General Pediatrics 3
Session: General Pediatrics 3
218 - Family Perspectives on Inclusive Family Engagement in Pediatric Primary Care
Sunday, April 27, 2025
8:30am - 10:45am HST
Publication Number: 218.4612
Jennifer O. Lambert, Johns Hopkins University School of Medicine, Baltimore, MD, United States; Emani Kelley, Johns Hopkins University School of Medicine, Baltimore, MD, United States; Amber Elaine. Bulna, Johns hopkins children’s center, Baltimore, MD, United States; Ria Gupta, Johns Hopkins University School of Medicine, Katy, TX, United States; Nakiya Showell, Johns Hopkins University School of Medicine, Baltimore, MD, United States; Brandon M. Smith, Johns Hopkins University School of Medicine, Baltimore, MD, United States

Jennifer O. Lambert, MD, MHS (she/her/hers)
General Academic Pediatrics Fellow
Johns Hopkins University School of Medicine
Baltimore, Maryland, United States
Presenting Author(s)
Background: Patient and family engagement is an important mechanism to improve healthcare quality and achieve health equity. Family engagement has been implemented at the institutional level in many pediatric inpatient settings using the Patient and Family Advisory Council (PFAC) model. However, research shows that PFAC membership is not representative of the communities they seek to represent, and it is unclear how this model is best applied to pediatric outpatient settings. Therefore, we sought to explore the preferences of families for inclusive and equitable collective family engagement in pediatric primary care.
Objective: To elicit perspectives from family caregivers on 1) the importance of collective family engagement with their child’s pediatric primary care clinic and 2) how to implement collective family engagement in an inclusive and equitable way in the pediatric primary care setting.
Design/Methods: Four virtual, one-hour-long focus groups, three in English and one in Spanish, were conducted with adult caregivers of pediatric patients who receive care at an academic, pediatric primary care clinic. An inductive, iterative coding process was used to analyze the qualitative data using the immersion-crystallization approach to identify major and minor themes.
Results: Twenty-two caregivers participated in four focus groups (Table 1). Participants were 100% female, 73% Black or African American, and 18% Hispanic or Latino. Most participants’ households were single-adult headed (64%) and 82% reported their children had public health insurance.
As detailed in Table 2 with representative quotations, our major themes were: 1) families viewed collective engagement as an essential component of high-quality, equitable, and culturally responsive care, which had the potential to improve multiple outcomes, 2) families preferred virtual, flexible engagement opportunities as these maximized their involvement while balancing competing priorities, and 3) families identified improved communication as a priority target area for family engagement efforts.
Conclusion(s): Caregivers view collective family engagement with their child’s primary care clinic as essential and expressed preferences for engagement, which differ from the traditional PFAC model. Pediatric primary care clinics should create virtual, flexible opportunities for connection between families and clinic leadership to promote inclusive and equitable collective family engagement. Further research is needed to identify whether collective family engagement in pediatric primary care improves communication as well as child and family health outcomes.
Table 1- Participant Demographic Characteristics (n=22)
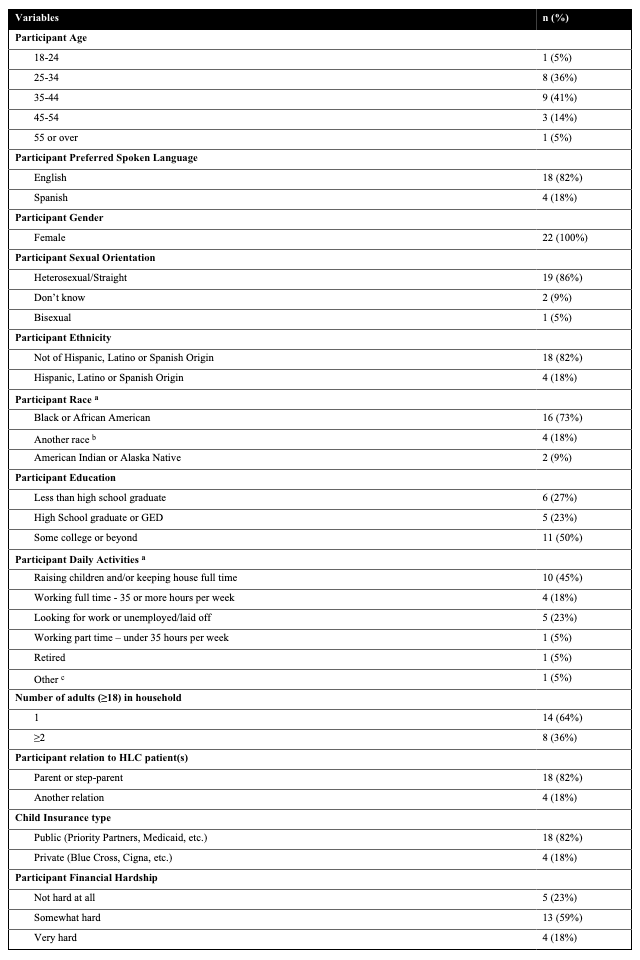 a Participants were asked to select all that apply
a Participants were asked to select all that apply b Participants specified race as: n=1 “mestiza” and n=3 did not specify
c Participant specified “Disabled, seeking disability”
Table 2- Major Themes with Representative Quotations

Table 1- Participant Demographic Characteristics (n=22)
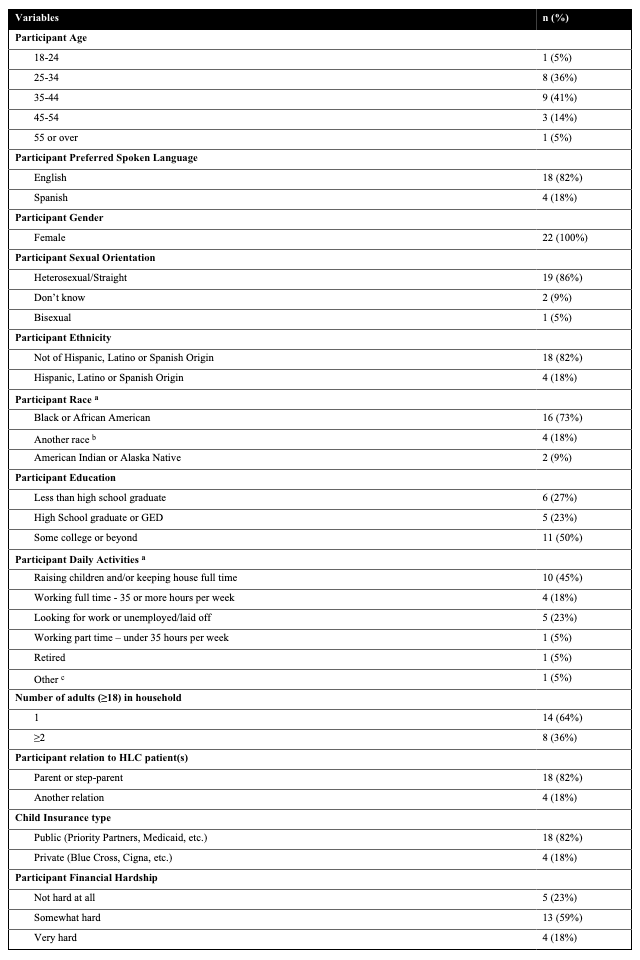 a Participants were asked to select all that apply
a Participants were asked to select all that apply b Participants specified race as: n=1 “mestiza” and n=3 did not specify
c Participant specified “Disabled, seeking disability”
Table 2- Major Themes with Representative Quotations


