Hospital Medicine 5: Clinical
Session: Hospital Medicine 5: Clinical
525 - Development and Validation of a Predictive Clinical Calculator for Invasive Bacterial Infection in Febrile Infants Aged 8-60 Days
Sunday, April 27, 2025
8:30am - 10:45am HST
Publication Number: 525.4243
Jared Kusma, Phoenix Children's, Phoenix, AZ, United States; Jacob Phouthavong-Murphy, Phoenix Children's Hospital, Tempe, AZ, United States; Maheshwor Kafle, Phoenix children’s hospital, Phoenix, AZ, United States; Quinney Fu, Phoenix Children's, Phoenix, AZ, United States; Andrew Ritchey, Phoenix Children's Hospital, Mesa, AZ, United States; Lucia Mirea, Phoenix Children's, Phoenix, AZ, United States; Jillian Wall, Phoenix Children's Hospital, Phoenix, AZ, United States; Jennifer Stamp, Phoenix Children's Hospital, Phoenix, AZ, United States; Ashley Bartlett, Phoenix Children's Hospital, Scottsdale, AZ, United States; Richard Engel, Phoenix Children's Hospital, Phoenix, AZ, United States; Sandra Gage, Phoenix Children's Hospital, Racine, WI, United States

Jared Kusma, MD, MS-CR (he/him/his)
Pediatric Hospitalist
Phoenix Children's
Phoenix Children's Hospital
Phoenix, Arizona, United States
Presenting Author(s)
Background: Febrile infants 8-60 days-old are at high risk for invasive bacterial infections (IBI), defined as bacteremia and meningitis. Existing guidelines use factors such as patient appearance, age, urinalysis (UA) results, and inflammatory marker cut-offs to assess IBI risk, and prior prediction tools have incorporated these factors with variable results. No reliable prediction tool exists to aid in clinical decision making.
Objective: 1). Develop and validate a clinical calculator predicting IBI risk in febrile infants aged 8-60 days
Design/Methods: Retrospective cohort study of infants 8-60 days-old presenting to a tertiary children’s hospital with objective fever ≥38°C between 1/1/2018-12/31/2023. Infants identified via ICD-10 codes for fever, IBI or urinary tract infection (UTI). Exclusion criteria: prematurity ( < 37 weeks), previous admission to intensive care, prior antibiotic use, non-IBI/UTI bacterial infection, or complex care needs. Collected data: age, procalcitonin (PCT), absolute neutrophil count (ANC), UA, and blood/cerebrospinal (CSF) culture results. Blood or CSF culture growth was required to be considered IBI+ (documented as non-contaminant). Positive UA defined as: urinary white blood cell count>5, positive leukocyte esterase, or positive nitrites. Training (80%) and testing (20%) data sets were created via stratified random sampling. Univariable logistic regression (ULR) identified predictive variables in the training data, and a multivariable logistic regression (MLR) model was developed. Internal validation using the testing data estimated the adjusted AUC and Brier score, and compared IBI+ vs. IBI- median risk via Wilcoxon rank sum test.
Results: Of 3,682 patients identified, 2,073 (56.3%) met inclusion criteria of which 57 (2.75%) had IBI. The final multivariable calculator retained PCT, ANC, positive UA, and age as predictors (Table 1). Internal validation demonstrated significantly higher median risk in IBI+ vs. IBI- infants [92.01 vs. 10.84; p-value < 0.01] (Table 2) with AUC [95% CI] = 0.93 [0.88, 0.98] and Brier score of 0.03.
Conclusion(s): In febrile infants 8-60 days-old, our prediction calculator identified infants at higher risk of IBI using basic lab results and age, with a high degree of accuracy as indicated by our high AUC and low Brier score. The calculator is promising for aiding clinicians in early, accurate risk assessment for IBI, potentially optimizing treatment decisions and resource use. Given the single-center design and low IBI case count, external multicenter validation is critical to confirm its broader applicability.
Table 1: Multivariable Predictors of Invasive Bacterial Infection via Logistic Regression, Using the Training Data Set.
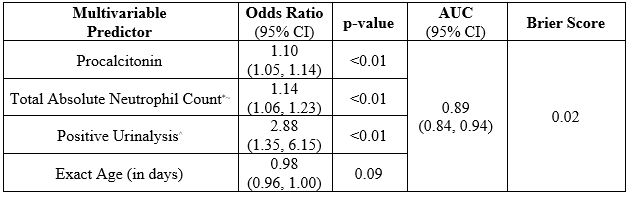 *: Total Absolute Neutrophil Count = Absolute Neutrophil Count + Band Count
*: Total Absolute Neutrophil Count = Absolute Neutrophil Count + Band Count ~: 1/1000th scale
^: Positive Urinalysis = Urinary White Blood Cell Count >5 or positive Leukocyte Esterase or positive Nitrites
AUC: Area Under the Curve, CI: Confidence Interval
Table 2: Internal Validation of the Clinical Calculator on the Test Data Set
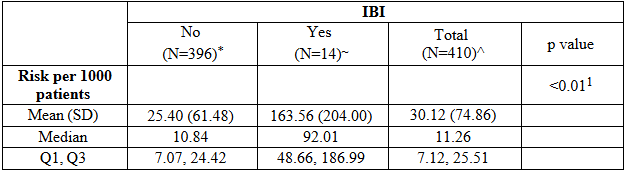 *: 3 patients missing a least 1 data point
*: 3 patients missing a least 1 data point ~: 1 patient missing at least 1 data point
^: 4 patients missing at least 1 data point
1: Wilcoxon rank sum test
SD: Standard Deviation, IBI: Invasive Bacterial Illness, Q1: First Quartile, Q2: Second Quartile

