Hospital Medicine 5: Clinical
Session: Hospital Medicine 5: Clinical
524 - Canadian practice patterns in the management of pediatric periorbital and orbital cellulitis: a national survey
Sunday, April 27, 2025
8:30am - 10:45am HST
Publication Number: 524.4266
Carsten Krueger, Children's Hospital, Calgary, AB, Canada; Emily Nguyen, The Hospital for Sick Children, Toronto, ON, Canada; Shamama Raza, The Hospital for Sick Children, Toronto, ON, Canada; Sanjay Mahant, The Hospital for Sick Children, Toronto, ON, Canada; Adrienne L. Davis, The Hospital for Sick Children, Toronto, ON, Canada; Ann Bayliss, Trillium Health Partners, Mississauga, ON, Canada; Mahmoud Sakran, Lakeridge Health Oshawa. Queen’s University, Whitby, ON, Canada; Arun Reginald, Hospital for Sick Children, Toronto, Aurora, ON, Canada; Nikolaus Wolter, Hospital for Sick Children, Toronto, ON, Canada; Peter Gill, The Hospital for Sick Children, Toronto, ON, Canada; Patricia M.. Parkin, university, Toronto, ON, Canada

Carsten Krueger, MD FRCPC (he/him/his)
Infectious Diseases Consultant
Alberta Children's Hospital
Calgary, Alberta, Canada
Presenting Author(s)
Background: Periorbital and orbital cellulitis are common infections in the pediatric population requiring interdisciplinary management. However, there are no Canadian clinical practice guidelines to evaluate and manage these severe orbital infections, and wide variation in care.
Objective: To describe clinical practice patterns in admission, diagnostic tests, antibiotic therapy, subspecialty consultation, and discharge recommendations across Canadian hospitals.
Design/Methods: A cross-sectional survey of general pediatricians at children’s and community hospitals across Canada, and pediatric emergency department (ED) physicians at children’s hospitals was conducted. The survey was distributed through Canadian Paediatric Inpatient Research Network (PIRN), and completed by one representative per hospital. Site-level clinical management specific to each provider type was assessed. Data were analyzed descriptively.
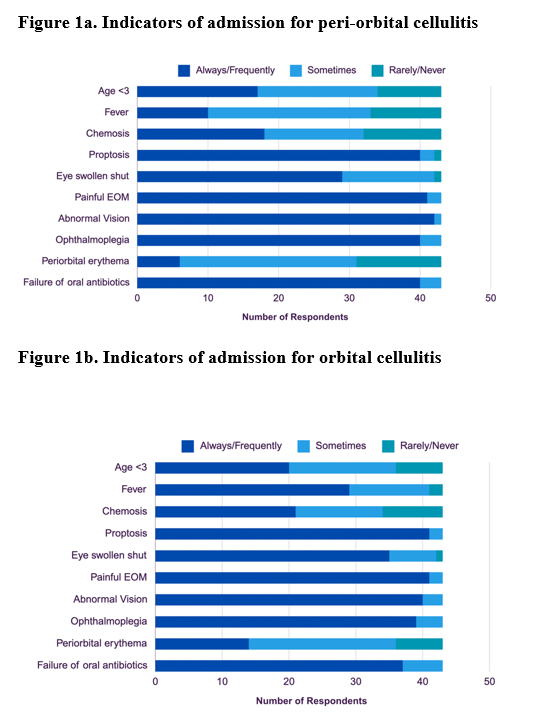
Results: Of 59 individuals contacted, 43 responded (72.9%) of which 19 (44.2%) were community hospital pediatricians, 13 (30.2%) were children’s hospitals pediatricians, and 11 (25.6%) were pediatric ED physicians. Only one hospital had a comprehensive clinical practice guideline. The most frequently ordered tests in the ED were CBC (81.9%) and CRP (81.9%) (Table 1). Abnormal vision and painful extra-ocular movements were indicators for admission. For admitted children, CT scans were ordered ‘always or frequently’ by 46.2% of children’s hospital pediatricians and 5.3% of community hospital pediatricians. Ophthalmology (n=11, 84.6%), otolaryngology (n=9, 69.2%), and infectious diseases (n=6, 46.2%) were frequently consulted at children’s hospitals. Patients with periorbital cellulitis who did not require admission were usually discharged home on oral cephalexin. For admitted periorbital cellulitis patients requiring IV antibiotics, first-generation and third-generation cephalosporin monotherapy were used equally (Table 2). For admitted patients with orbital cellulitis, the most routinely used empiric IV antibiotics included a third-generation cephalosporin with anti-anerobic and anti-staphylococcal agents.
Conclusion(s): There is no consensus on diagnostic test usage, subspeciality consultation, and empiric antibiotic therapy for severe orbital infections. This survey provides important data on health system level usage that highlights the need to develop a Canadian clinical practice guideline is needed to help standardize management.
Table 1
.png)
Table 2
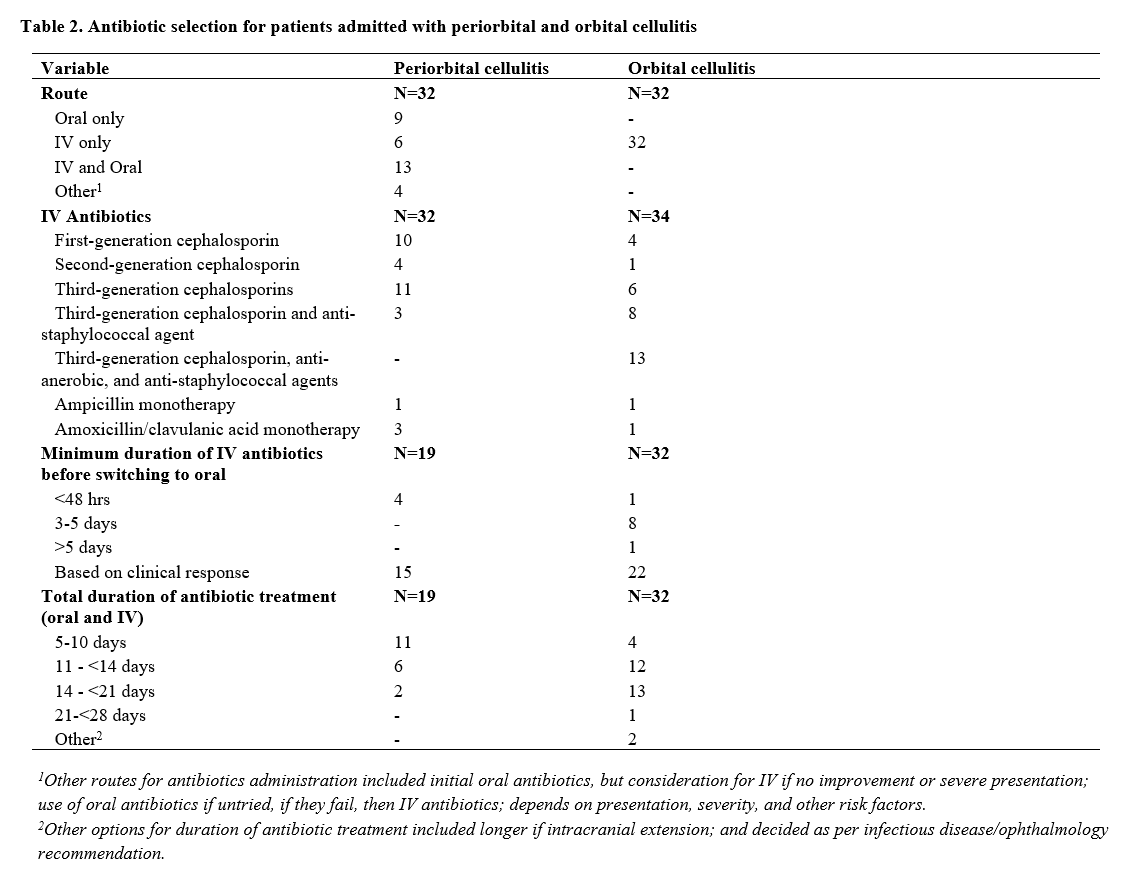
Figure 1a and 1b