Back
Background: Rhabdomyolysis is a pediatric diagnosis with a variable presentation. Recent data shows pediatric hospitalizations for primary rhabdomyolysis have increased in the last decade. The American Academy of Pediatrics released a review article in 2020 that provided general guidelines for treatment of rhabdomyolysis. These guidelines are helpful but lack standardization of care and are ambiguous about treatment specifics including types of intravenous fluids (IV), specific pain control regimens, and lab and imaging diagnostic work up required. Standardization of care is linked to positive outcomes, but to achieve this goal, we must first understand the variation of care.
Objective: The primary aim of this study was to describe the hospital level variation in management of primary rhabdomyolysis that exists across children's hospitals. Our secondary aim was to determine how resource utilization relates to clinical outcomes.
Design/Methods: This was a retrospective cross-sectional study utilizing data from the Pediatric Health Information System database of patients aged 0-18 years with the primary discharge diagnosis of rhabdomyolysis who were admitted between January 2020 to December 2023. Our outcomes were adjusted for differences in age, race, payor, number of complex chronic conditions, and Hospitalization Resource Intensity Score for Kids.
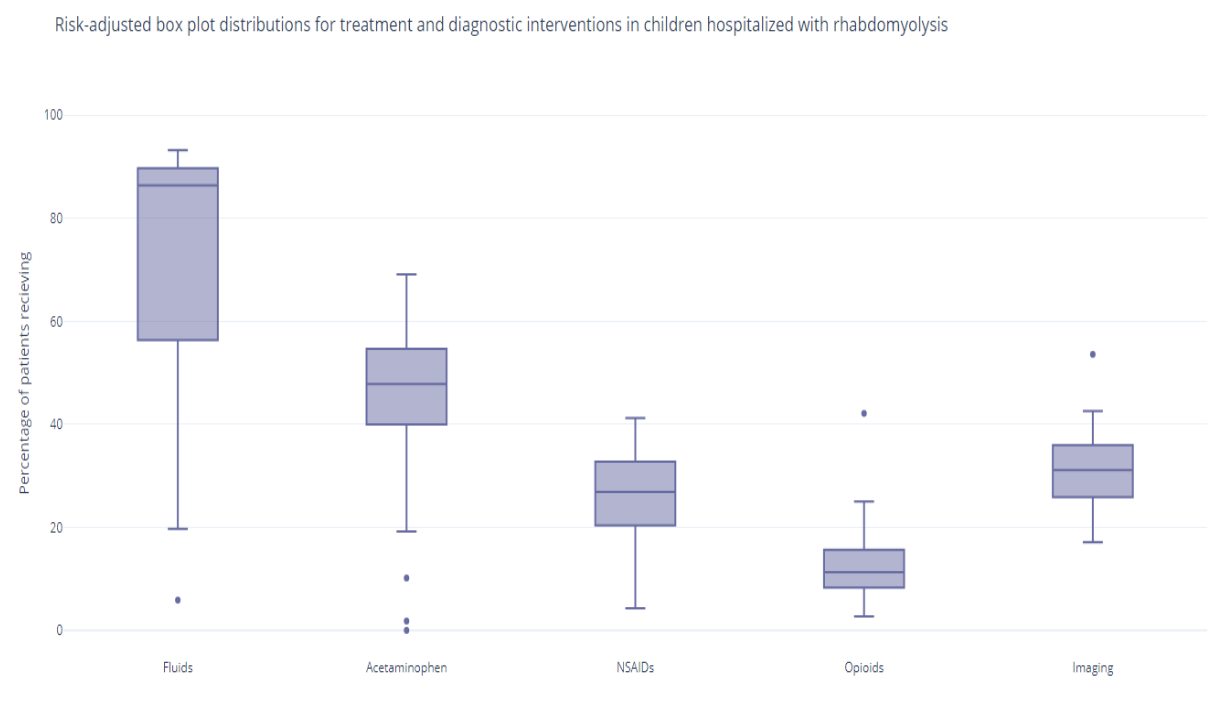
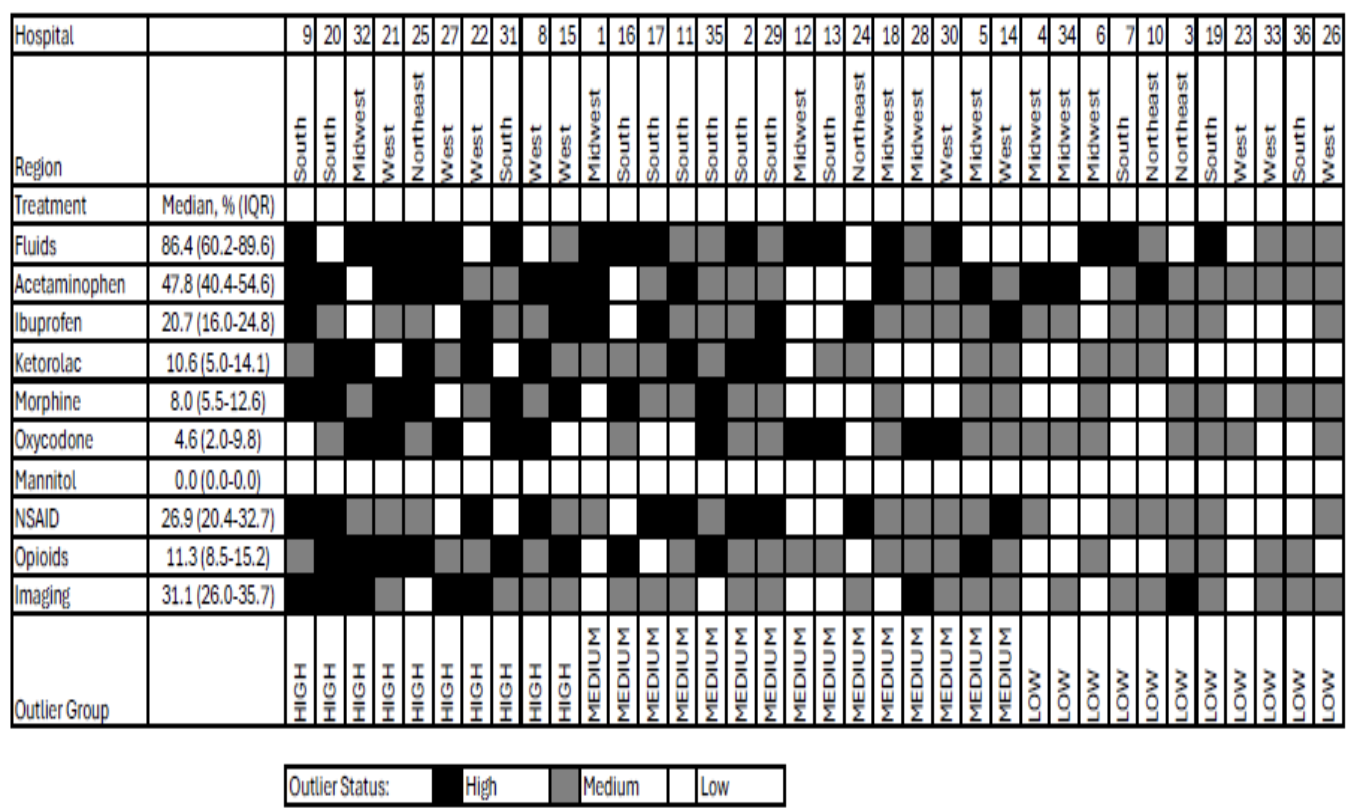
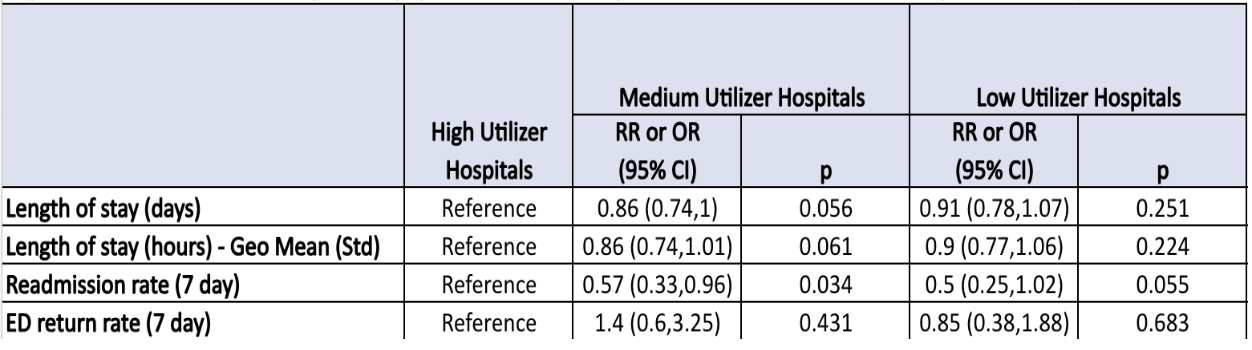
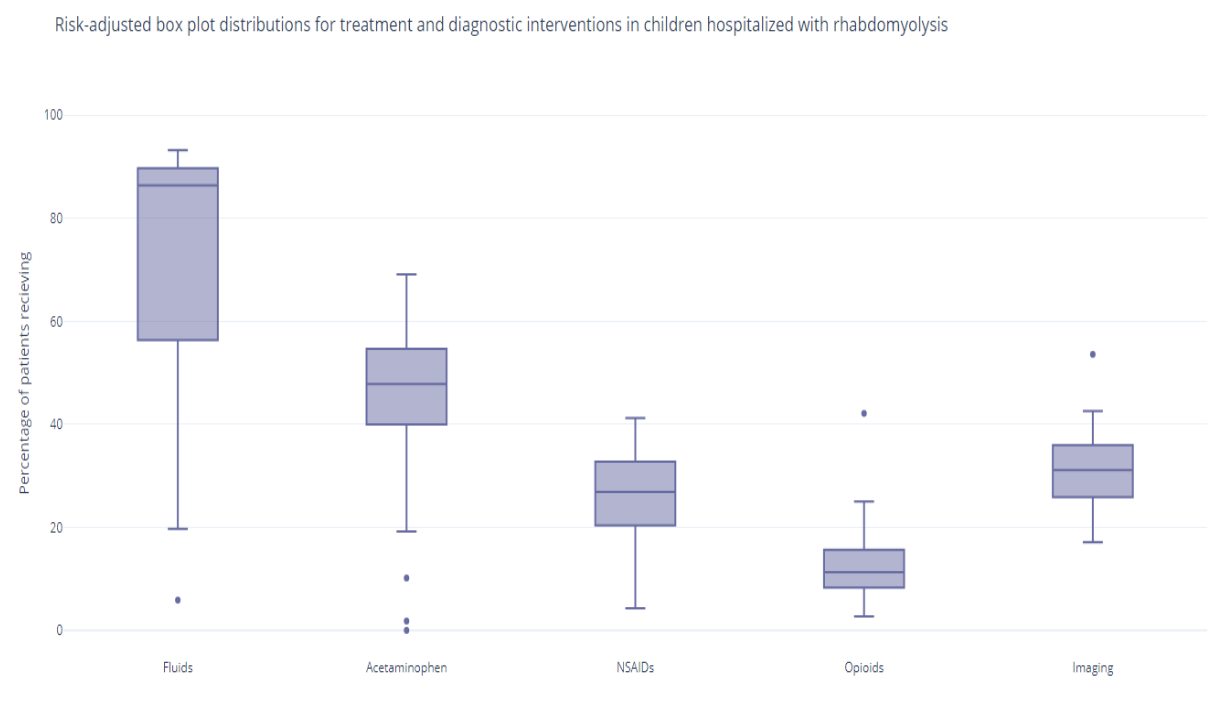
Results: 3779 cases across 36 children’s hospitals met inclusion criteria. Fluids were received by a median 86.4% (IQR: 60.2%-89.6%) across the hospitals. A variety of IV fluids were used with the most common being sodium chloride by a median (67.1%), followed by dextrose and sodium chloride (45.1%), dextrose and sodium chloride with potassium chloride (14.2%), and dextrose in water (10.4%). Acetaminophen was the most used analgesic medication (47.8%), followed by NSAIDs (26.9%), and opioids (11.3%). Use of mannitol was uncommon with only 0.2% of total cases studied receiving it. Use of imaging studies was observed in all 36 hospitals and occurred in 31.1%; (IQR 26%-35.7%). When adjusted, there was no statistical difference in LOS (55.7 hours), or emergency department return rate (1.5%) between the high, medium, and lower utilizer groups.There was a statistically significant decrease in the 7-day readmission rate in the medium utilizer group compared to the high utilizer group (Odds Ratio 0.57, 95% CI: 0.33-0.96).
Conclusion(s): There was wide variation across hospitals in all aspects of treatment for children hospitalized with rhabdomyolysis including fluid use, type, and analgesic use. Further, high resource utilization did not improve the measured clinical outcomes.
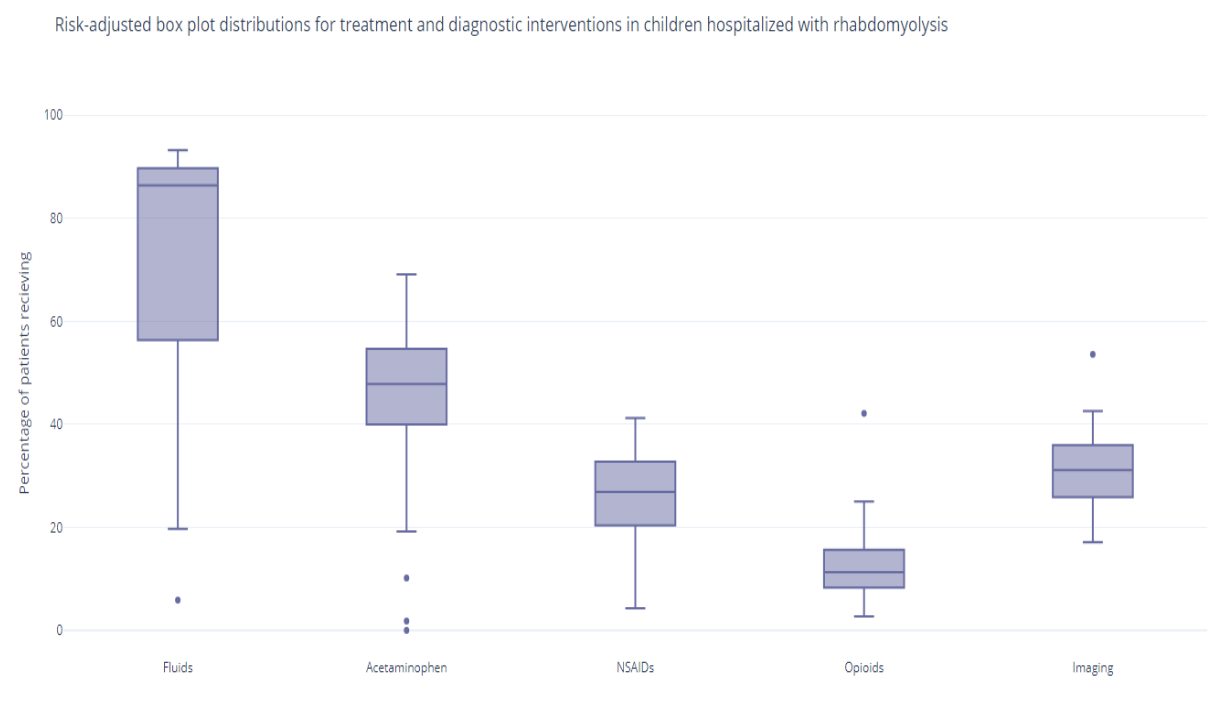
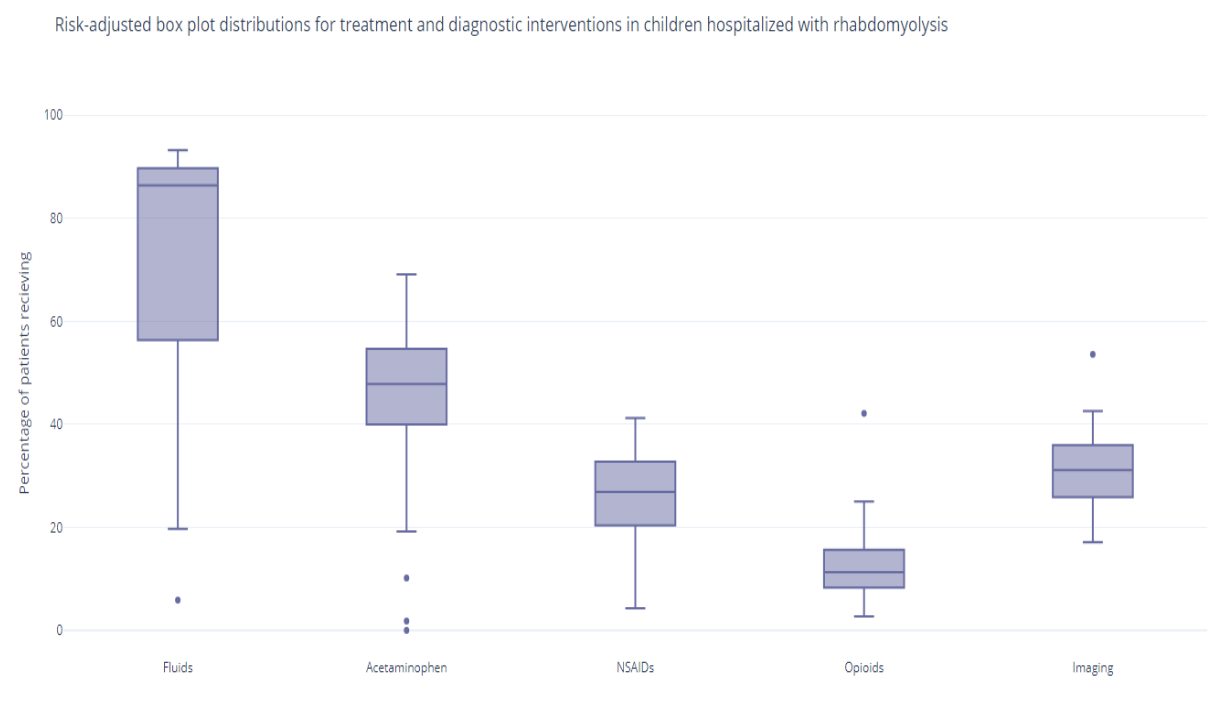
Box plot distribution for treatment and diagnosis in our adjusted data
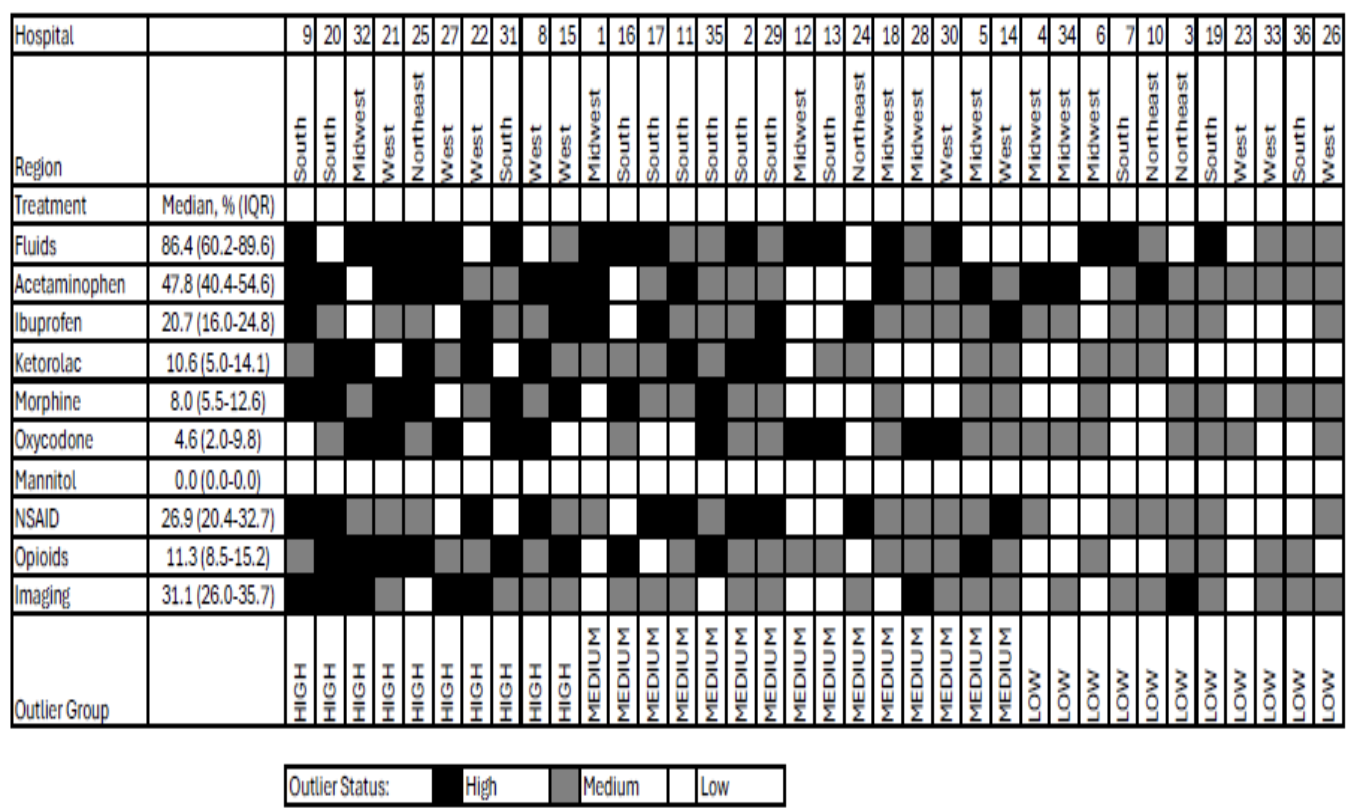
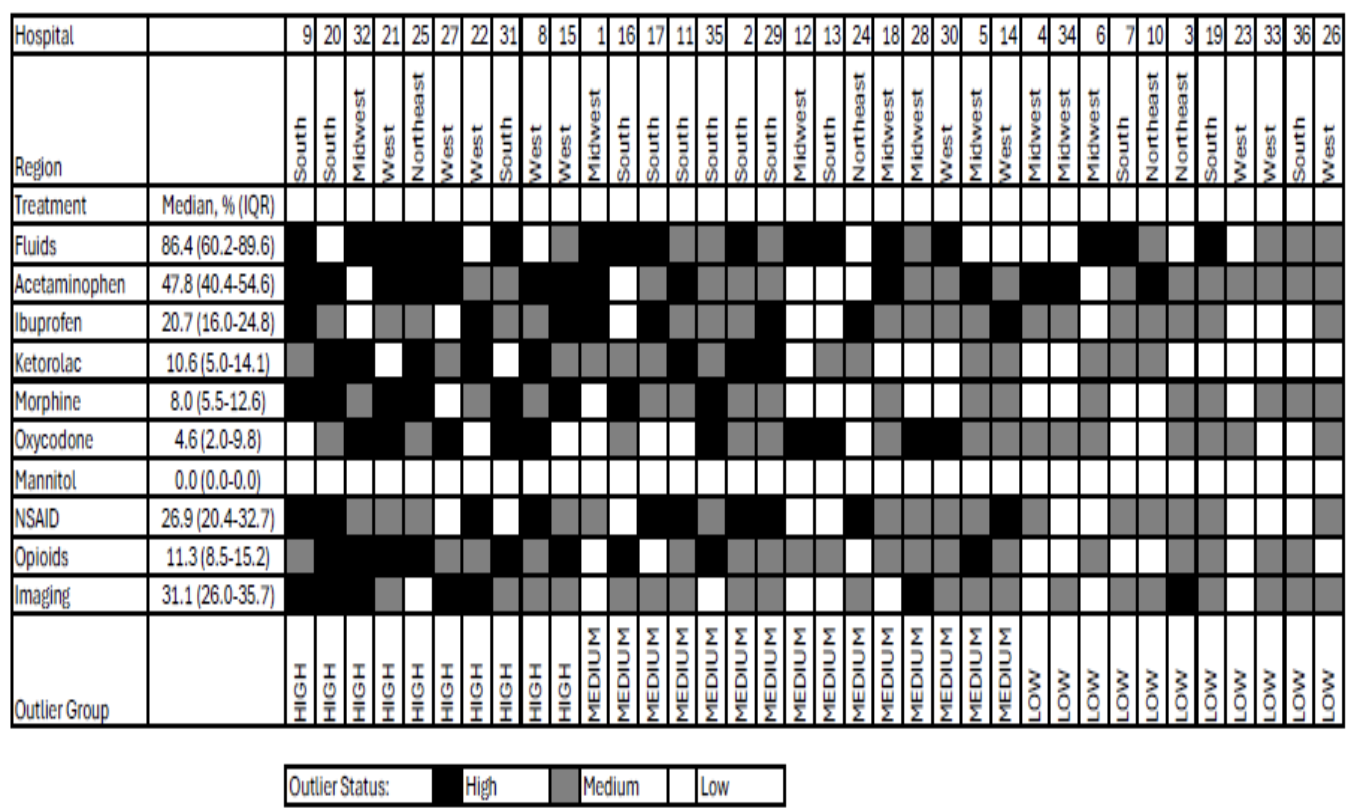
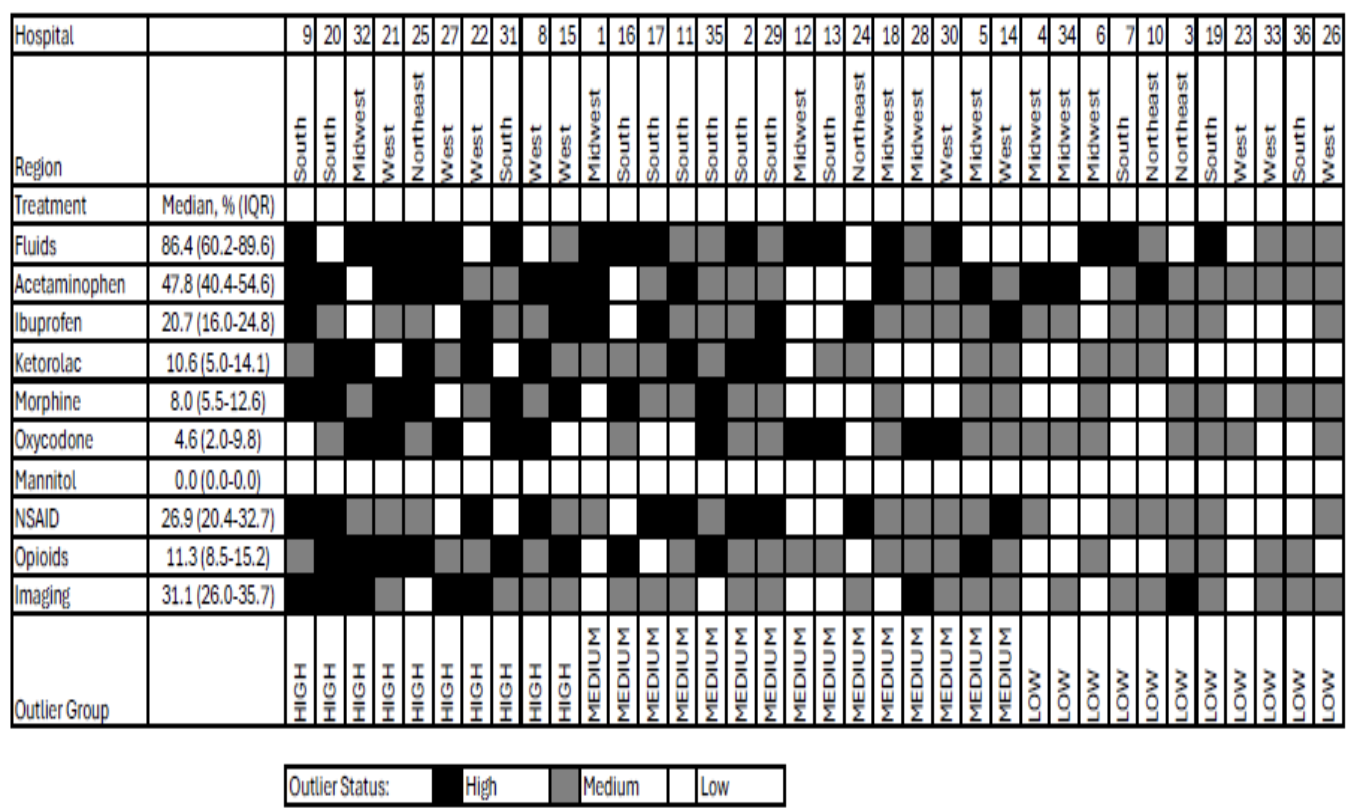
Heat map of risk adjusted resource utilization by hospitals
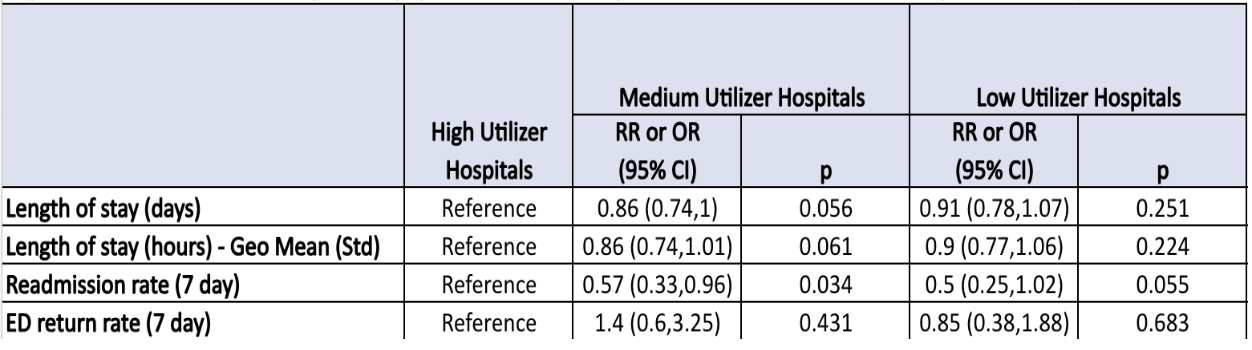
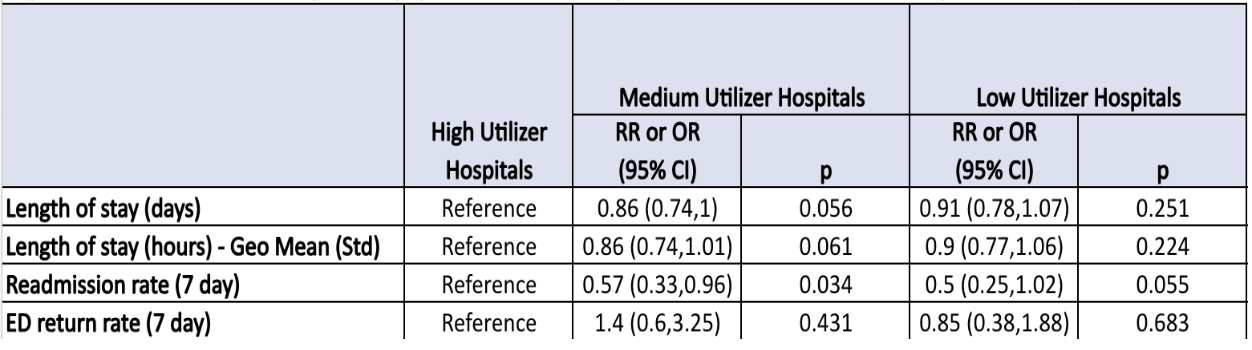
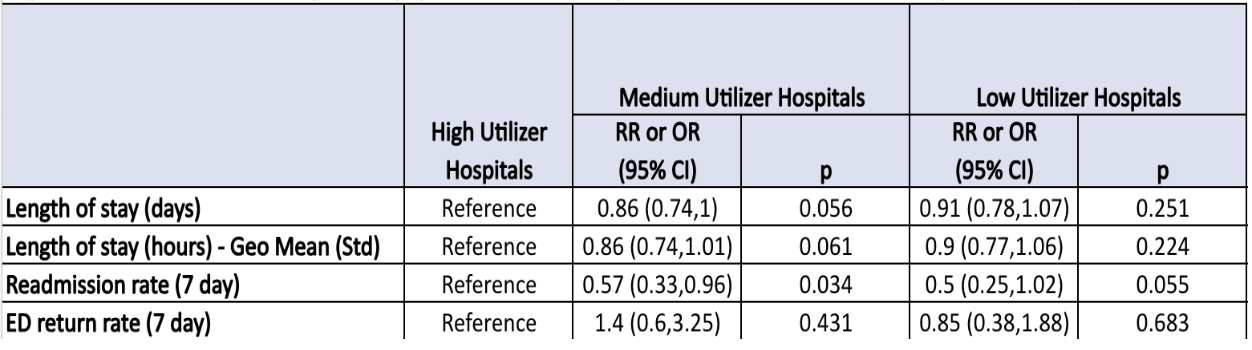
Adjusted Outcomes for differences in age, race, payor, number of CCC, census region, H-risk and clustered on hospitals.
Box plot distribution for treatment and diagnosis in our adjusted data
Heat map of risk adjusted resource utilization by hospitals
Adjusted Outcomes for differences in age, race, payor, number of CCC, census region, H-risk and clustered on hospitals.
Hospital Medicine 6: Clinical
Session: Hospital Medicine 6: Clinical
548 - Variation in Treatment and Clinical Outcome of Primary Rhabdomyolysis in Children’s Hospitals
Sunday, April 27, 2025
8:30am – 10:45am HST
Darya Falamarzi, Helen DeVos Children's Hospital, Grand Rapids, MI, United States; Matthew Hall, Children's Hospital Association, Lenexa, KS, United States; David C. Synhorst, Helen DeVos Children's Hospital, Rockford, MI, United States; Meghan Lemmen, Corewell Health, White (Not Hispanic or Latino), MI, United States; Katie Peterson, Corewell health, Grand Rapids, MI, United States; Grace E. Tsaloff, Helen DeVos Children's Hospital, Wyoming, MI, United States

Meghan Lemmen, MD (she/her/hers)
Pediatric Resident
Corewell Health
White (Not Hispanic or Latino), Michigan, United States
Presenting Author(s)
Background: Rhabdomyolysis is a pediatric diagnosis with a variable presentation. Recent data shows pediatric hospitalizations for primary rhabdomyolysis have increased in the last decade. The American Academy of Pediatrics released a review article in 2020 that provided general guidelines for treatment of rhabdomyolysis. These guidelines are helpful but lack standardization of care and are ambiguous about treatment specifics including types of intravenous fluids (IV), specific pain control regimens, and lab and imaging diagnostic work up required. Standardization of care is linked to positive outcomes, but to achieve this goal, we must first understand the variation of care.
Objective: The primary aim of this study was to describe the hospital level variation in management of primary rhabdomyolysis that exists across children's hospitals. Our secondary aim was to determine how resource utilization relates to clinical outcomes.
Design/Methods: This was a retrospective cross-sectional study utilizing data from the Pediatric Health Information System database of patients aged 0-18 years with the primary discharge diagnosis of rhabdomyolysis who were admitted between January 2020 to December 2023. Our outcomes were adjusted for differences in age, race, payor, number of complex chronic conditions, and Hospitalization Resource Intensity Score for Kids.
Results: 3779 cases across 36 children’s hospitals met inclusion criteria. Fluids were received by a median 86.4% (IQR: 60.2%-89.6%) across the hospitals. A variety of IV fluids were used with the most common being sodium chloride by a median (67.1%), followed by dextrose and sodium chloride (45.1%), dextrose and sodium chloride with potassium chloride (14.2%), and dextrose in water (10.4%). Acetaminophen was the most used analgesic medication (47.8%), followed by NSAIDs (26.9%), and opioids (11.3%). Use of mannitol was uncommon with only 0.2% of total cases studied receiving it. Use of imaging studies was observed in all 36 hospitals and occurred in 31.1%; (IQR 26%-35.7%). When adjusted, there was no statistical difference in LOS (55.7 hours), or emergency department return rate (1.5%) between the high, medium, and lower utilizer groups.There was a statistically significant decrease in the 7-day readmission rate in the medium utilizer group compared to the high utilizer group (Odds Ratio 0.57, 95% CI: 0.33-0.96).
Conclusion(s): There was wide variation across hospitals in all aspects of treatment for children hospitalized with rhabdomyolysis including fluid use, type, and analgesic use. Further, high resource utilization did not improve the measured clinical outcomes.
Box plot distribution for treatment and diagnosis in our adjusted data
Heat map of risk adjusted resource utilization by hospitals
Adjusted Outcomes for differences in age, race, payor, number of CCC, census region, H-risk and clustered on hospitals.
Box plot distribution for treatment and diagnosis in our adjusted data
Heat map of risk adjusted resource utilization by hospitals
Adjusted Outcomes for differences in age, race, payor, number of CCC, census region, H-risk and clustered on hospitals.