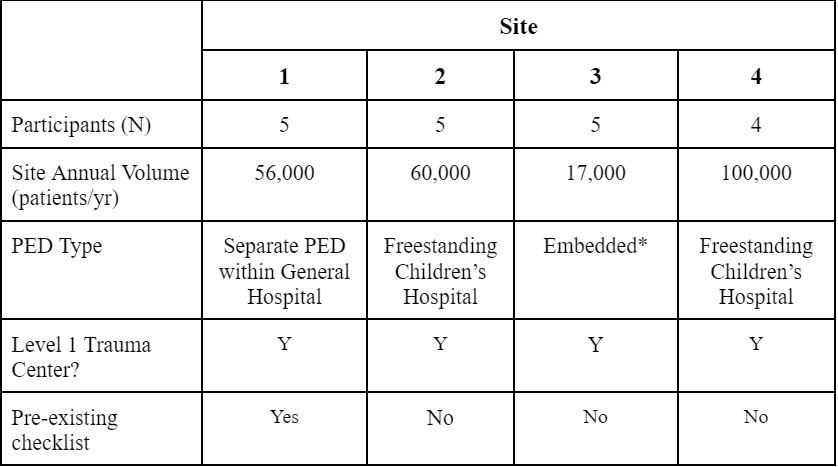 *Embedded - PED situated within a larger general ED, shared RNs and RTs with adult ED
*Embedded - PED situated within a larger general ED, shared RNs and RTs with adult EDTable 2. Barriers to Checklist Implementation
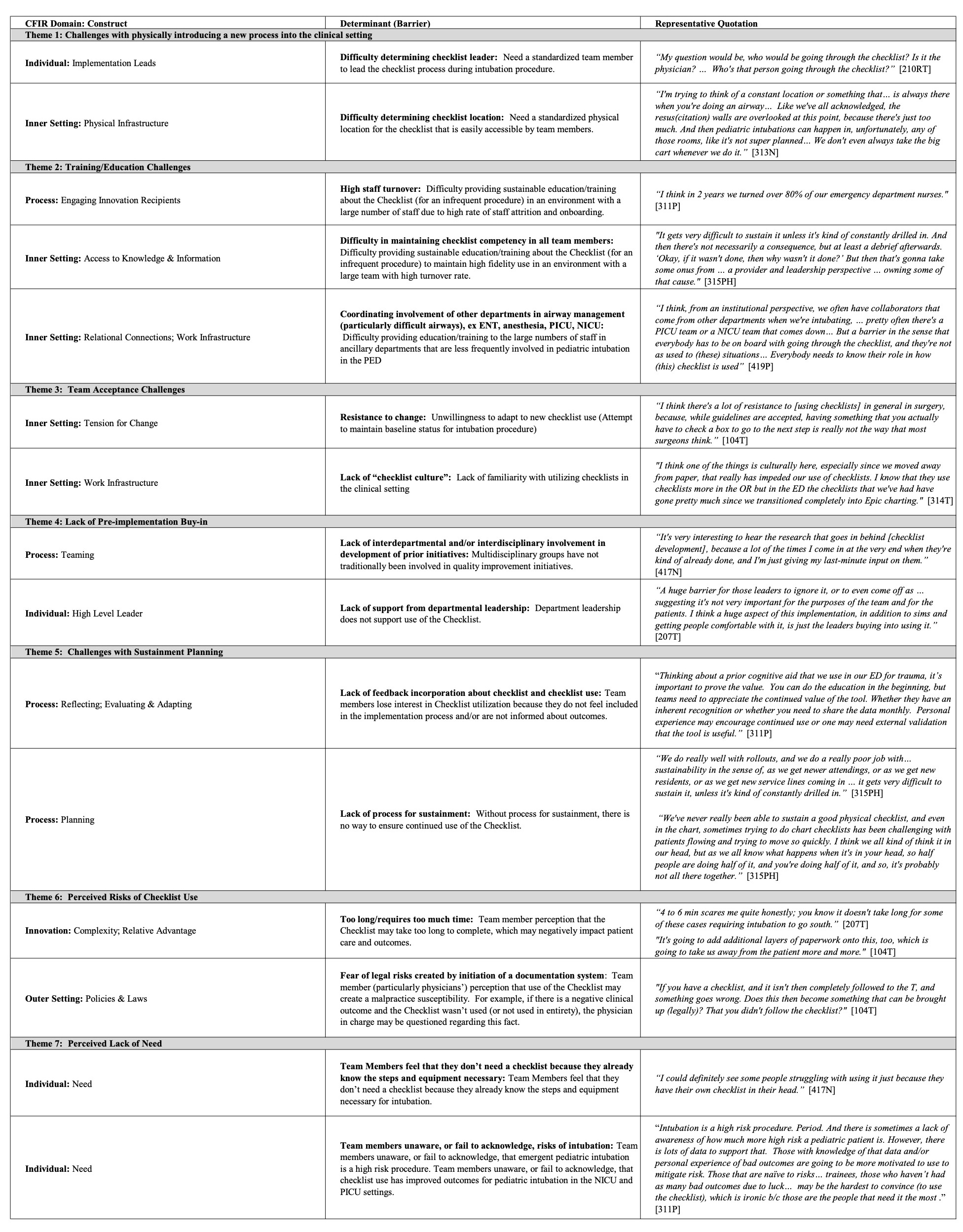 *Discipline of respondent is coded: P = PEM physician, RN = nurse, RT = respiratory therapist, PH = pharmacist, T = trauma team representative
*Discipline of respondent is coded: P = PEM physician, RN = nurse, RT = respiratory therapist, PH = pharmacist, T = trauma team representative Table 3. Facilitators to Checklist Implementation
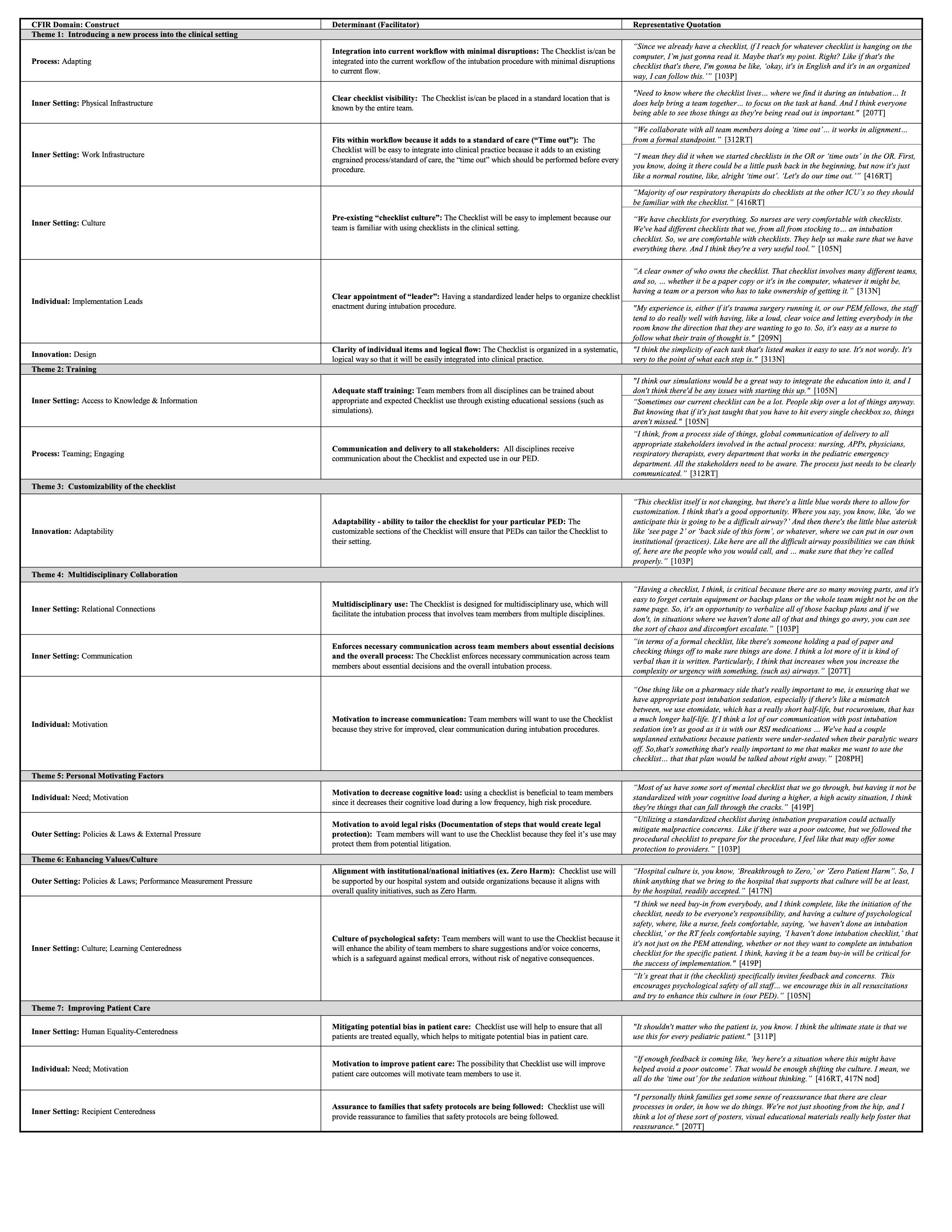 *Discipline of respondent is coded: P = PEM physician, RN = nurse, RT = respiratory therapist, PH = pharmacist, T = trauma team representative
*Discipline of respondent is coded: P = PEM physician, RN = nurse, RT = respiratory therapist, PH = pharmacist, T = trauma team representative
