Health Equity/Social Determinants of Health 7
Session: Health Equity/Social Determinants of Health 7
739 - Caregiver Perceptions of Housing-related Social Risks and Pediatric Asthma Morbidity: A Qualitative Study
Sunday, April 27, 2025
8:30am - 10:45am HST
Publication Number: 739.4111
Jenny L. Ren, Children's National Health System, Washington, DC, United States; Janet A. Phoenix, George Washington University School of Medicine and Health Sciences, Washington, DC, United States; Rachel H.F.. Margolis, Children's National Health System, Washington, DC, United States; Shayla Stringfield, IMPACT DC, Children’s National Hospital, Washington, DC, United States; Shilpa J.. Patel, Children's National Health System, Washington, DC, United States; Kavita Parikh, Children's National Health System, Washington DC, DC, United States; Jordan Tyris, Children’s National Hospital, Washington, DC, United States

Jenny L. Ren, MD (she/her/hers)
Pediatric Resident
Children's National Health System
Washington, District of Columbia, United States
Presenting Author(s)
Background: Housing-related social risks (HSR) (e.g., pests, mold, smoke) contribute to pediatric asthma disparities, and remediation may reduce morbidity. However, caregivers’ perceptions of HSR and their relationship with children’s asthma remain understudied, limiting social needs-informed and patient-centered asthma care.
Objective: Describe caregivers’ perspectives on 1) the relationship between the home environment and child asthma morbidity and 2) experiences with housing-related resources.
Design/Methods: Caregivers of children < 17 years (y) were interviewed during their child’s asthma-related hospitalization at a freestanding children’s hospital. Demographic data (child and caregiver age, caregiver role, preferred language), asthma history (child’s age of diagnosis, family history of asthma), and exposure to in-home asthma triggers were collected and summarized descriptively. Semi-structured interview guides developed by local pediatric asthma and housing experts assessed: 1) perception of the home environment’s impact on the child’s asthma; 2) perceived ability to remedy in-home asthma triggers; and 3) experience with housing-related assistance. Interviews were audio-recorded, transcribed, and analyzed using rapid qualitative analysis, in which interview content was summarized and compared across domains to identify themes.
Results: Twenty-seven caregivers were interviewed (20 mothers, 6 fathers, 1 grandmother; ages 21-59y; 26/27 [96%] spoke English). Most children had an existing asthma diagnosis (n=23,85%) and >1 family member with asthma (n=24,89%). Children were evenly split by sex (n=13 girls,48%) and ranged from 16 months-17y old (mean: 6.6y [standard deviation 3.4]). All caregivers reported exposure to >1 trigger, commonly dust (n=25,93%), pets (n=20,74%), and smoke (n=17,63%) (Fig. 1). Four themes emerged (Table 1): 1) families who experienced multiple, persistent HSR felt their only option was to move; 2) despite ongoing HSR impacting their child’s asthma, caregivers were unsure how to access help; 3) there was often a discrepancy between the HSR that children experienced versus the HSR caregivers perceived to impact their asthma; 4) caregivers with no/minimal exposure to HSR did not believe their current environment impacted their child’s asthma.
Conclusion(s): In this high-risk, hospitalized pediatric asthma cohort, caregivers with HSR often had unsuccessful or limited experiences with housing-related assistance. These data are informing educational strategies to optimize families’ knowledge of HSR, providers’ assessment of families’ HSR, and families’ connection to appropriate housing resources.
Figure 1. Percentage of participants exposed to each in-house asthma trigger.
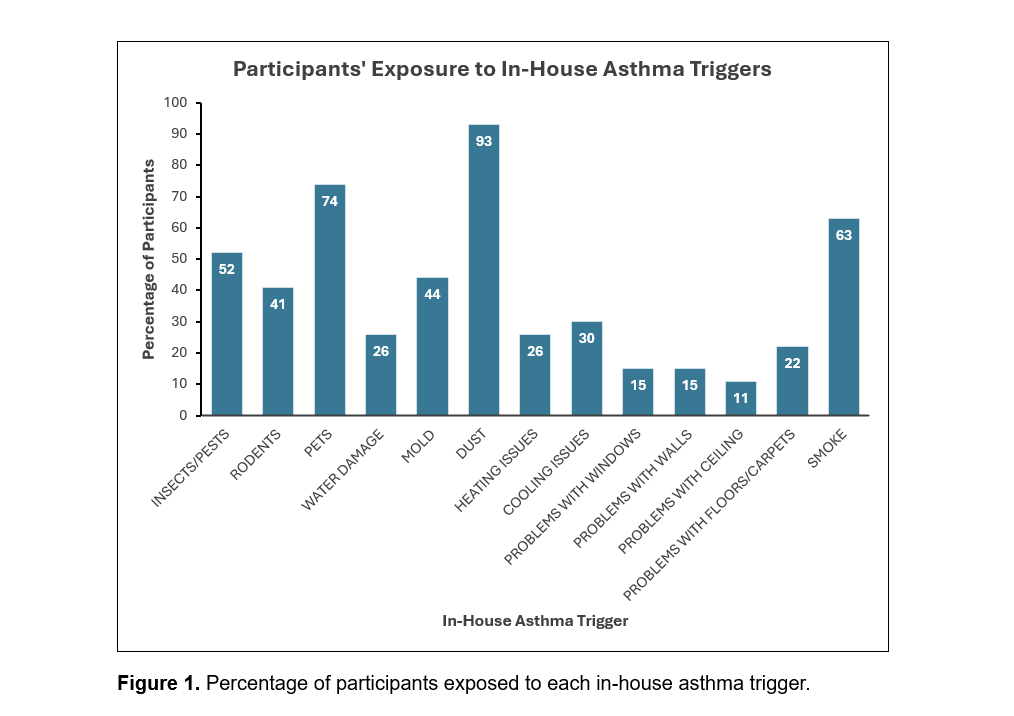
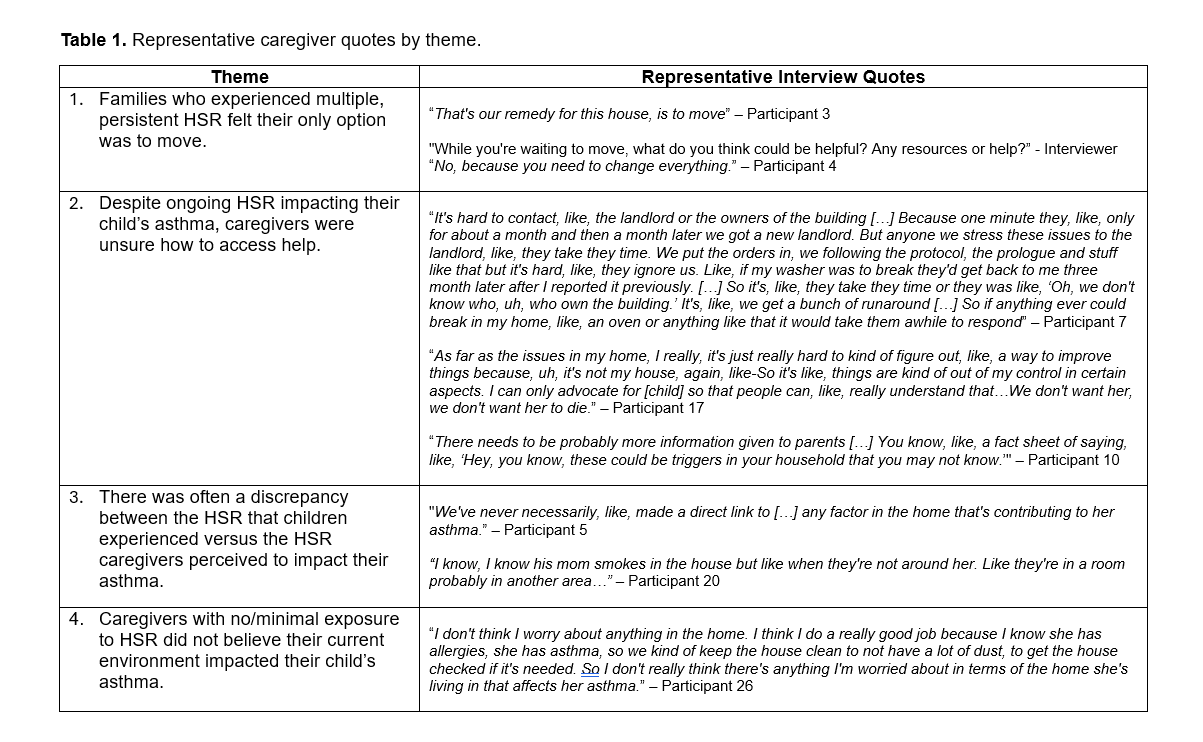
Table 1. Representative caregiver quotes by theme.
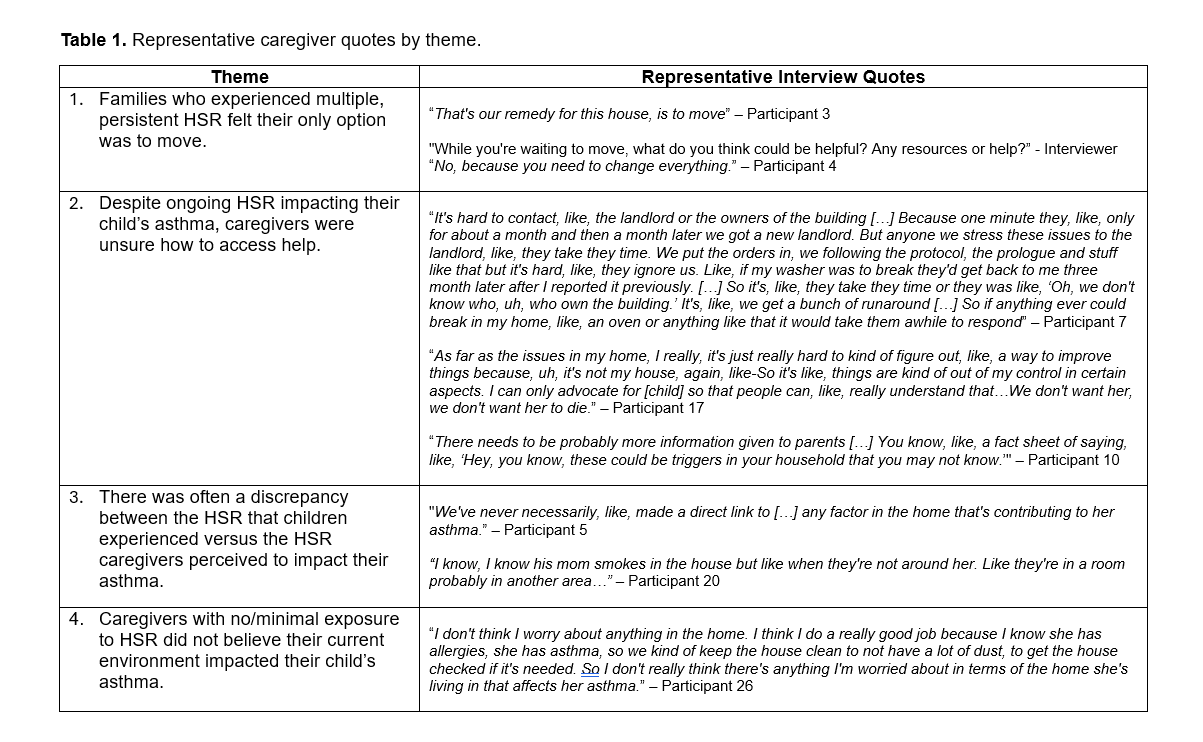
Figure 1. Percentage of participants exposed to each in-house asthma trigger.
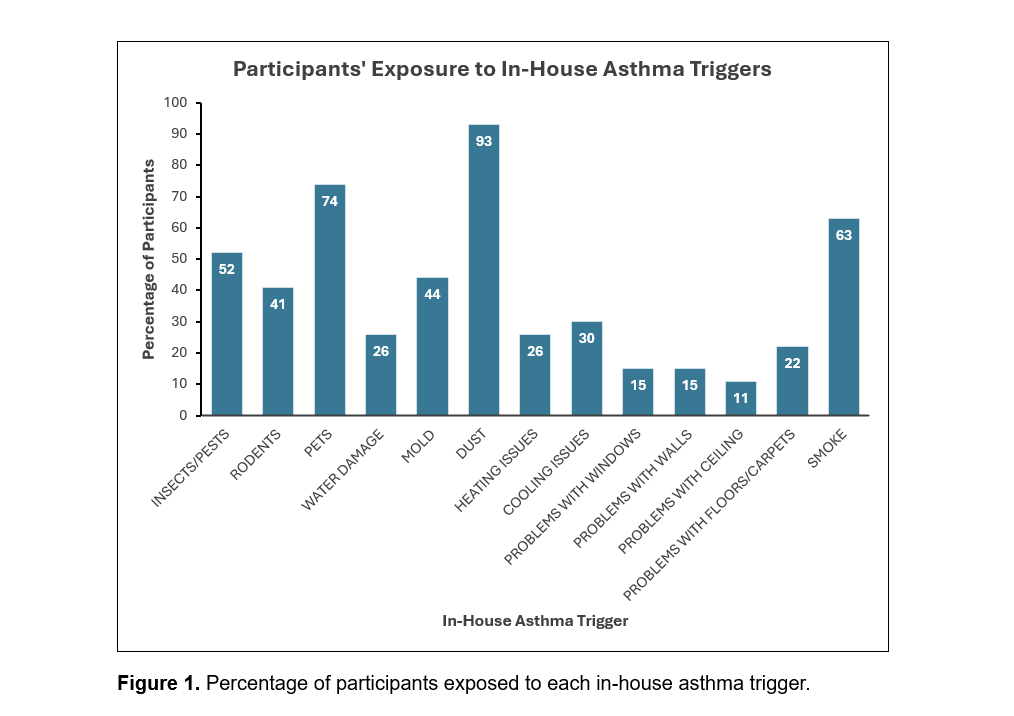
Table 1. Representative caregiver quotes by theme.