Hospital Medicine 6: Clinical
Session: Hospital Medicine 6: Clinical
538 - Assessing Pediatric Surgeons’ Perceptions of the Enhanced Recovery After Surgery (ERAS) Pathway
Sunday, April 27, 2025
8:30am - 10:45am HST
Publication Number: 538.3687
Rachita Gupta, Children's Hospital Colorado, Aurora, CO, United States; Rachel Torry, Children's Hospital Colorado, Denver, CO, United States; Jason Zamkoff, Children's Hospital Colorado, Denver, CO, United States; Mark Brittan, Children's Hospital Colorado, Aurora, CO, United States; Kyle O.. Rove, Children's Hospital Colorado, Aurora, CO, United States; Sonja I. Ziniel, University of Colorado School of Medicine, Aurora, CO, United States

Sonja I. Ziniel, PhD, MA (she/her/hers)
Associate Professor
University of Colorado School of Medicine
Franktown, Colorado, United States
Presenting Author(s)
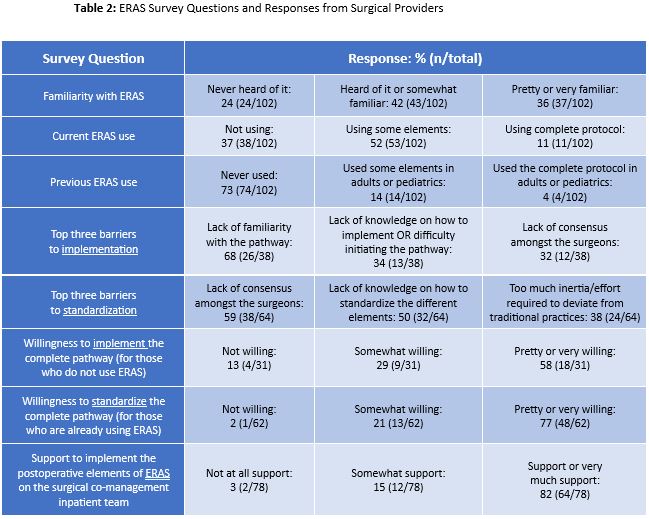
Background: Enhanced Recovery After Surgery (ERAS) is a pathway of standardized pre-, intra-, and postoperative elements that improve operative recovery (Table 1). ERAS has shown benefits in pediatrics by reducing hospital length of stay, opioid use, readmission rates, health care costs and improving patient satisfaction. At our institution, only a few pediatric surgical subspecialties consistently use ERAS. As hospitalists, we aim to work with surgeons to implement ERAS for our shared patients on the surgical co-management inpatient team, and this survey is a first step towards achieving that goal.
Objective: To assess pediatric surgeons’ perceptions of ERAS implementation and standardization for perioperative patients at a tertiary children’s hospital.
Design/Methods: An inter-disciplinary team of hospitalists, surgeons, and a survey methodologist created a de-novo, 35-question survey. The questions were refined to achieve the intended effect via cognitive interviews. A REDCap survey link was emailed to all pediatric surgical providers, including APPs, trainees, and attendings. The survey remained open for 48 days from April to June in 2024 with four follow-up reminders sent to non-responders. Data were analyzed descriptively using frequencies and percentages.
Results: We received 102 out of 345 possible responses (30%). Respondents were mostly orthopedic (23%) and general pediatric surgeons (23%). Nearly half were attendings (43%) and 34% were APPs. Most support or very much support implementing postoperative ERAS on the surgical co-management team (Table 2), but familiarity with ERAS varied, with 24% never having heard of ERAS. This lack of familiarity (68%) and knowledge on how to implement (34%) were the main barriers for ERAS implementation. Barriers for standardization included lack of surgeon consensus (59%) and lack of knowledge on how to standardize (50%). Only 11% reported currently using all of ERAS, 52% using some elements, and 37% not using ERAS at all. 73% had not used ERAS prior to their current role. 58% were pretty or very willing to implement ERAS and 77%, amongst those who were already using it, were pretty or very willing to standardize ERAS for all surgical patients.
Conclusion(s): Most surgeons are in favor of implementing and standardizing the ERAS pathway, especially for their patients on the surgical co-management team. However, most surgical providers are not very familiar with ERAS which is a key barrier to its implementation. These data will guide us in collaborating with various surgical subspecialties to implement ERAS for their patients to improve outcomes and reduce health care costs.
Table 1: Sample Enhanced Recovery After Surgery (ERAS) Pathway
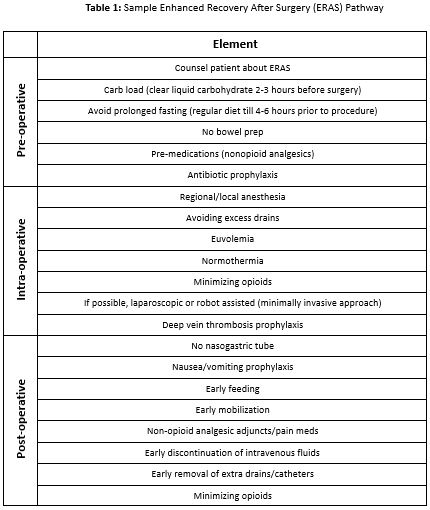
Table 2: ERAS Survey Questions and Responses from Surgical Providers