Obesity 1
Session: Obesity 1
274 - Feasibility of Using Best Practice Alerts in Pediatric Primary Care for Equitable Recruitment in Obesity Research
Sunday, April 27, 2025
8:30am - 10:45am HST
Publication Number: 274.4619
Annika Blackbird. Kruse, Duke University School of Medicine, Durham, NC, United States; Sarah Armstrong, Professor of Pediatrics, Chapel Hill, NC, United States; Asheley C. Skinner, Duke University, Durham, NC, United States; Cody D. Neshteruk, Duke University School of Medicine, Durham, NC, United States

Annika Blackbird Kruse, BS (she/her/hers)
Medical Student
Duke University School of Medicine
Durham, North Carolina, United States
Presenting Author(s)
Background: Childhood obesity affects over 14 million youth in the U.S., with the highest prevalence among Black, Hispanic, and low-income populations. These priority groups face unique challenges in accessing lifestyle interventions, which have proven effective in non-Hispanic White children but less so in these underserved populations. A significant barrier to addressing this disparity in pediatric obesity research is recruitment, especially among diverse populations. Stigma, parental attitudes, and psychosocial barriers can deter participation. The use of electronic health record (EHR) Best Practice Alerts (BPAs) has emerged as a tool for improving recruitment efficiency, but its role in pediatric obesity research remains underexplored.
Objective: This study aimed to assess the feasibility and effectiveness of using an EHR BPA to recruit pediatric patients with obesity into a clinical research trial for lifestyle interventions, with a specific focus on increasing recruitment from diverse populations.
Design/Methods: A BPA was implemented in the Duke Health EHR system (Epic) for the Hearts & Parks randomized controlled trial. The alert triggered during well-child visits for patients aged 5-17 years with a body mass index (BMI) ≥95th percentile. Primary care providers (PCPs) received a notification to gauge caregiver interest in research participation. They could either indicate interest, decline, or opt out if clinical concerns existed. Study coordinators followed up with those who expressed interest to confirm eligibility and complete recruitment. Outcomes from BPA recruitment were compared to traditional methods like direct caregiver contact and in-person recruitment.
Results: From January 2018 to April 2020, the BPA was triggered for 2,121 patients. PCPs responded 85% of the time, leading to 1,422 follow-ups. Of these, 1,104 caregivers (78%) expressed interest, and 177 children were enrolled, comprising 68% of total study participants. Other recruitment methods contributed 32% of the sample. Notably, 83.5% of participants recruited through the BPA were from minoritized racial and ethnic groups. The number needed to screen to enroll one participant via the BPA was 12.
Conclusion(s): EHR BPAs are a feasible and effective recruitment tool for pediatric obesity research, significantly increasing diversity and efficiency. BPAs streamline the recruitment process, reducing cost and time burdens on staff while engaging underrepresented populations. Future work should explore optimizing BPA design to minimize alert fatigue and balance automation with provider discretion.
Figure 1: Best Practice Alert within the Electronic Health Record
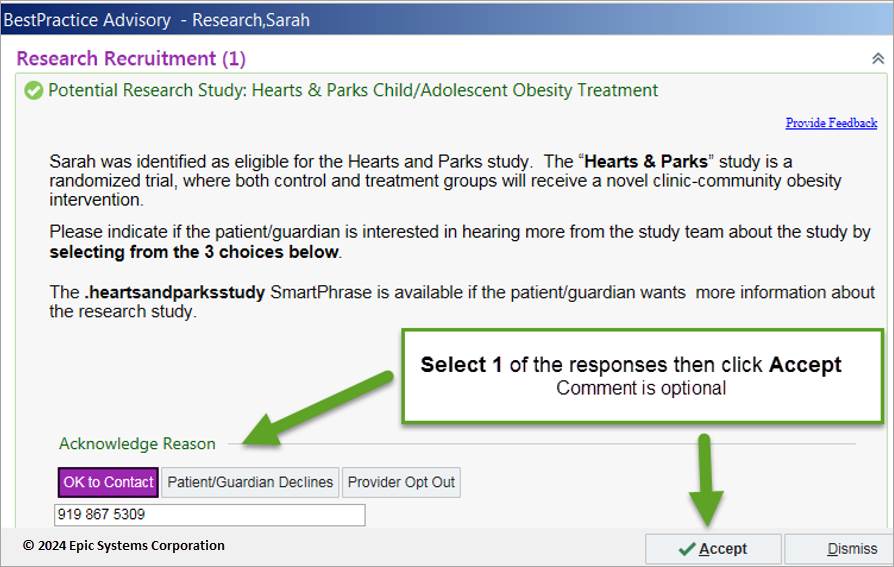 A screenshot of the best practice alert within the electronic health system as seen by pediatric primary care providers
A screenshot of the best practice alert within the electronic health system as seen by pediatric primary care providersFigure 2: Best Practice Alert Workflow and Responses
Figure4.pdfA workflow process describing the best practice alert deployment within the electronic health record in the pediatric primary care setting with primary care providers
Figure 1: Best Practice Alert within the Electronic Health Record
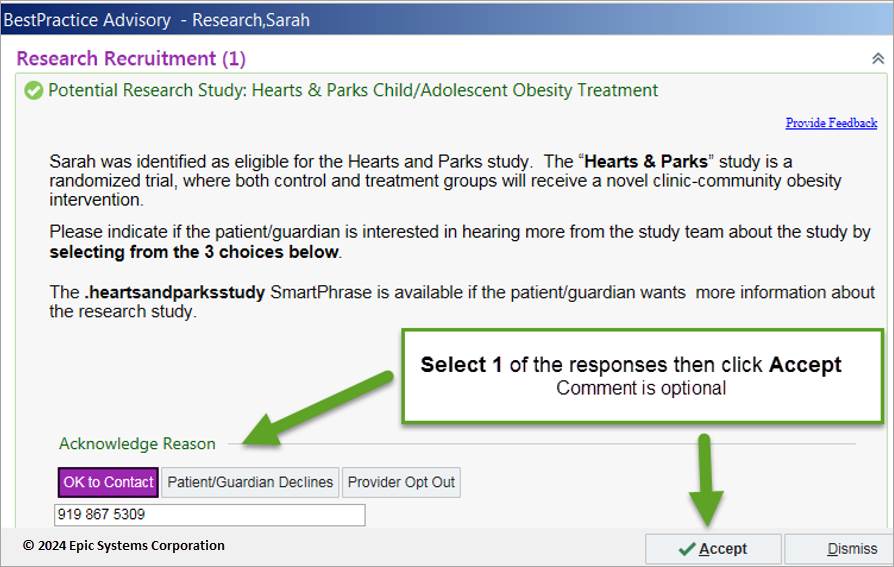 A screenshot of the best practice alert within the electronic health system as seen by pediatric primary care providers
A screenshot of the best practice alert within the electronic health system as seen by pediatric primary care providersFigure 2: Best Practice Alert Workflow and Responses
Figure4.pdfA workflow process describing the best practice alert deployment within the electronic health record in the pediatric primary care setting with primary care providers

