Health Equity/Social Determinants of Health 4
Session: Health Equity/Social Determinants of Health 4
697 - Evaluating the Impact of a Pediatric Aerodigestive Clinic on At-Risk Neighborhoods Using the Childhood Opportunity Index: A Retrospective Analysis
Sunday, April 27, 2025
8:30am - 10:45am HST
Publication Number: 697.4594
Natalia N. Youssef, Albany Medical College, Albany, NY, United States; Julie Khlevner, Columbia University Vagelos College of Physicians and Surgeons, New York, NY, United States
.jpeg.jpg)
Natalia N. Youssef (she/her/hers)
Medical Student
Albany Medical College
Albany, New York, United States
Presenting Author(s)
Background: The Pediatric Aerodigestive Clinic (ADC) at Columbia University Irving Medical Center provides coordinated care to medically fragile children with complex gastrointestinal, respiratory and otolaryngology conditions from regions with significant linguistic barriers, low income, and low adult education levels. While prior studies have demonstrated numerous positive impacts of aerodigestive programs, there is limited data on the impact of an ADC on neighborhoods with linguistic barriers and low education levels. To quantify barriers faced by pediatric patients, the Childhood Opportunity Index (COI) compiles education, health/environment, and social/economic data from U.S. neighborhoods and categorizes zip codes into five levels: "very low" (VL), "low" (L), "moderate" (M), "high" (H), and "very high" (VH).
Objective: We sought to examine whether social determinants of health, as determined by COI levels, impact clinical outcomes in patients referred to the ADC from January 2022 to December 2023.
Design/Methods: A retrospective chart review was conducted on 144 patients (Table 1) seen at the ADC during the study period, with 27 meeting inclusion criteria of relevant medical records at least 1 year before and after initial ADC evaluation. COI levels were combined into two cohorts: “Low” (VL+L) and “High” (M+H+VH). Clinical outcomes were examined 1 year before and after the initial ADC visit, as indicated by number of emergency room (ER) visits, hospitalizations, and Δ weight-for-age percentile (WAP) Z-score (Figure 1A-C).
Results: The “High” cohort showed improvement 1-year post-initial ADC visit in the number of ER visits (-38.7%), hospitalizations (-45.9%), and mean ΔWAP Z-score (+966.7%) compared to 1-year pre-initial ADC visit. Conversely, the “Low” cohort experienced a reduction in hospitalizations (-33.7%) but saw an increase in ER visits (+20%) and a decrease in mean ΔWAP Z-score (-66.7%) 1-year post-initial ADC visit. A trend suggests that a higher COI level may lead to better clinical outcomes in a cohort of patients referred to Columbia’s ADC.
Conclusion(s): Further research with a larger cohort size is needed to draw statistically significant conclusions to support these trends. Collaborating with other ADC clinics nationwide who care for neighborhoods with low COI may achieve this. This study highlights the importance of ADC teams managing complex patient populations to be aware that those from lower COI levels may not benefit as much from the intervention of an ADC. Identifying resources to address specific barriers contributing to outcome disparities in low COI neighborhoods is crucial for ADC teams.
Table 1. Demographics of Study Participants
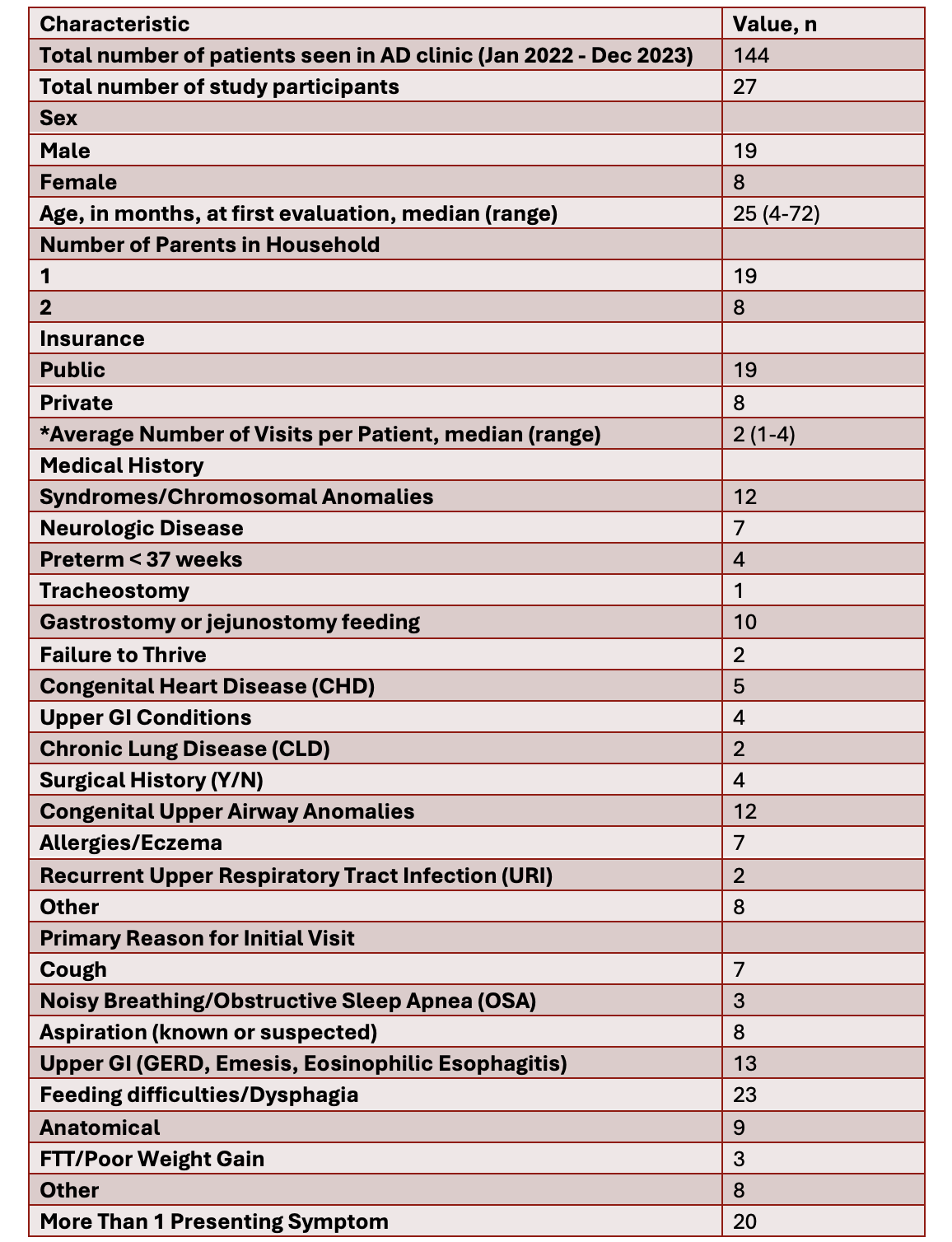 *During study period from January 2022 - December 2023.
*During study period from January 2022 - December 2023.Clinical Outcomes 1-Year Pre- vs Post-Initial ADC Visit (ER Visits, Hospitalizations, and ∆WAP Z-Scores).
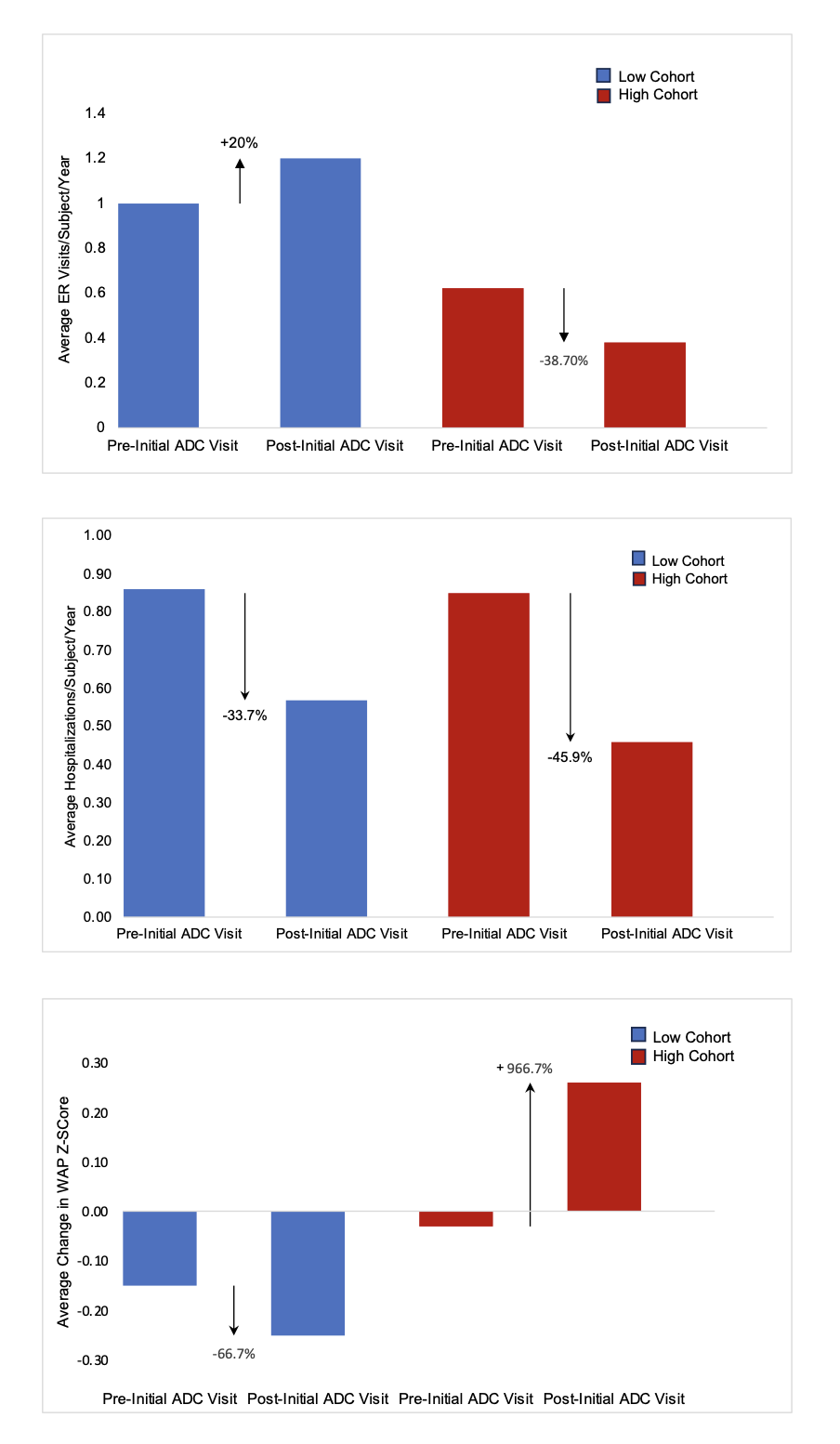 Figure 1: (a) Percentile Change in Average ER visits/subject/year by COI Level (1 Year pre- vs. post-ADC Initial Visit). (b) Percentile Change in Average Hospitalization visits/subject/year by COI Level (1 Year pre- vs. post-ADC Initial Visit). (c) Percentile Change in Average ∆WAP Z-Scores by COI Level (1 Year pre- vs. post-ADC Initial Visit).
Figure 1: (a) Percentile Change in Average ER visits/subject/year by COI Level (1 Year pre- vs. post-ADC Initial Visit). (b) Percentile Change in Average Hospitalization visits/subject/year by COI Level (1 Year pre- vs. post-ADC Initial Visit). (c) Percentile Change in Average ∆WAP Z-Scores by COI Level (1 Year pre- vs. post-ADC Initial Visit).Table 1. Demographics of Study Participants
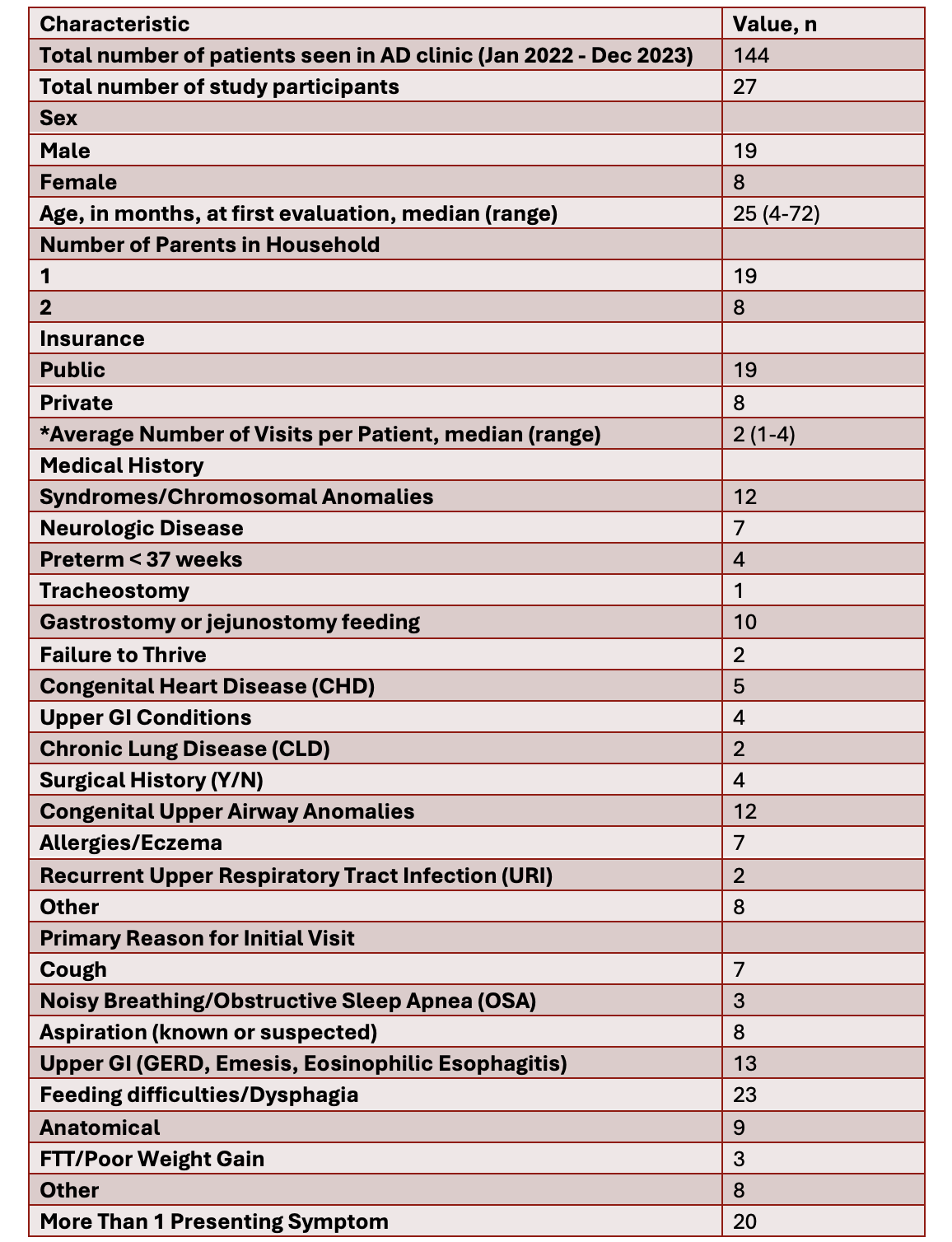 *During study period from January 2022 - December 2023.
*During study period from January 2022 - December 2023.Clinical Outcomes 1-Year Pre- vs Post-Initial ADC Visit (ER Visits, Hospitalizations, and ∆WAP Z-Scores).
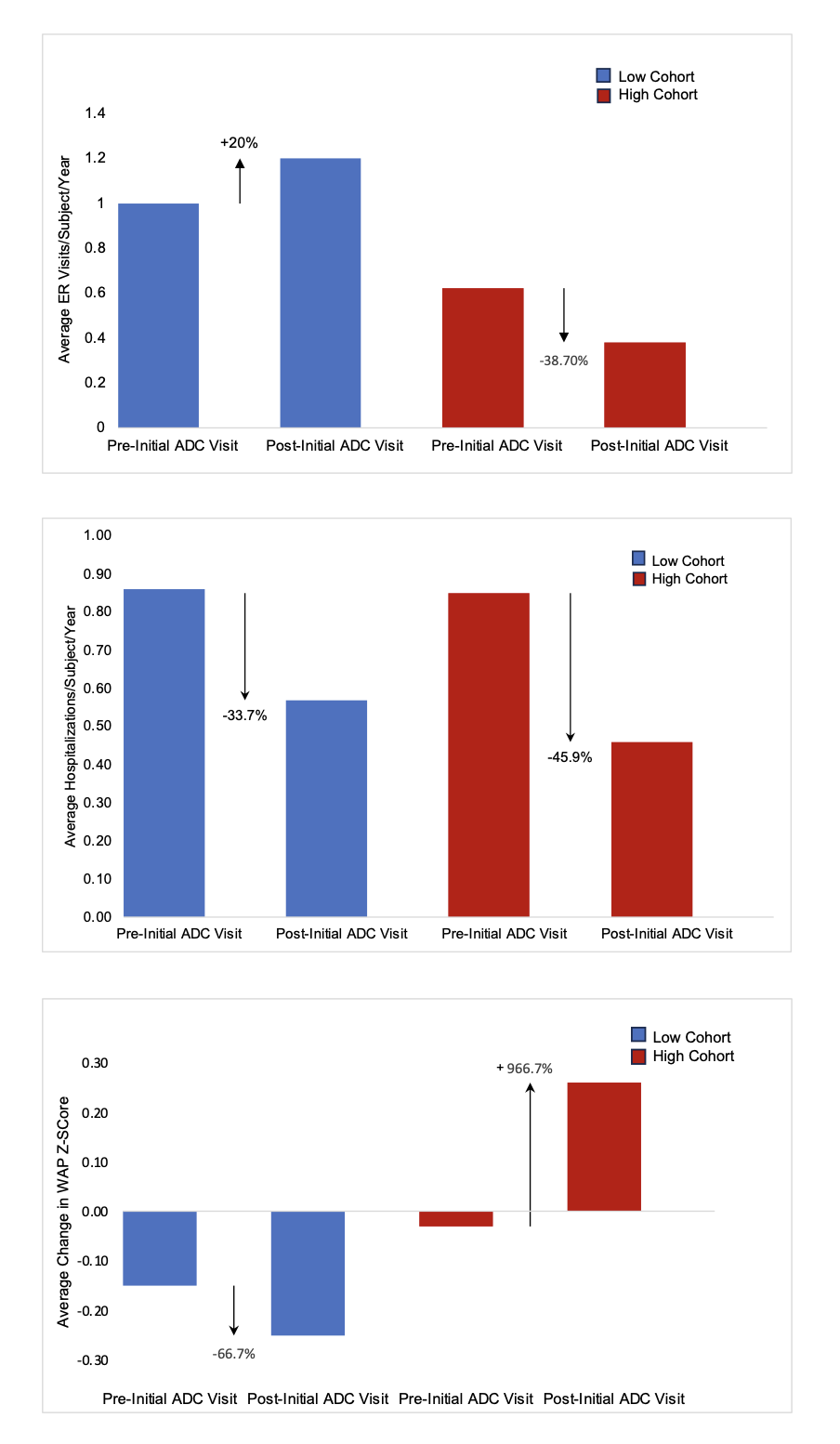 Figure 1: (a) Percentile Change in Average ER visits/subject/year by COI Level (1 Year pre- vs. post-ADC Initial Visit). (b) Percentile Change in Average Hospitalization visits/subject/year by COI Level (1 Year pre- vs. post-ADC Initial Visit). (c) Percentile Change in Average ∆WAP Z-Scores by COI Level (1 Year pre- vs. post-ADC Initial Visit).
Figure 1: (a) Percentile Change in Average ER visits/subject/year by COI Level (1 Year pre- vs. post-ADC Initial Visit). (b) Percentile Change in Average Hospitalization visits/subject/year by COI Level (1 Year pre- vs. post-ADC Initial Visit). (c) Percentile Change in Average ∆WAP Z-Scores by COI Level (1 Year pre- vs. post-ADC Initial Visit).
