Palliative Care
Session: Palliative Care
428 - Decision-Making Communication in Interpreted and English Care Conferences of Seriously Ill Children
Sunday, April 27, 2025
8:30am - 10:45am HST
Publication Number: 428.4239
Aleksandra Olszewski, UPMC Childrens Hospital of Pittsburgh, Pittsburgh, PA, United States; Melissa Martos, University of Washington School of Medicine, Seattle, WA, United States; Blanca Fields, Seattle Children's, Bellevue, WA, United States; Maya JH. Scott, Seattle Children's Hospital, Seattle, WA, United States; K. Casey Lion, University of Washington/ Seattle Children's Hospital, Seattle, WA, United States; Amy C. Trowbridge, University of Washington School of Medicine, Seattle, WA, United States

Aleksandra Olszewski, MD, MA (she/her/hers)
Faculty, Pediatric Critical Care
UPMC Childrens Hospital of Pittsburgh
Pittsburgh, Pennsylvania, United States
Presenting Author(s)
Background: Quality communication is important in medical decision-making (DM), especially for seriously ill patients. Children and families who use language interpretation for care experience disparities in health outcomes and communication. Little is known about how DM conversations occur for different decision types or across caregiver language preference.
Objective: Explore decision types and DM communication for seriously ill children, including describing differences in DM communication in English and interpreted care conferences.
Design/Methods: We conducted a mixed methods analysis of English and interpreted audio-recorded care conference transcripts for pediatric patients with serious illness hospitalized at a single urban, quaternary hospital between January 2018 and January 2021. Codes were developed deductively, based on existing DM frameworks, and inductively from transcripts. Decisions were coded as clinician-guided if made predominantly by clinicians, family-guided if made predominantly by families, and shared if there was a joint decision with input from each group. Descriptive analyses summarized demographics and codes. Mann-Whitney-U and Chi-square tests tested differences in DM by language.
Results: We analyzed 29 care conferences; 11 (39%) were interpreted (8 Spanish, 2 Vietnamese, 1 Somali). There were 162 DM instances (109 English, 53 interpreted), with means of 6.1 DM per English conference vs. 4.5 DM per interpreted conference (p=0.049). DM types included 34% big picture, 36% day-to-day, 26% forward-thinking, and 2% logistical or non-medical decisions (Figure 1). DM was 60% clinician-guided, 14% family-guided, and 22% shared (Figures 1, 2). The presence of a decision to be made was labeled explicitly 46% of the time, and DM was explicitly labeled as shared 30% of the time (Figure 3). DM was initiated by parents 31% of the time (Figure 3). Family’s desired DM role was elicited 7% of the time. These trends were similar across care conference types by language (Figures 2, 3).
Conclusion(s): Decisions are discussed significantly less often in interpreted pediatric care conferences than in English ones. Decision types were widely variable and primarily clinician-guided. However, clinicians were infrequently explicit about DM occurring, and even less frequently explicit about sharing the decision or eliciting families’ desired DM roles. Future work ought to explore best practices, including family preferences, for DM communication across decision types and by family language.
Figure 1.
.jpg) Coding schematic with examples and exemplar quotes for each of the major codes.
Coding schematic with examples and exemplar quotes for each of the major codes.Figure 2.
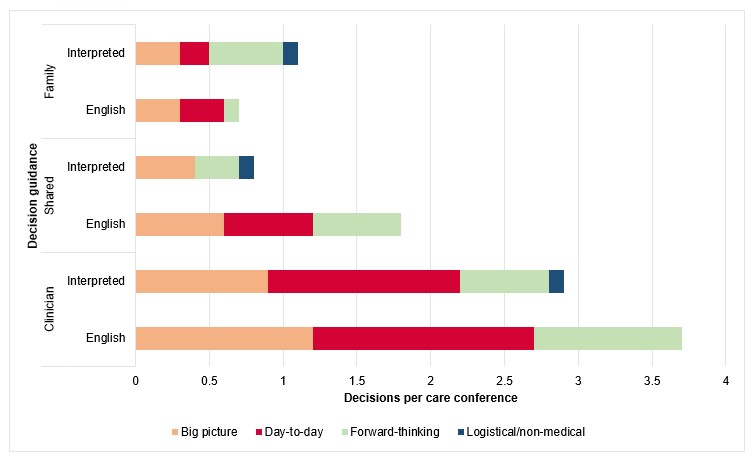 Number of decisions per care conference, by conference type (n= 18 (English); n=11 (interpreted)), decision type, and decision guidance.
Number of decisions per care conference, by conference type (n= 18 (English); n=11 (interpreted)), decision type, and decision guidance.Figure 3.
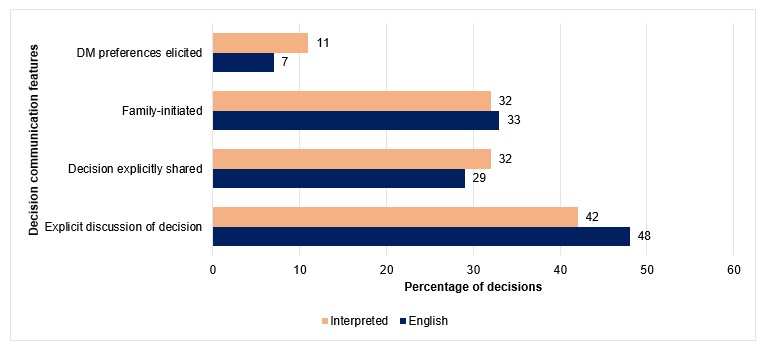 Percentage of decisions per care conference type (n=109 for English, n=53 for interpreted), by the following decision communication features: decision-making preferences elicited (p=0.4), decisions explicitly described (p=0.5), decisions explicitly described as shared (p=0.7), and decisions family-initiated (p=0.9).
Percentage of decisions per care conference type (n=109 for English, n=53 for interpreted), by the following decision communication features: decision-making preferences elicited (p=0.4), decisions explicitly described (p=0.5), decisions explicitly described as shared (p=0.7), and decisions family-initiated (p=0.9).
