Child Abuse & Neglect 1
Session: Child Abuse & Neglect 1
338 - AHT Diagnosis: The Influences of Clinical Presentation and Evidence of Impact
Sunday, April 27, 2025
8:30am - 10:45am HST
Publication Number: 338.3689
Ruairi E. Smith-Dewey, Children's Mercy Hospital, KANSAS CITY, MO, United States; Angela Bachim, Baylor College of Medicine, Houston, TX, United States; Colleen J. Bressler, Medical University of South Carolina College of Medicine, Charleston, SC, United States; Kristine A. Campbell, University of Utah School of Medicine, Salt Lake City, UT, United States; Lori Frasier, Penn state hershey, Hershey, PA, United States; Christopher Greeley, Baylor College of Medicine, Houston, TX, United States; Danielle Horton, Children's Mercy Hospital, Kansas City, MO, United States; Nicole R. Johnson, University of Minnesota Masonic Children's Hospital, Minneapolis, MN, United States; Jan Leonard, Children's Hospital of Philadelphia, Philadelphia, PA, United States; Megan M.. Letson, Nationwide Children's Hospital, Columbus, OH, United States; Caitlin R. McNamara, UPMC Childrens Hospital of Pittsburgh, Pittsburgh, PA, United States; Shalon M. Nienow, UC San Diego School of Medicine, San Diego, CA, United States; Joanne N. Wood, Children's Hospital of Philadelphia, Philadelphia, PA, United States; Jim Anderst, Children's Mercy Hospitals and Clinics, Kansas City, MO, United States
.jpg)
Ruairi E. Smith-Dewey, DO (she/her/hers)
Child Abuse Pediatric Fellow
Children's Mercy Hospital
KANSAS CITY, Missouri, United States
Presenting Author(s)
Background: In cases where Child Abuse Pediatricians (CAPs) diagnose abusive head trauma (AHT) in young children, some factors surrounding the diagnosis have been challenged including causative shaking, necessity of external signs of impact, or concomitant suspicious injuries. Evaluation of CAP diagnoses in children with subdural hemorrhage (SDH) can give insight into factors related to the frequency of abusive head trauma (AHT) diagnoses. Additionally, characterization of those with SDH+CSI without evidence of impact may inform controversies around AHT diagnoses.
Objective: We aim to compare CAP diagnoses in subjects with SDH across clinical presentations and in the context of evidence of head impact. We also aim to describe the subjects with SDH+CSI and no external signs of impact to the head.
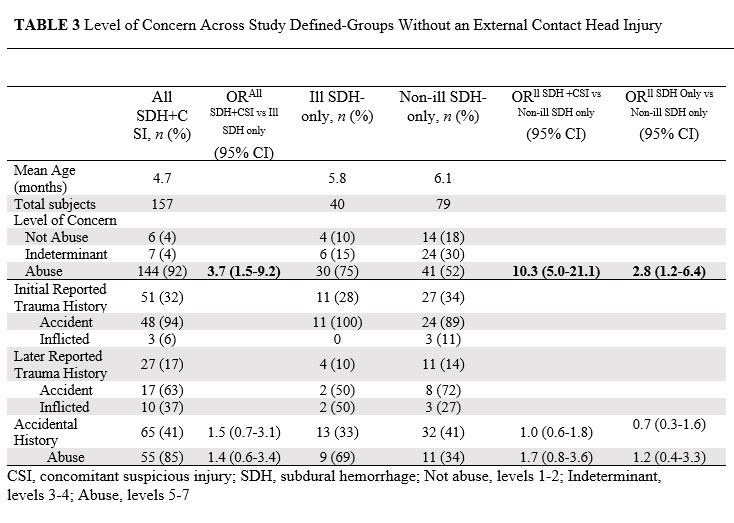
Design/Methods: Retrospective case-control study using Child Abuse Pediatrics Research Network (CAPNET) data from 10 sites over 27 months. Subjects were < 24 months old with SDH and in-person CAP evaluation. Subjects were divided into groups based on study determined criteria: Ill SDH only, Non-ill SDH only, and SDH with CSI. Ill status was categorized by clinical signs of cardio-respiratory collapse and/or significantly altered consciousness. CSIs are injuries highly associated with abuse in the following categories: skin, bones, eyes, and abdomen. CAP diagnosis of abuse was defined as 5-7 on a 7-point scale. Abuse diagnoses were compared across study groups. Head impact signs included bruising to the head, scalp swelling, and skull fractures. Comparisons used unadjusted odds ratios with 95% confidence intervals.
Results: Of the 492 study subjects, 386 (78%) were diagnosed with AHT. The SDH+CSI subjects were more likely to be diagnosed with abuse than Ill-SDH (OR 2.7, 95% CI 1.3-5.6) and Non-ill SDH (OR 7.2, 95% CI 4.3-12.1). Of the 276 subjects without signs of head impact, 215 (78%) were diagnosed with abuse. In this subgroup, SDH+CSI were more likely to be diagnosed with abuse than Ill-SDH (OR 3.7, 95% CI 1.5-9.2) and Non-ill SDH (10.3, 95% CI 5.0-21.1). Of the 157 subjects with SDH+CSI and no signs of head impact, 88/157 (56%) had non-head/eye related CSIs, including 52/88 (59%) with high specificity fractures and/or multiple fractures, 48/88 (55%) with high specificity bruising. Multiple types of CSIs were in 22/88 (25%).
Conclusion(s): Among children with SDH, AHT is more frequently diagnosed in the presence of CSIs, particularly in the absence of external signs of impact. The high prevalence of CSIs in cases with SDH and no external signs of impact indicates that AHT can occur absent external signs of head impact.
Level of Concern Across Study Defined-Groups
.jpg)
Level of Concern Across Study Defined-Groups with External Contact Head Injury
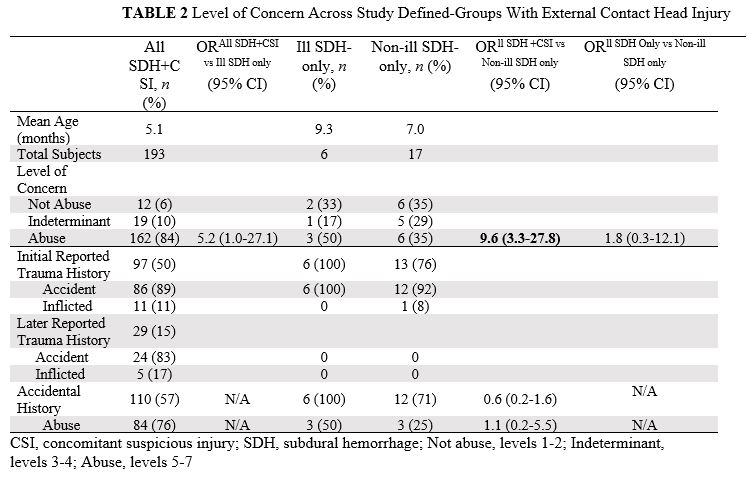
Level of Concern Across Study Defined-Groups Without an External Contact Head Injury