Back
Background: Hospitalization remains the standard of care for acute illness, but is costly, uncomfortable, and associated with adverse safety events. Moreover, capacity for inpatient pediatric care is declining nationally. Acute hospital care at home – wherein inpatient-level services are delivered in the patient’s home - has emerged as an alternative to conventional hospitalization with comparable, if not better, clinical outcomes, cost-effectiveness and patient experience in adults and internationally. To date, none of the more than 300 programs in the U.S. serve a pediatric population.
Objective: To qualitatively assess the perceptions of patient family caregivers towards pediatric home hospital to inform family-centered design and implementation.
Design/Methods: Semi-structured interviews were performed with a purposive sample of family caregivers of children who were recently hospitalized at an urban freestanding children’s hospital (Boston, MA). Interviews focused on experiences with prior hospitalization along with perceptions of pediatric home hospital, emphasizing potential benefits and challenges. Qualitative data were coded and analyzed by two investigators using grounded theory to discover core themes and sub-themes.
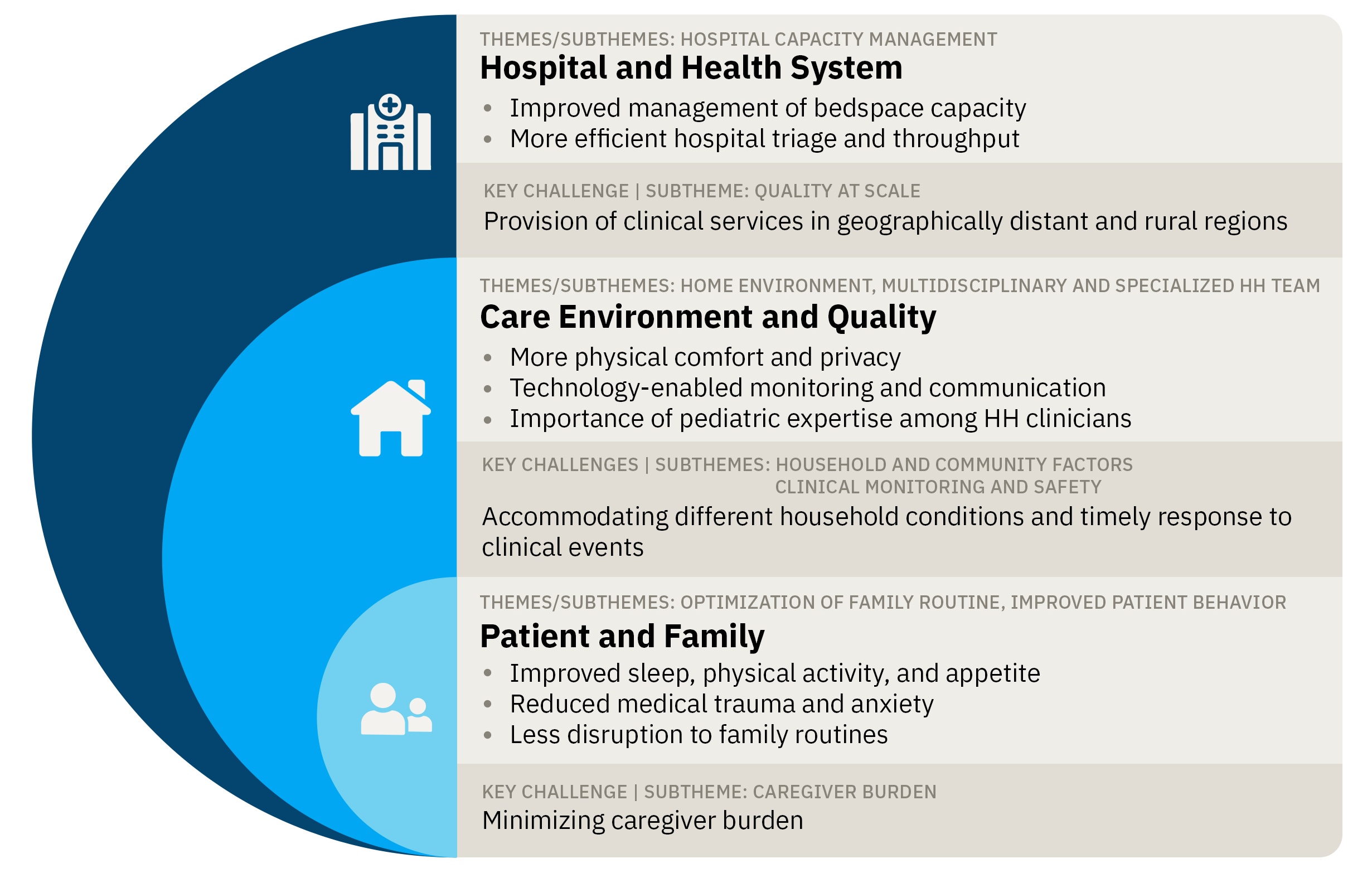
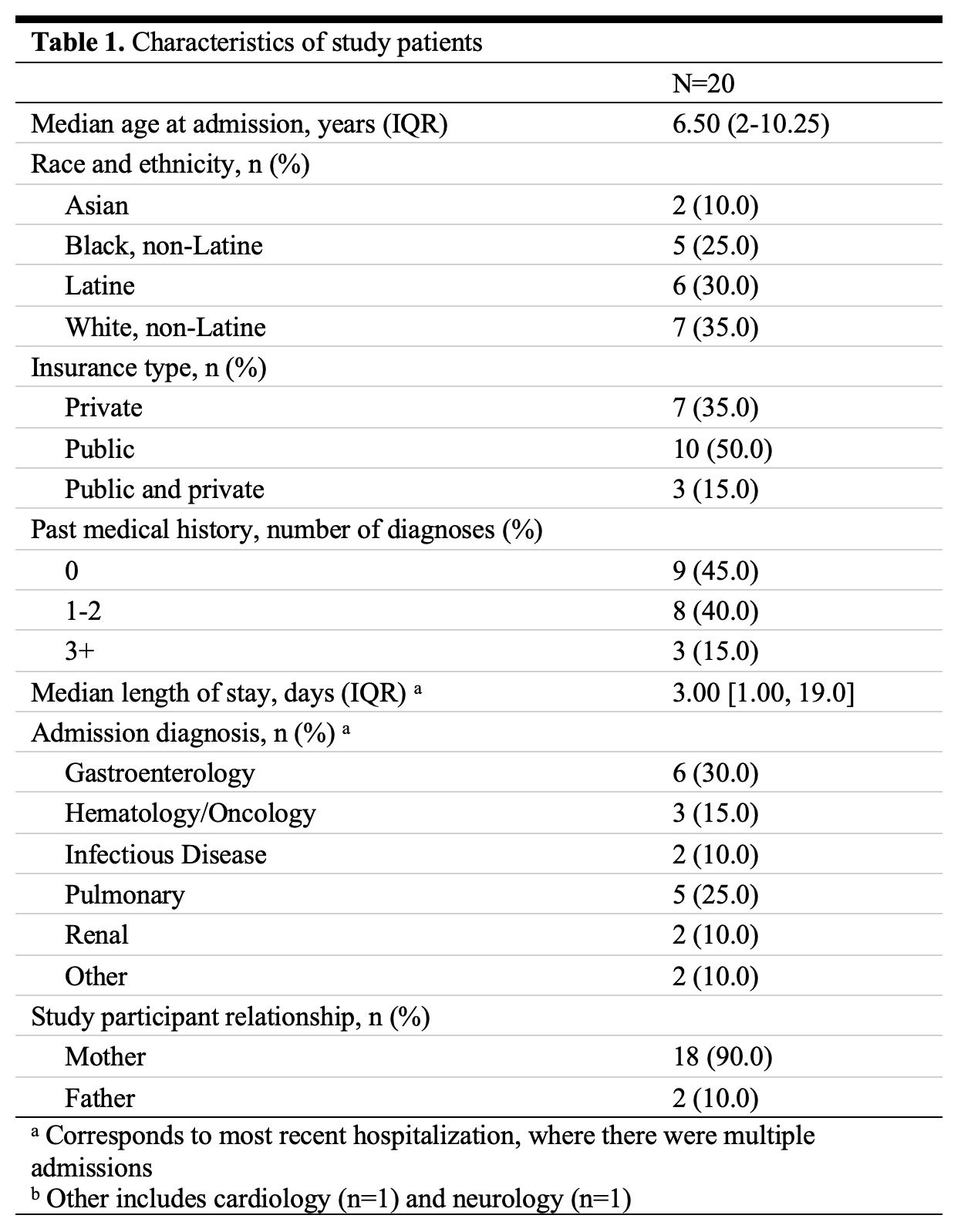
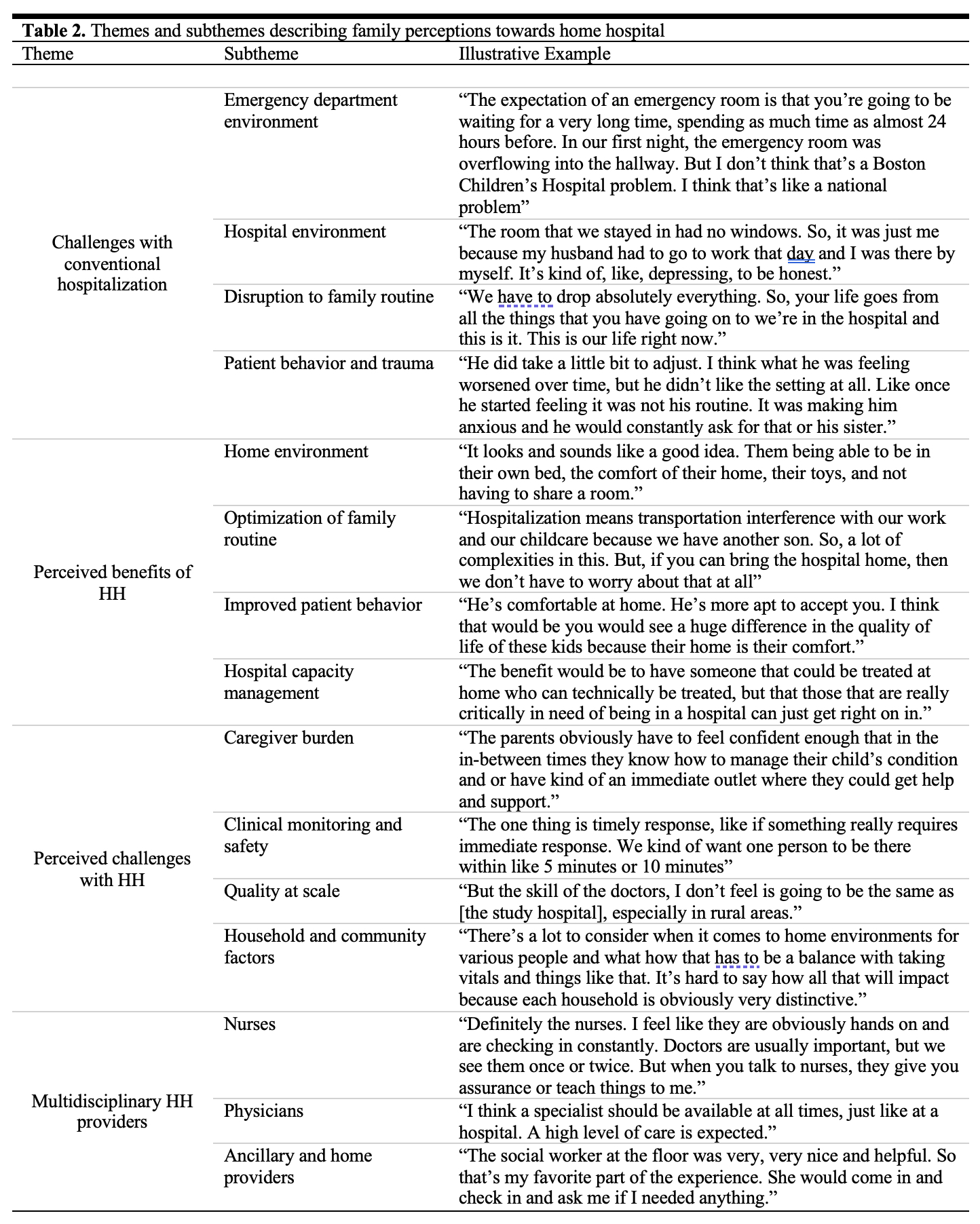
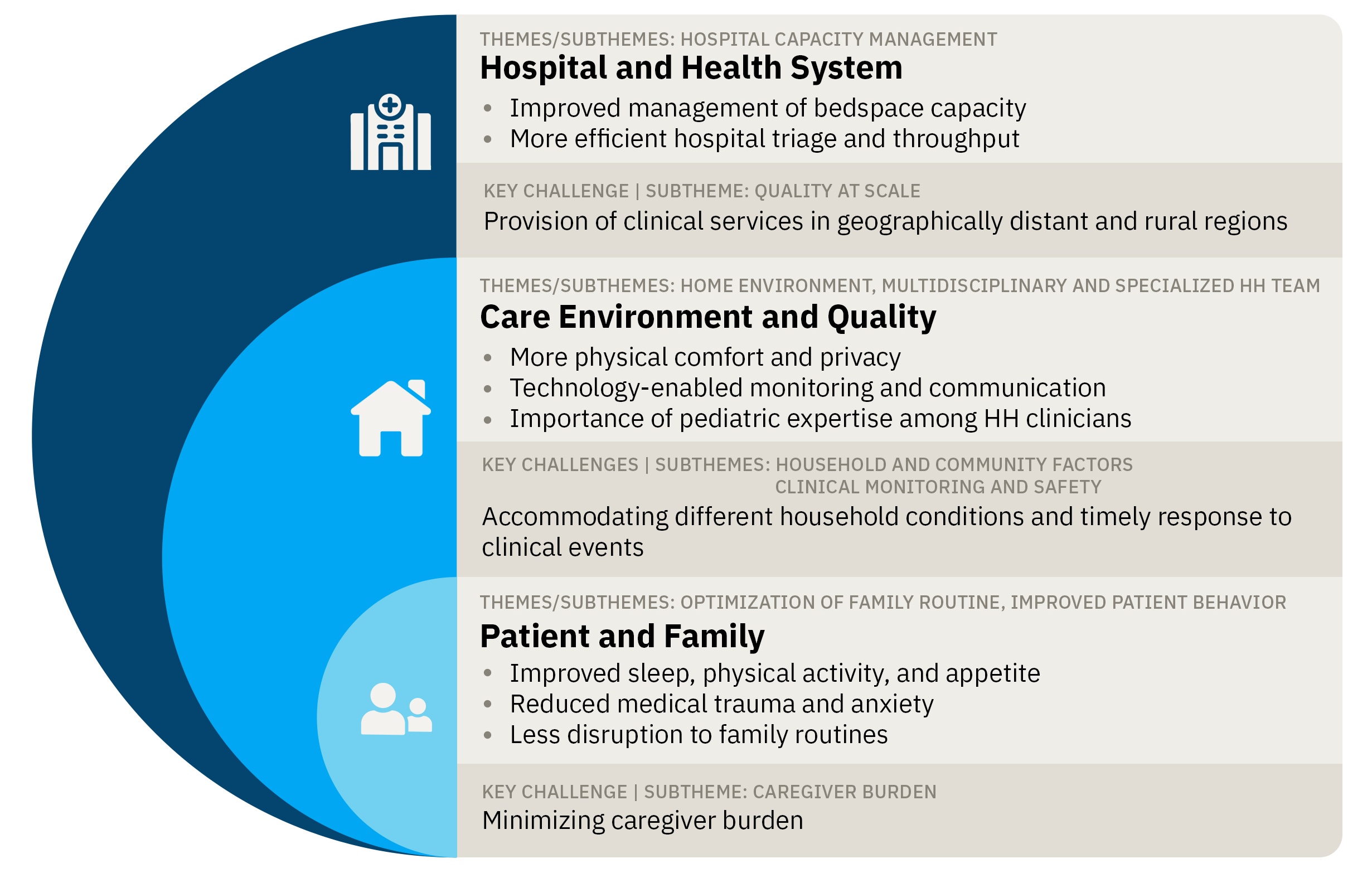
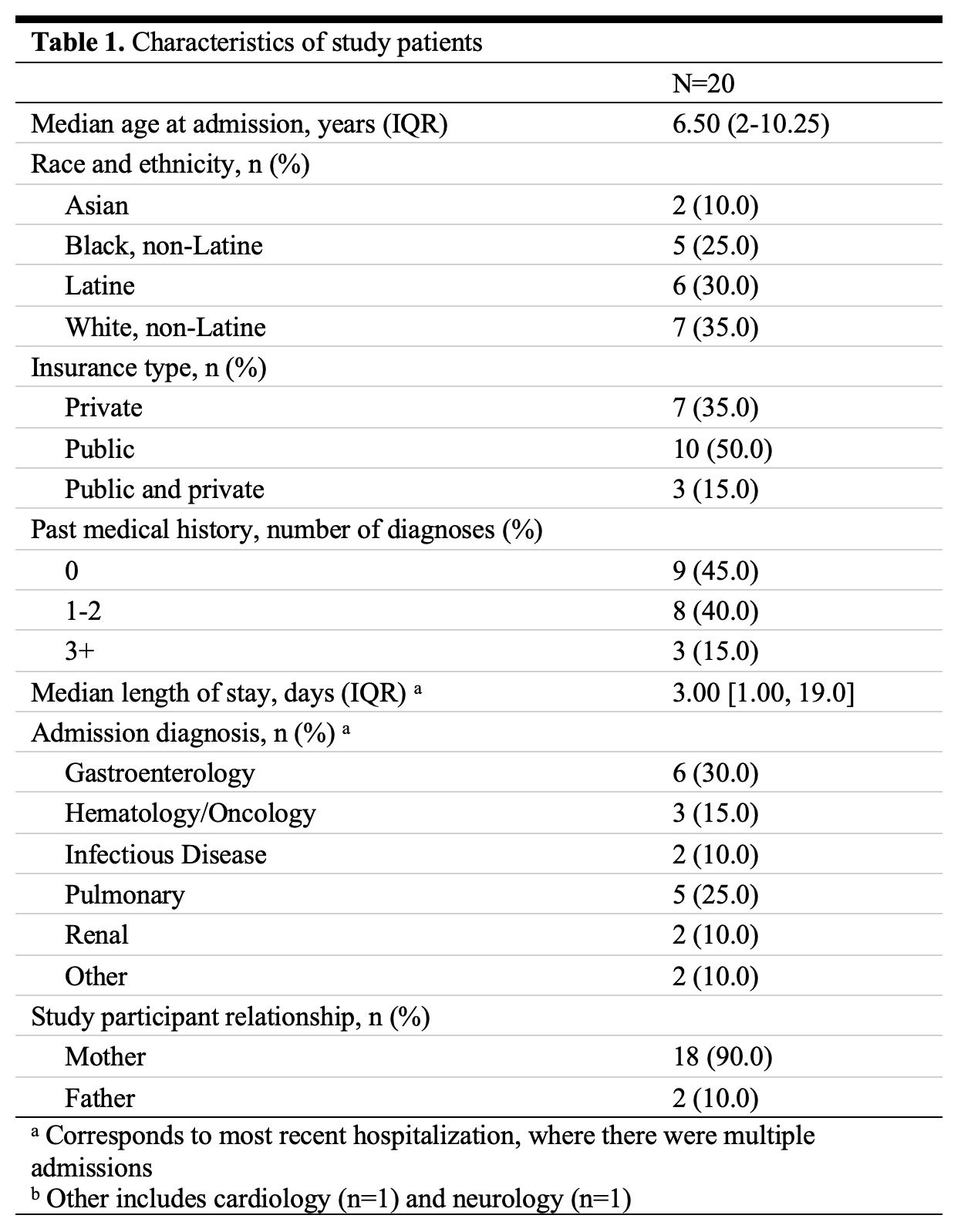
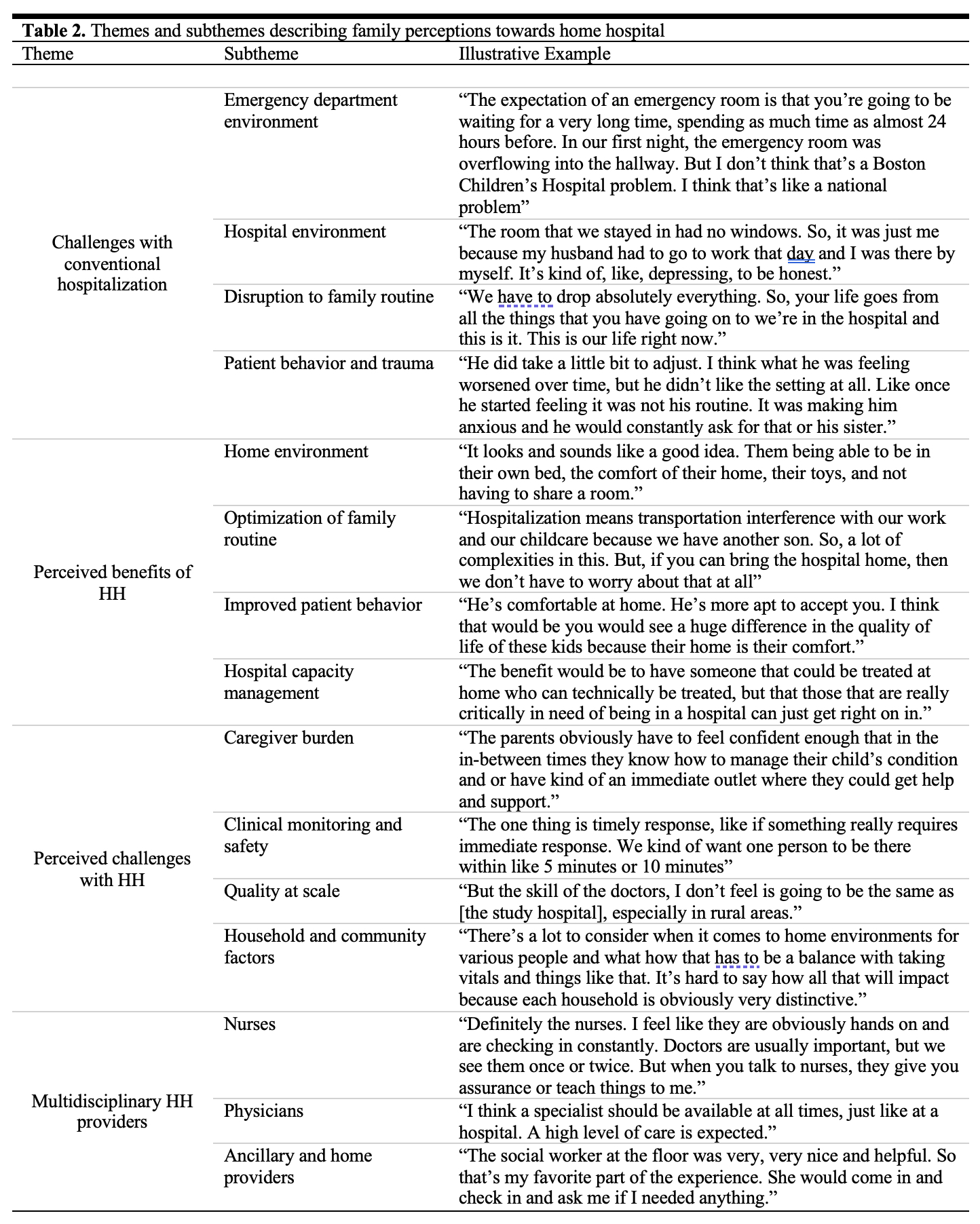
Results: Among 20 family caregivers, the majority were mothers (90%) whose children were a median age of 6.5 years (interquartile range [IQR] 2-10.25) with public insurance (50%), no prior medical history (45%), and a median length of stay of 3 days (IQR 1-19) (Table 1). Four themes emerged: (1) disruptions to family routine and psychosocial stressors were two common challenges experienced during conventional hospitalization; (2) family caregivers were largely receptive to the home hospital concept and described numerous potential benefits, including improved physical comfort, patient behavior, and hospital capacity management; (3) concerns about caregiver burden, clinical monitoring and safety, and scalability to different geographies and household conditions were noted as barriers to home hospital implementation; and (4) participants emphasized the importance of pediatric expertise among home hospital clinicians (Figure 1, Table 2).
Conclusion(s): Family caregivers held positive perceptions towards the HH model. Participants identified numerous potential benefits to the patient, family caregivers, and health system, while emphasizing ongoing questions about safety, accessibility, and quality. Our findings lay the groundwork for designing clinical studies and deploying family-centered pediatric HH programs in the US, ensuring these efforts remain anchored by the input of key stakeholders.
Characteristics of study patients
Themes and subthemes describing family perceptions towards home hospital
Conceptual model of pediatric home hospital benefits and challenges compared to conventional hospitalization
Hospital Medicine 3: Systems/Population-based Research
Session: Hospital Medicine 3: Systems/Population-based Research
142 - Family Perceptions of Pediatric Acute Hospital Care at Home in the US: A Qualitative Analysis
Sunday, April 27, 2025
8:30am – 10:45am HST
Ryan Brewster, Ariadne Labs, Brigham and Women's Hospital, Boston, MA, United States; Roger T. Day, Boston Children's Hospital, Boston, MA, United States; Alex Butler, Boston Children's Hospital, Boston, MA, United States; Elaine J. Lin, Boston Children's Hospital, Wayland, MA, United States; David Levine, Harvard Medical School, Boston, MA, United States; Jay Berry, Complex Care, Boston Children's Hospital, Boston, MA, United States

Ryan Brewster, MD
Resident Physician
Ariadne Labs, Brigham and Women's Hospital
Boston, Massachusetts, United States
Presenting Author(s)
Background: Hospitalization remains the standard of care for acute illness, but is costly, uncomfortable, and associated with adverse safety events. Moreover, capacity for inpatient pediatric care is declining nationally. Acute hospital care at home – wherein inpatient-level services are delivered in the patient’s home - has emerged as an alternative to conventional hospitalization with comparable, if not better, clinical outcomes, cost-effectiveness and patient experience in adults and internationally. To date, none of the more than 300 programs in the U.S. serve a pediatric population.
Objective: To qualitatively assess the perceptions of patient family caregivers towards pediatric home hospital to inform family-centered design and implementation.
Design/Methods: Semi-structured interviews were performed with a purposive sample of family caregivers of children who were recently hospitalized at an urban freestanding children’s hospital (Boston, MA). Interviews focused on experiences with prior hospitalization along with perceptions of pediatric home hospital, emphasizing potential benefits and challenges. Qualitative data were coded and analyzed by two investigators using grounded theory to discover core themes and sub-themes.
Results: Among 20 family caregivers, the majority were mothers (90%) whose children were a median age of 6.5 years (interquartile range [IQR] 2-10.25) with public insurance (50%), no prior medical history (45%), and a median length of stay of 3 days (IQR 1-19) (Table 1). Four themes emerged: (1) disruptions to family routine and psychosocial stressors were two common challenges experienced during conventional hospitalization; (2) family caregivers were largely receptive to the home hospital concept and described numerous potential benefits, including improved physical comfort, patient behavior, and hospital capacity management; (3) concerns about caregiver burden, clinical monitoring and safety, and scalability to different geographies and household conditions were noted as barriers to home hospital implementation; and (4) participants emphasized the importance of pediatric expertise among home hospital clinicians (Figure 1, Table 2).
Conclusion(s): Family caregivers held positive perceptions towards the HH model. Participants identified numerous potential benefits to the patient, family caregivers, and health system, while emphasizing ongoing questions about safety, accessibility, and quality. Our findings lay the groundwork for designing clinical studies and deploying family-centered pediatric HH programs in the US, ensuring these efforts remain anchored by the input of key stakeholders.
Characteristics of study patients
Themes and subthemes describing family perceptions towards home hospital
Conceptual model of pediatric home hospital benefits and challenges compared to conventional hospitalization