Global Neonatal & Children's Health 5
Session: Global Neonatal & Children's Health 5
784 - Donor Human Milk in Ethiopian NICUs: Pre-Implementation Perspectives from Neonatal Intensive Care Providers in Addis Ababa
Sunday, April 27, 2025
8:30am - 10:45am HST
Publication Number: 784.4585
Sharla Rent, Duke University School of Medicine, Durham, NC, United States; Merhawit Abadi, Saint Paul's Hospital Millennium Medical College, ADDIS ABABA, Adis Abeba, Ethiopia; Krystle M.. Perez, University of Washington, Seattle, WA, United States; Gregory C.. Valentine, University of Washington School of Medicine, Tacoma, WA, United States; Olivia C. Brandon, University of Washington: Magnuson Health Sciences Center – RR 544A, Seattle, WA, United States; Gal Barbut, Golisano Children's Hospital at The University of Rochester Medical Center, Rochester, NY, United States; Redeat Workneh, St Paul's Hospital Millennium Medical College, Addis Ababa, Ethiopia, Adis Abeba, Ethiopia; Mahlet Abayneh, St Paul's Hospital Millennium Medical College, Addis ABABA, Adis Abeba, Ethiopia

Sharla Rent, MD, MScGH (she/her/hers)
Assistant Professor of Pediatrics
Duke University School of Medicine
Durham, North Carolina, United States
Presenting Author(s)
Background: For small and sick newborns (SSNBs), recommendations emphasize providing mother’s own milk (MOM) or donor human milk (DHM) if MOM is not available (e.g. if mothers are too ill or die during childbirth). Only 7 out of 54 African countries have DHM programs; Ethiopia, which ranks in the top 10 countries globally for neonatal mortality, is not amongst them.
Objective: We sought to describe existing knowledge and beliefs of medical providers in an Ethiopian Neonatal Intensive Care Unit (NICU) regarding the use of DHM to nourish SSNBs as part of a pre-implementation assessment for establishing a DHM program at St Paul’s Hospital Millenium Medical College (SPHMMC).
Design/Methods: We recruited NICU providers via purposive sampling to ensure representation of physicians, nurses, midwives, and other providers. All providers completed a one-time survey about perceptions and practices related to DHM use in the NICU. Descriptive statistics were utilized for demographic and response data.
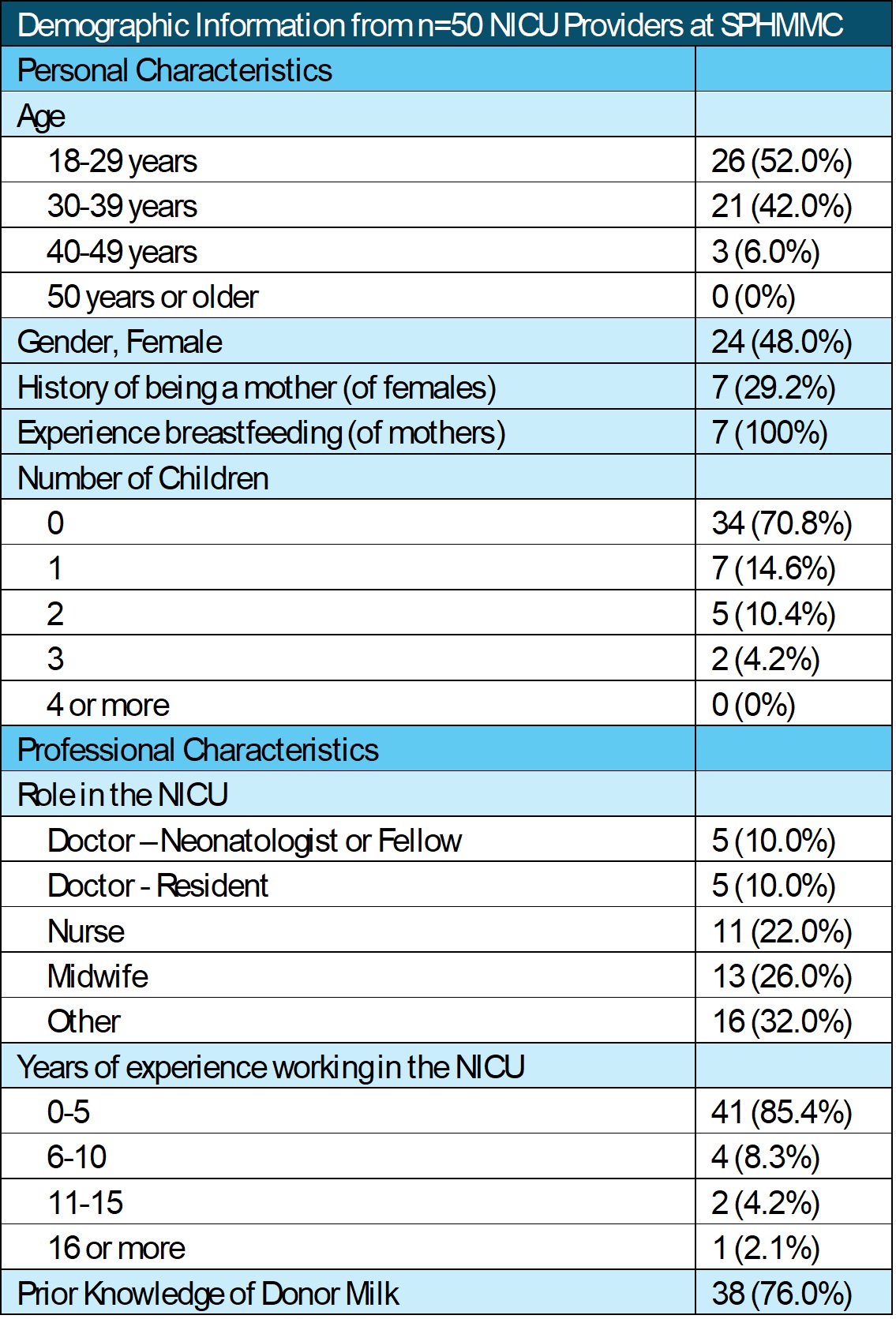
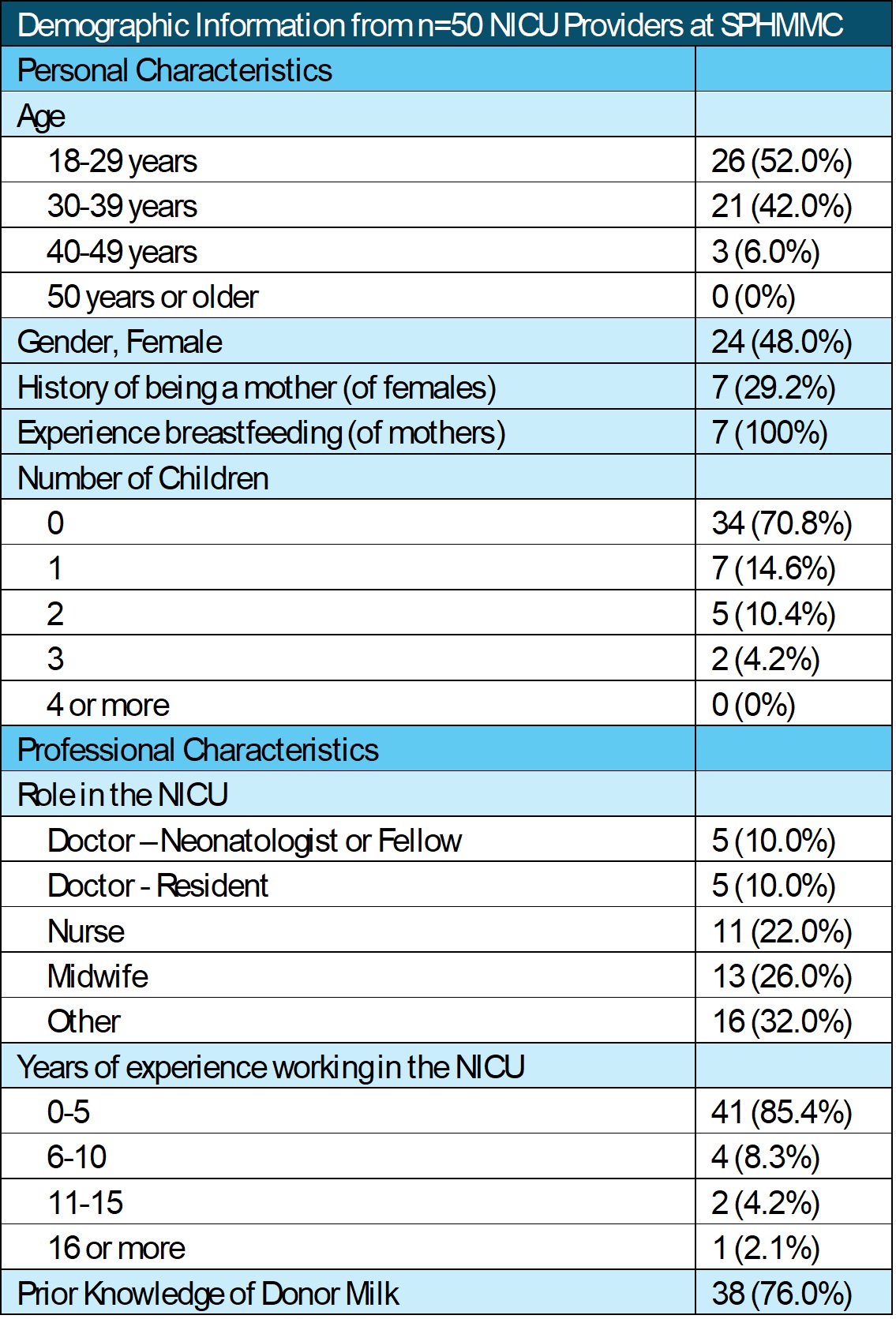
Results: Of the 50 providers who completed the survey; 76% had heard of DHM (Table 1). 78% “encounter newborns who have no access to their mother’s breast milk” primarily due to maternal illness (66.7%) or death (61.5%), yet 94% report that infants are “never fed with the breastmilk of another woman”. Around half of providers “disapprove” or “strongly disapprove” of a mother breastfeeding a baby who is not her own in the community (50%), the NICU (58%), and following maternal death (46%). Formula was the preferred alternative to MOM, with 88% of providers “willing” or “extremely willing” to offer formula (vs 44% for DHM; Figure 1a) and 86% describing formula as having “good” or “very good” nutrition (vs 76% for DHM; Figure 1b). Over 60% of providers would support offering DHM (Figure 2a, 2b) and providing mothers with deceased infants the opportunity to donate milk (Figure 2c). 72% view establishing a DHM program as “important” or “extremely important” (Figure 2d). “NICU Resources” (40%) and “Safety” (34%) were cited as the primary concerns about implementing a DHM program at SPHMMC. 58% listed “Provider Perceptions” as a barrier while 38% listed “Mothers’ Perceptions.”
Conclusion(s): A majority of providers at SPHMMC are supportive of offering DHM to NICU babies yet view formula as the preferred alternative to MOM and about half disapprove of mother’s directly breastfeeding a baby who is not her own. Providers see their own perceptions of DHM as the primary barrier to implementation. Further work is needed to target human and systems factors influencing DHM adoption in Ethiopia.
Demographic Information from n=50 NICU Providers at SPHMMC
Beliefs about neonatal nutrition as expressed by Ethiopian medical providers.
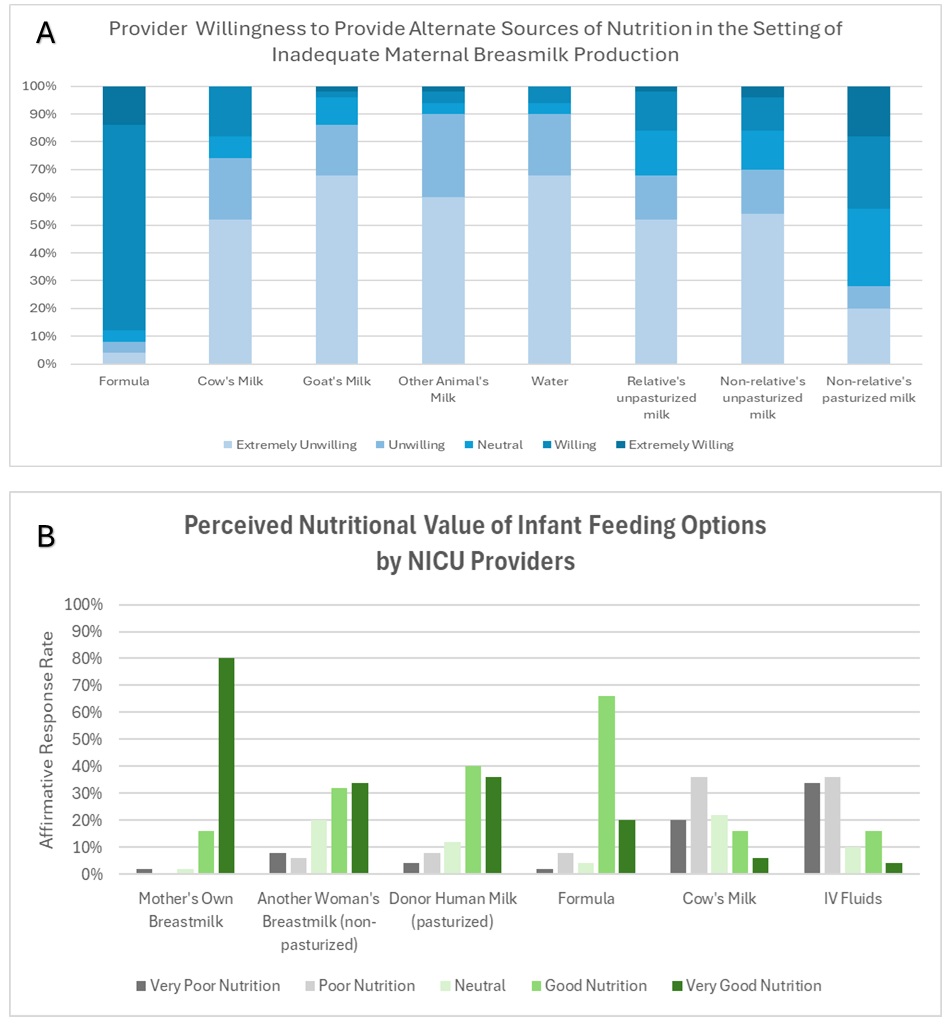 Figure 1: Beliefs about neonatal nutrition as expressed by Ethiopian medical providers. Panel (A) depicts willingness to provide proposed alternative feeds, including donor milk, when maternal milk is not available. Panel (B) depicts perceived nutritional value of proposed alternative feeds.
Figure 1: Beliefs about neonatal nutrition as expressed by Ethiopian medical providers. Panel (A) depicts willingness to provide proposed alternative feeds, including donor milk, when maternal milk is not available. Panel (B) depicts perceived nutritional value of proposed alternative feeds.Provider views on Donor Human Milk (DHM).
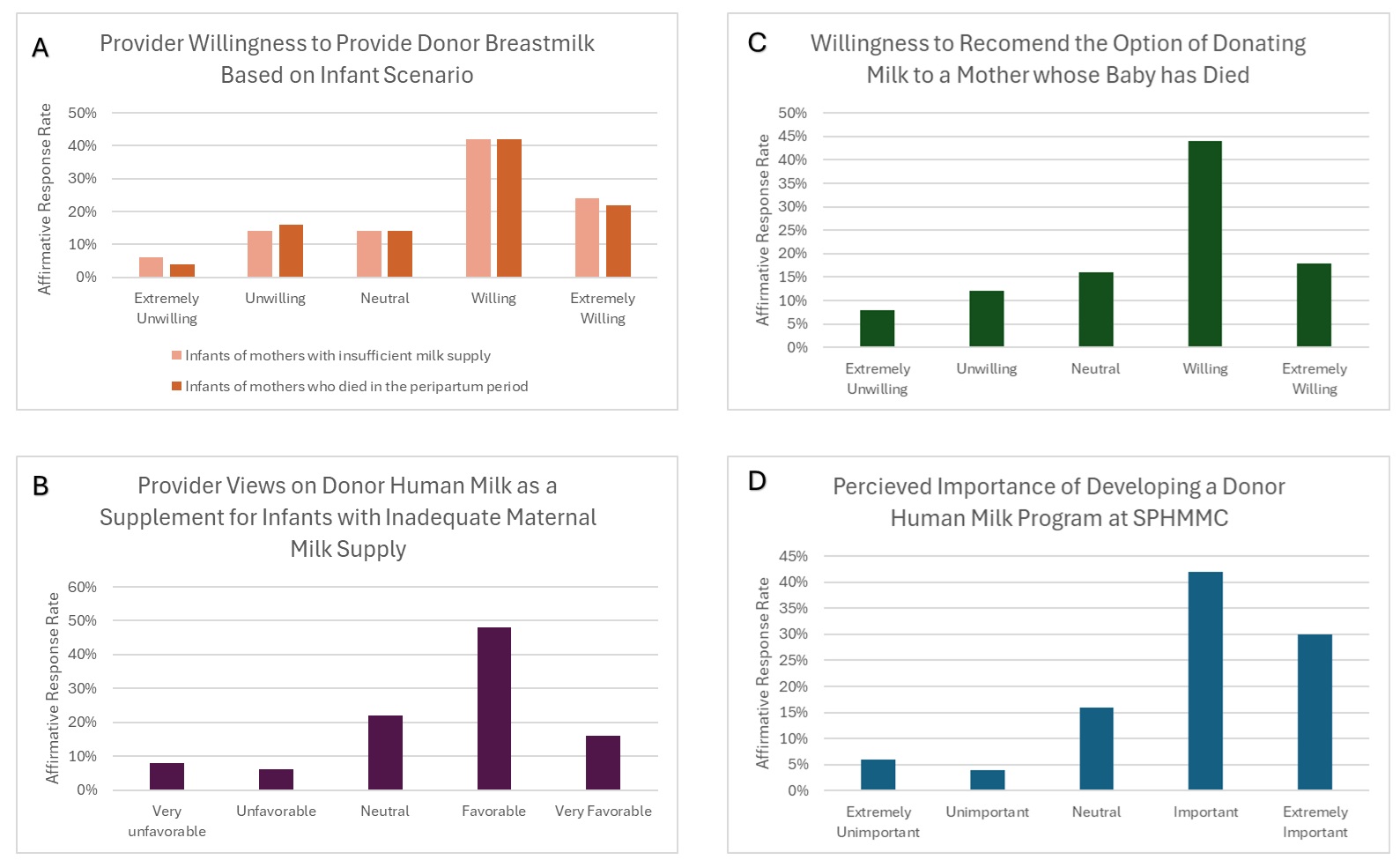 Figure 2: Provider views on Donor Human Milk (DHM). Panels depict views related to providing DHM in the setting of maternal death (A) or low maternal supply (A and B), and in recommending the option to donate milk to other babies if a woman’s own child has died (C). Panel (D) depicts overall perceived importance of developing a DHM in the NICU in Ethiopia.
Figure 2: Provider views on Donor Human Milk (DHM). Panels depict views related to providing DHM in the setting of maternal death (A) or low maternal supply (A and B), and in recommending the option to donate milk to other babies if a woman’s own child has died (C). Panel (D) depicts overall perceived importance of developing a DHM in the NICU in Ethiopia. Demographic Information from n=50 NICU Providers at SPHMMC
Beliefs about neonatal nutrition as expressed by Ethiopian medical providers.
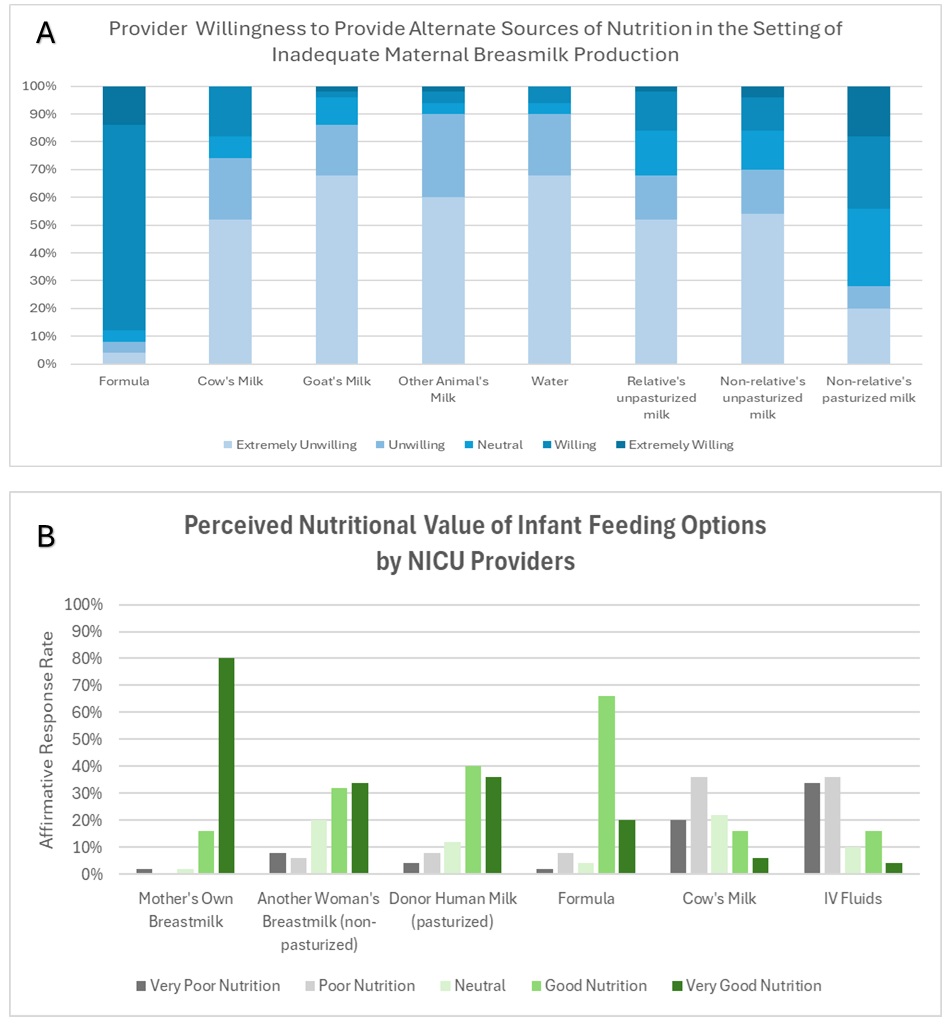 Figure 1: Beliefs about neonatal nutrition as expressed by Ethiopian medical providers. Panel (A) depicts willingness to provide proposed alternative feeds, including donor milk, when maternal milk is not available. Panel (B) depicts perceived nutritional value of proposed alternative feeds.
Figure 1: Beliefs about neonatal nutrition as expressed by Ethiopian medical providers. Panel (A) depicts willingness to provide proposed alternative feeds, including donor milk, when maternal milk is not available. Panel (B) depicts perceived nutritional value of proposed alternative feeds.Provider views on Donor Human Milk (DHM).
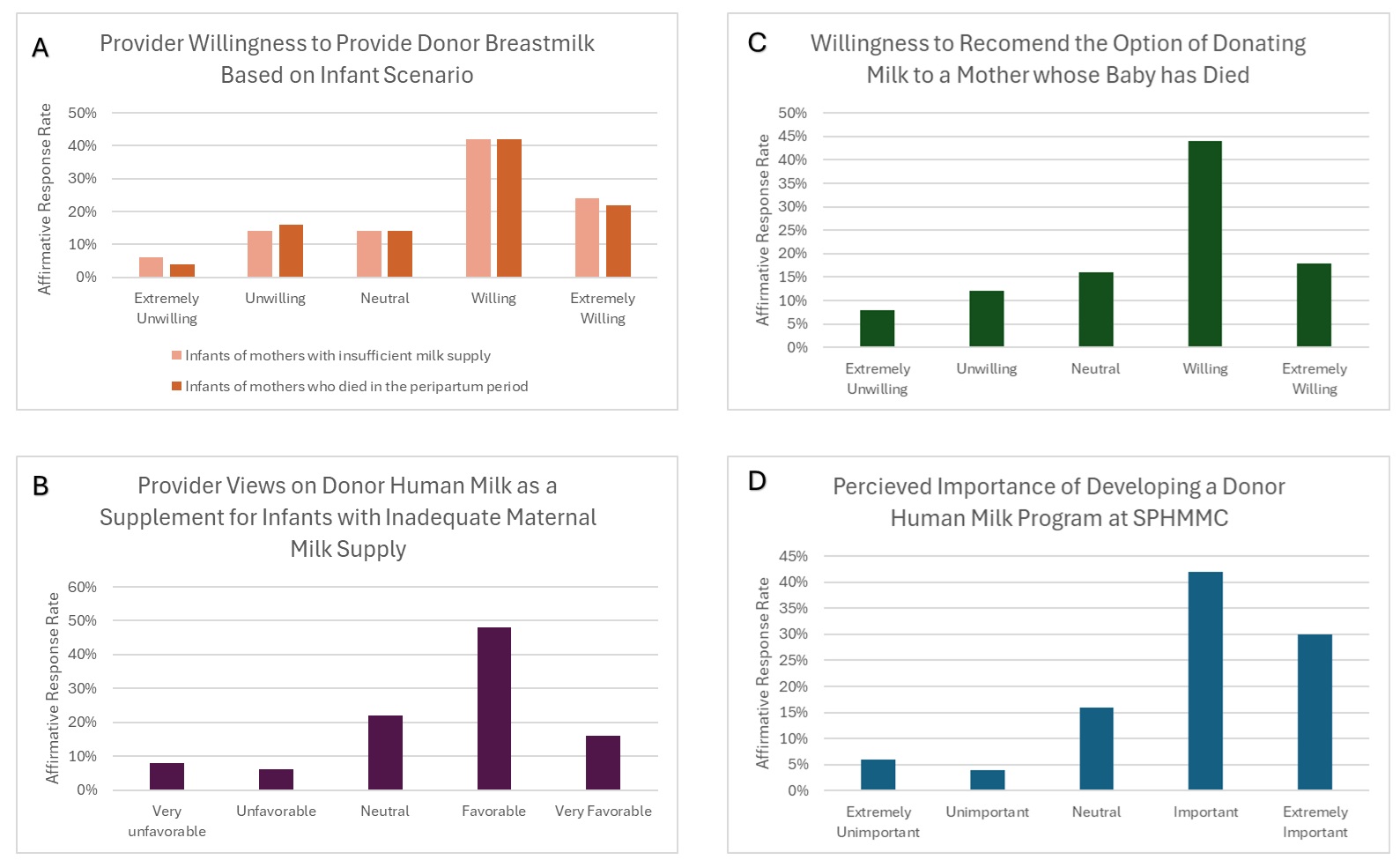 Figure 2: Provider views on Donor Human Milk (DHM). Panels depict views related to providing DHM in the setting of maternal death (A) or low maternal supply (A and B), and in recommending the option to donate milk to other babies if a woman’s own child has died (C). Panel (D) depicts overall perceived importance of developing a DHM in the NICU in Ethiopia.
Figure 2: Provider views on Donor Human Milk (DHM). Panels depict views related to providing DHM in the setting of maternal death (A) or low maternal supply (A and B), and in recommending the option to donate milk to other babies if a woman’s own child has died (C). Panel (D) depicts overall perceived importance of developing a DHM in the NICU in Ethiopia. 
