Emergency Medicine 8
Session: Emergency Medicine 8
112 - Evaluation of hydration status in children with type 1 diabetes and diabetic ketoacidosis using artificial intelligence-assisted point-of-care ultrasound
Sunday, April 27, 2025
8:30am - 10:45am HST
Publication Number: 112.4617
Rachel G. Hedstrom, Children's Hospitals and Clinics of Minnesota, Saint Paul, MN, United States; Kelly R.. Bergmann, Children’s Minnesota, University of Minnesota Masonic Children’s Hospital, Minneapolis, MN, United States; Valerie Whitcomb, Children's Minnesota, Minneapolis, MN, United States; Shea Lammers, Children's Hospitals and Clinics of Minnesota, Minneapolis, MN, United States; Paige Reimche, Children's Hospitals and Clinics of Minnesota, Minneapolis, MN, United States

Rachel G. Hedstrom, MD (she/her/hers)
Pediatric Emergency Medicine Fellow
Children's Hospitals and Clinics of Minnesota
Saint Paul, Minnesota, United States
Presenting Author(s)
Background: Point-of-care ultrasound (POCUS) is a noninvasive and rapid diagnostic tool that has been used to assess intravascular hydration status in pediatric patients.
Objective: We aimed to use an artificial intelligence (AI) feature embedded within our POCUS machine to assess hydration status as measured by inferior vena cava (IVC) collapsibility in children and adolescents with diabetes and diabetic ketoacidosis (DKA).
Design/Methods: We conducted a prospective, observational, cohort study including pediatric patients with diabetes who presented to the emergency department between March 2023 and May 2024. The patients were categorized into 3 groups: non-DKA, mild DKA, and moderate/severe DKA. IVC collapsibility was measured using POCUS (Figure 1), and was correlated with clinical assessments of dehydration, the Gorelick dehydration scale, percent body weight loss, and laboratory values.
Results: We included 87 encounters, with a median age of 11 (IQR 7-14). Fifty-four (62.1%) patients were categorized as non-DKA, 22 (25.3%) as mild, 11 (12.6%) and as moderate/severe (Table 1). Though IVC collapsibility was not found to be statistically significant across DKA severity groups (p=0.16), % body weight loss (p < 0.01), the 10-point Gorelick dehydration scale (p=0.01), the 4-point Gorelick dehydration scale (p=0.07), and the clinical estimation of dehydration made by clinician (p=0.02) were found to be significantly different among the groups (Table 2). Nonparametric correlations revealed no statistically significant correlation between AI-assisted IVC collapsibility and percent weight loss (p=0.24), or between AI-assisted IVC collapsibility and clinician estimate of dehydration (p=0.74), the Gorelick dehydration scale (p=0.62), or any laboratory values. Clinician estimate of dehydration significantly predicted percent body weight loss, where the more severe the estimate of dehydration, the higher the percentage of weight loss (1.80% body weight loss, 95% CI 0.46% - 3.13%). The Gorelick dehydration scale also significantly (p < 0.01) predicted body weight loss, where for every 1-point increase in the score, there was approximately 1.21% change in body weight loss (95% CI 0.47% - 1.96%).
Conclusion(s): The role of POCUS in assessing hydration status in children with DKA was not a reliable measure of intravascular volume status in our study. Further study is needed to validate our findings.
Figure 1.
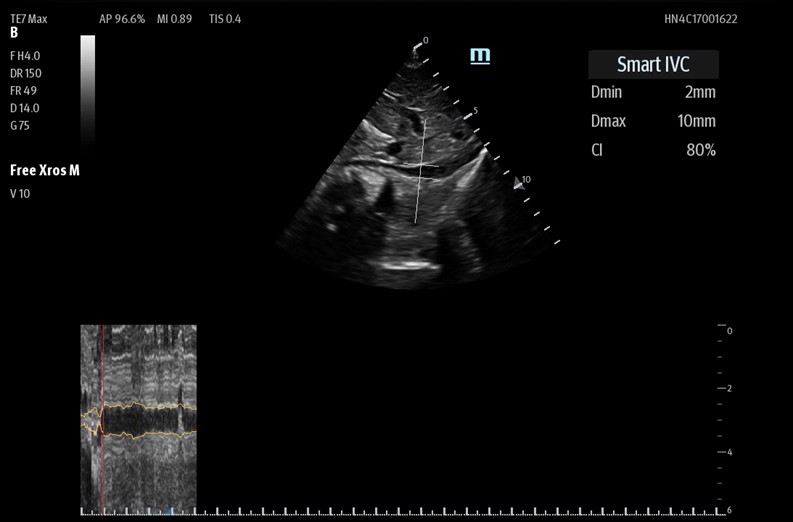 Utilizing the "Smart IVC" mode on the Mindray TE7 Max ultrasound machine.
Utilizing the "Smart IVC" mode on the Mindray TE7 Max ultrasound machine.Table 1.
.jpg) Demographic and encounter-level characteristics.
Demographic and encounter-level characteristics.Table 2.
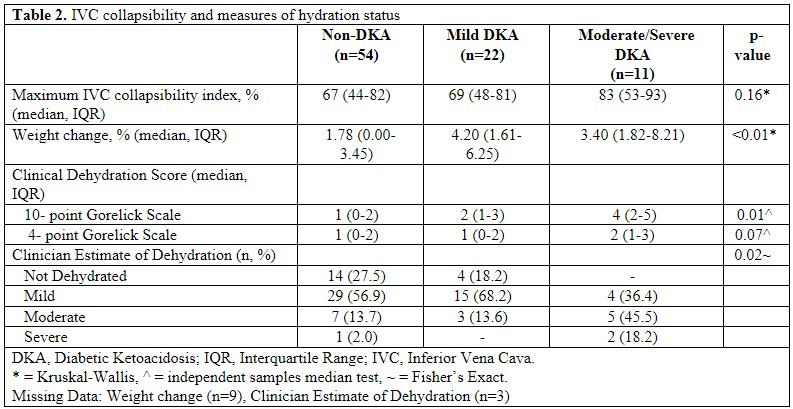 IVC Collapsibility and measures of hydration status.
IVC Collapsibility and measures of hydration status.Figure 1.
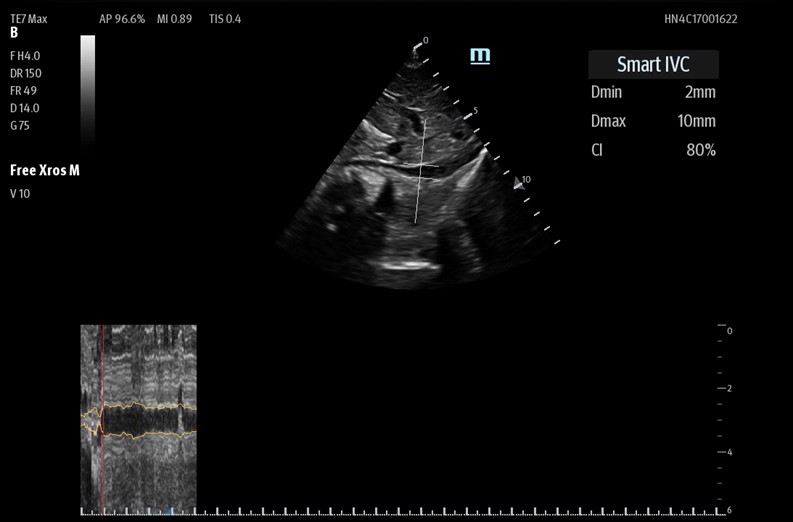 Utilizing the "Smart IVC" mode on the Mindray TE7 Max ultrasound machine.
Utilizing the "Smart IVC" mode on the Mindray TE7 Max ultrasound machine.Table 1.
.jpg) Demographic and encounter-level characteristics.
Demographic and encounter-level characteristics.Table 2.
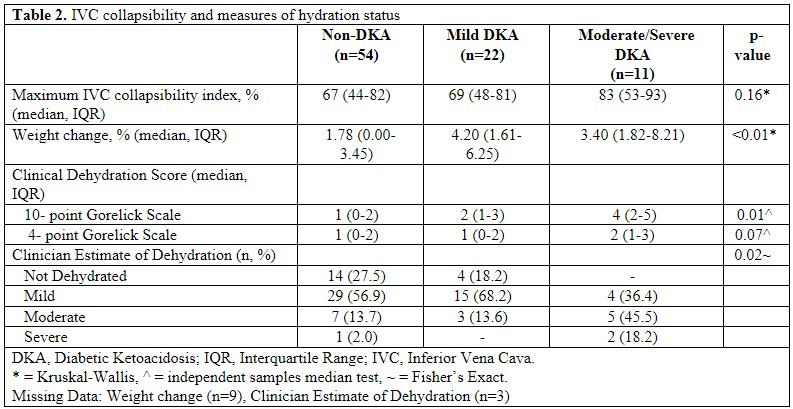 IVC Collapsibility and measures of hydration status.
IVC Collapsibility and measures of hydration status.
