Obesity 1
Session: Obesity 1
268 - “Every day we learn something about the way we're communicating”: perspectives of pediatric primary care clinicians on discussing overweight/obesity
Sunday, April 27, 2025
8:30am - 10:45am HST
Publication Number: 268.3575
Katrina B. Dietsche, Yale School of Medicine, New Haven, CT, United States; Emily B. Finn, Yale School of Medicine, New Haven, CT, United States; Carlin Aloe, Yale School of Medicine, New Haven, CT, United States; Jhourdan Allen, Ponce Health Sciences University School of, St. Louis, MO, United States; Jessica Ray, University of Florida College of Medicine, Gainesville, FL, United States; Hollyce Tyrrell, Academic Pediatric Association, McLean, VA, United States; Jeremy Michel, Childrens Hospital of Philadelphia, Bryn Mawr, PA, United States; Randall Grout, Indiana University School of Medicine, Indianapolis, IN, United States; Charles Wood, Duke University School of Medicine, Durham, NC, United States; Eliana M. Perrin, Johns Hopkins University Schools of Medicine, Nursing, and Public Health, Baltimore, MD, United States; Laura J. Damschroder, Implementation Pathways, LLC, Chelsea, MI, United States; Mona Sharifi, Yale School of Medicine, New Haven, CT, United States

Katrina B. Dietsche (she/her/hers)
Medical Student
Yale School of Medicine
New Haven, Connecticut, United States
Presenting Author(s)
Background: Patients and families prefer, and national guidelines advise, that clinicians use non-stigmatizing language when addressing overweight/obesity, yet little is known about the degree to which this occurs in context of counseling in pediatric primary care.
Objective: To explore the language and communication strategies used by PCCs when describing their approach to caring for patients/families affected by overweight/obesity.
Design/Methods: We conducted a secondary analysis of transcripts from semi-structured qualitative interviews conducted with PCCs recruited from 77 clinics across three health systems in the Northeast, South, and Midwest. We used content analysis to identify all weight-related terms used by PCCs in each transcript. We then calculated the proportion of participants that used each term at least once during their interview and identified “non-person-first language” discouraged by academic, professional, and patient advocacy societies and “potentially stigmatizing” terms based on a literature review of weight-related terms preferred by patients/families in clinical settings. Inductive thematic analysis was also used to identify strategies for discussing weight and factors influencing those discussions.
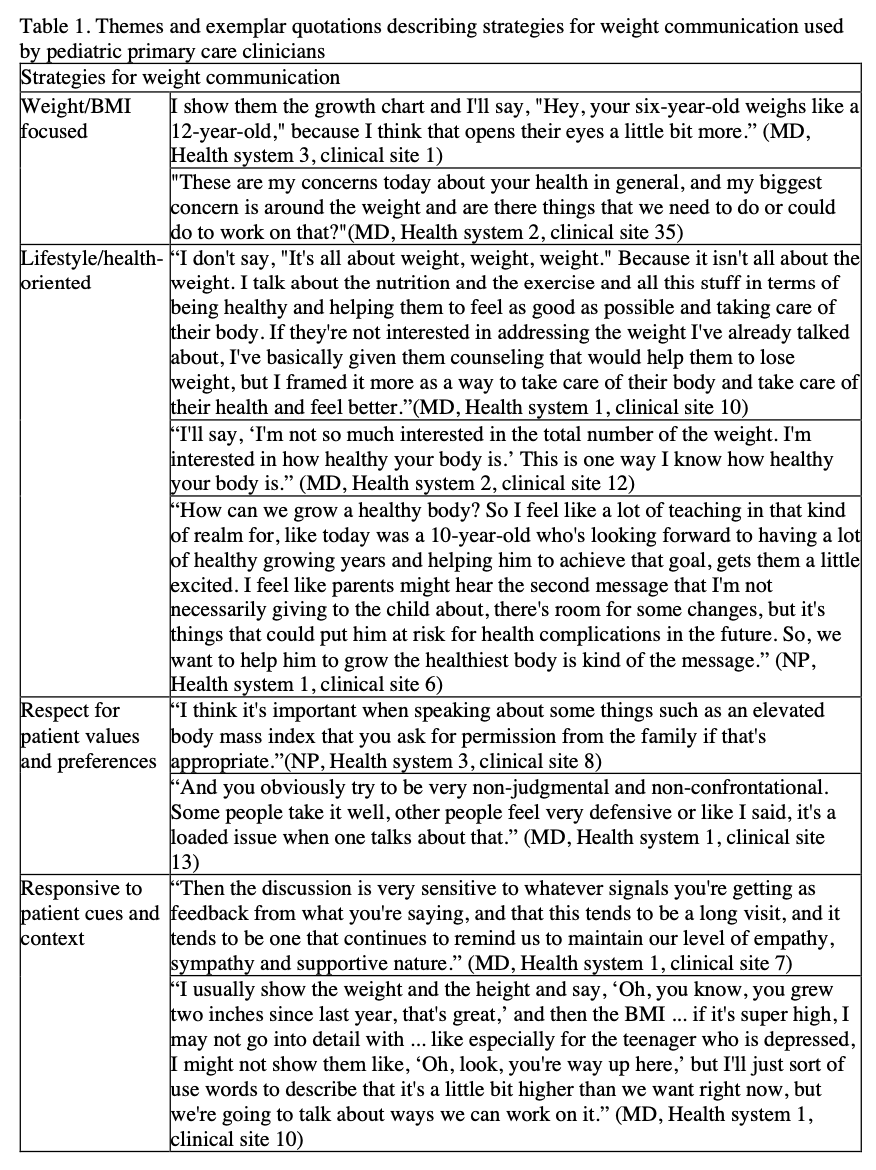
Results: Of 21 PCCs interviewed (81% identified as women and 86% reported ≥10 years in practice). Content analysis revealed that PCCs primarily used clinical terminology including “weight” (95%), "BMI" (95%), and "obesity" (90%) when discussing pediatric overweight/obesity. Over half of PCCs (62%) used non-person-first language at least once in interview transcripts. Potentially stigmatizing terms such as “heavy” (14%), “morbidly obese” (14%), and “fat” (0%) were rarely or never used. Four themes emerged on strategies for communicating about weight: 1) Weight/BMI-focused, 2) Lifestyle/health-oriented, 3) Respect for patient values and preferences, and 4) Responsiveness to patient/family cues and context (table 1). Factors influencing PCC’s communication included self-doubt, fear of stigmatizing patients, and their own body habitus.
Conclusion(s): PCCs expressed the importance of respectful, responsive, and non-stigmatizing communication when discussing overweight/obesity with patients/families, yet most used non-person first language and some used potentially stigmatizing terms during interviews. Our findings reveal the need to better support PCCs in delivering patient-centered, non-stigmatizing care for overweight/obesity.
Table 1. Themes and exemplar quotations describing strategies for weight communication used by pediatric primary care clinicians
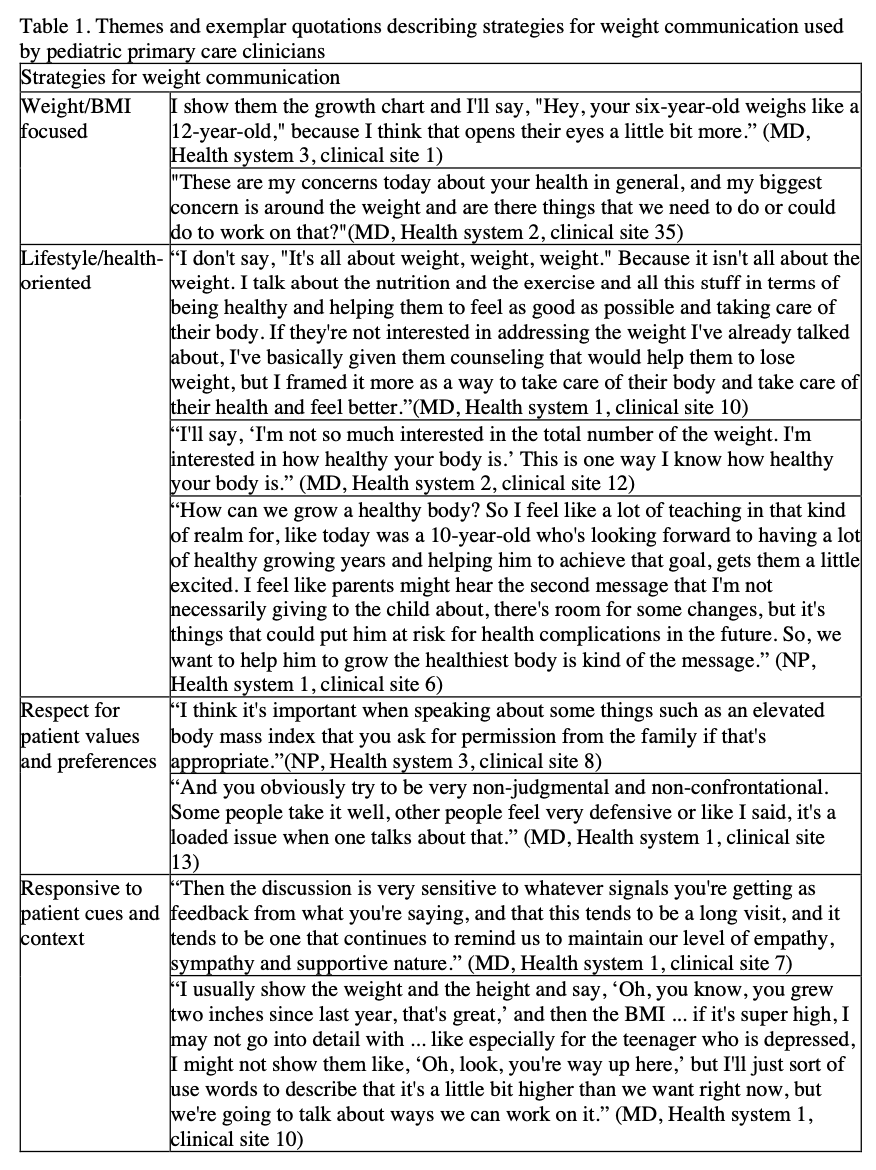
Table 1. Themes and exemplar quotations describing strategies for weight communication used by pediatric primary care clinicians