Gastroenterology/Hepatology
Session: Gastroenterology/Hepatology
323 - COVID-19 Infection is Not Associated with Incident Diagnosis of Celiac Disease
Sunday, April 27, 2025
8:30am - 10:45am HST
Publication Number: 323.4242
Cade M. Nylund, Uniformed Services University of the Health Sciences F. Edward Hebert School of Medicine, Bethesda, MD, United States; Sarah Prabhakar, Uniformed Services University of the Health Sciences F. Edward Hebert School of Medicine, Bethesda, MD, United States; Rian C. Calo, Uniformed Services University of the Health Sciences F. Edward Hebert School of Medicine, Kensinton, MD, United States; Apryl Susi, Uniformed Services University of the Health Sciences F. Edward Hebert School of Medicine, Bethesda, MD, United States

Cade M. Nylund, MD
Professor of Pediatrics
Uniformed Services University of the Health Sciences F. Edward Hebert School of Medicine
Bethesda, Maryland, United States
Presenting Author(s)
Background: The COVID-19 pandemic and COVID-19 infection have been linked to immune-mediated diseases. It is not known whether COVID-19 infection is associated with the development of celiac disease (CD).
Objective: This study evaluates the causal relationship between COVID-19 infection and incident diagnosis of CD.
Design/Methods: A propensity score-matched retrospective cohort study using the Military Health System (MHS) Database data for children 0-17 years of age was performed. ICD-10 codes and laboratory test results identified patients with COVID-19 infections from July 2020 to June 2021. Counts of inpatient and outpatient diagnoses, procedures, and outpatient medication prescription data one year preceding COVID-19 infection were categorized by a clinical classification software. Using 1770 clinical variables, a propensity score for COVID-19 infection was matched 1:2 to non-exposed, additionally matched on age, sex, and month of the year.. The cohort was followed for a diagnosis of CD and separately for any esophagogastroduodenoscopy (EGD). Any subject and their controls with an ICD-10 code indicating the outcome in the year prior to their cohort entry date was excluded. Participants were followed for a year with censoring at loss to follow-up or COVID-19 infection or a diagnosis of CD. Cox Proportional Hazards Model was used to generate hazard ratios (HR).
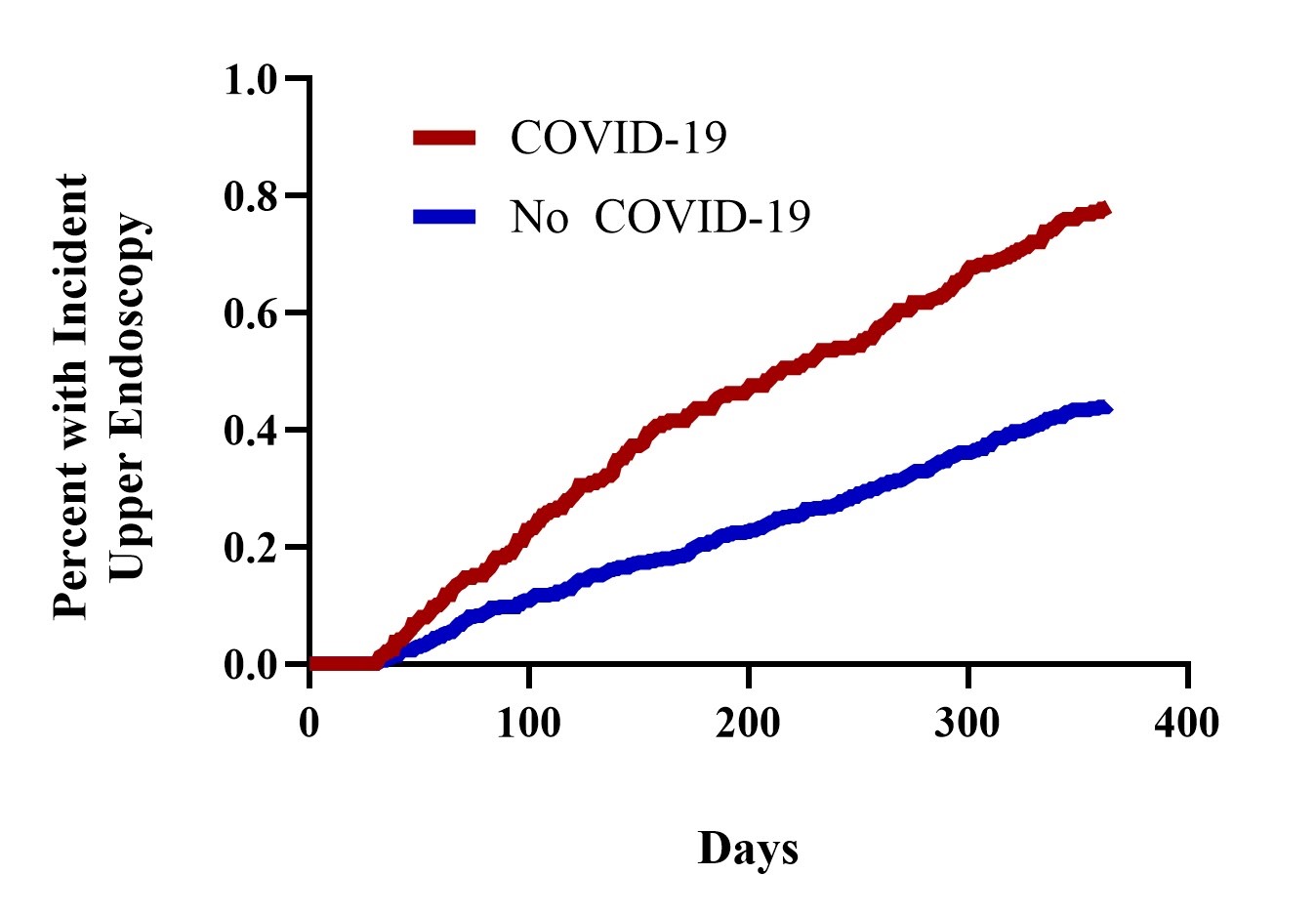
Results: There were 72,027 total participants in the study, 24,009 with COVID-19 exposure and 48,018 controls. 53.3% were female and the median age was 11 (interquartile range [IQR], 5-15). Children with COVID-19 were more likely to have an EGD (HR, 1.74; 95% confidence interval[CI], 1.43-2.13; N=384). There were 54 total subjects with CD for the first time; 21 (0.09%) among those with COVID-19 and 33 (0.07%) among controls. Of those with CD the median age was 13 years (IQR, 8-15) and 64.8 % were females (n= 35). Children who had a recorded diagnosis of COVID-19 were not more likely to have a new diagnosis of CD (HR, 1.22; 95% CI, 0.70-2.16).
Conclusion(s): Children 0-17 years of age diagnosed with COVID-19 were more likely to have an EGD but were not more likely to be diagnosed with CD. However, our study suggests that children with COVID-19 may have more post-COVID-19 gastrointestinal symptoms leading to evaluation with an EGD. The study was limited by a low number of CD patients and future larger studies, possibly including a longer follow-up period and young adults would be warranted.
Figure 1 Cumulative Percent of Subjects with a Newly Diagnosed Celiac Disease by COVID-19 Exposure Status
.png)
Figure 2 Cumulative Percent of Subjects with an Esophagogastroduodenoscopy by COVID-19 Exposure Status