Hospital Medicine 3: Systems/Population-based Research
Session: Hospital Medicine 3: Systems/Population-based Research
140 - Drivers of Inpatient Antibiotic Prescribing Diversity Among Pediatric Hospitalists: A Qualitative Study
Sunday, April 27, 2025
8:30am - 10:45am HST
Publication Number: 140.4861
Jessica Markham, Children's Mercy Kansas City, Kansas City, MO, United States; Sarah Fouquet, University of Missouri-Kansas City School of Medicine, Lenexa, KS, United States; Eryn Godwin, Children's Mercy Hospitals and Clinics, Kansas City, MO, United States; Alaina Burns, Children's Mercy Hospitals and Clinics, Kansas City, MO, United States; Jennifer Goldman, Children's Mercy Hospitals and Clinics, Kansas City, MO, United States; Kathy Goggin, San Diego State University, San Diego, CA, United States

Jessica Markham, MD, MSc (she/her/hers)
Dr.
Children's Mercy Kansas City
Kansas City, Missouri, United States
Presenting Author(s)
Background: Despite nationally endorsed treatment guidelines and antimicrobial stewardship programs, 30-50% of all antibiotics are still inappropriately prescribed or completely unnecessary. While hospital-level antibiotic prescribing diversity has been described quantitatively, qualitative methods may help elucidate novel factors influencing prescribing diversity.
Objective: To describe factors influencing antibiotic prescribing diversity using qualitative methods.
Design/Methods: We performed a qualitative study within a sequential mixed-methods design to elucidate key drivers of antibiotic prescribing diversity. We conducted semi-structured interviews with a purposive sample of pediatric hospitalists from 3 children’s hospitals previously identified as having low antibiotic diversity indices (i.e. high hospital-level similarity in empiric antibiotic prescribing for common infections). Interviews were conducted virtually, audio-recorded, transcribed verbatim, de-identified, and proofread for accuracy. Guided by the Social Ecological Model, we conducted a content analysis to synthesize information using both deductive and inductive codes. Reflexivity and member checking were utilized during analysis to ensure rigor.
Results: We recruited 10 pediatric hospitalists across the 3 hospitals (Table 1). Hospitalists overwhelmingly self-identified as being frontline stewards and teachers of antibiotic stewardship, but existing outside of formal antibiotic stewardship programs. Hospitalists identified collegial antibiotic stewardship relationships (i.e. handshake stewardship), cultures of change and evidence-based practice, cohesiveness of the hospitalist group (i.e. mutual trust and collaboration), and ability to generate shared mental models (e.g. clinical pathways, order sets) as influencing antibiotic prescribing similarity. Hospitalists also described factors in their work environment (e.g. resource availability at the point-of-care, integration of prescribing resources into clinical workflows, intuitiveness/complexity of order processes) that challenge prescribing similarity. Drivers of antibiotic prescribing diversity supported by representative quotations are presented in Table 2.
Conclusion(s): Antibiotic prescribing is complex and influenced by many interpersonal, organizational, and systems-based factors beyond a patient’s clinical status. Hospitalist relationships with other key stakeholders play a strong role in antibiotic decisions. Creating a 'shared mission' of stewardship through formal engagement of hospitalists on stewardship committees may enhance implementation of prescribing interventions.
Table 1. Characteristics of participating hospitalists.
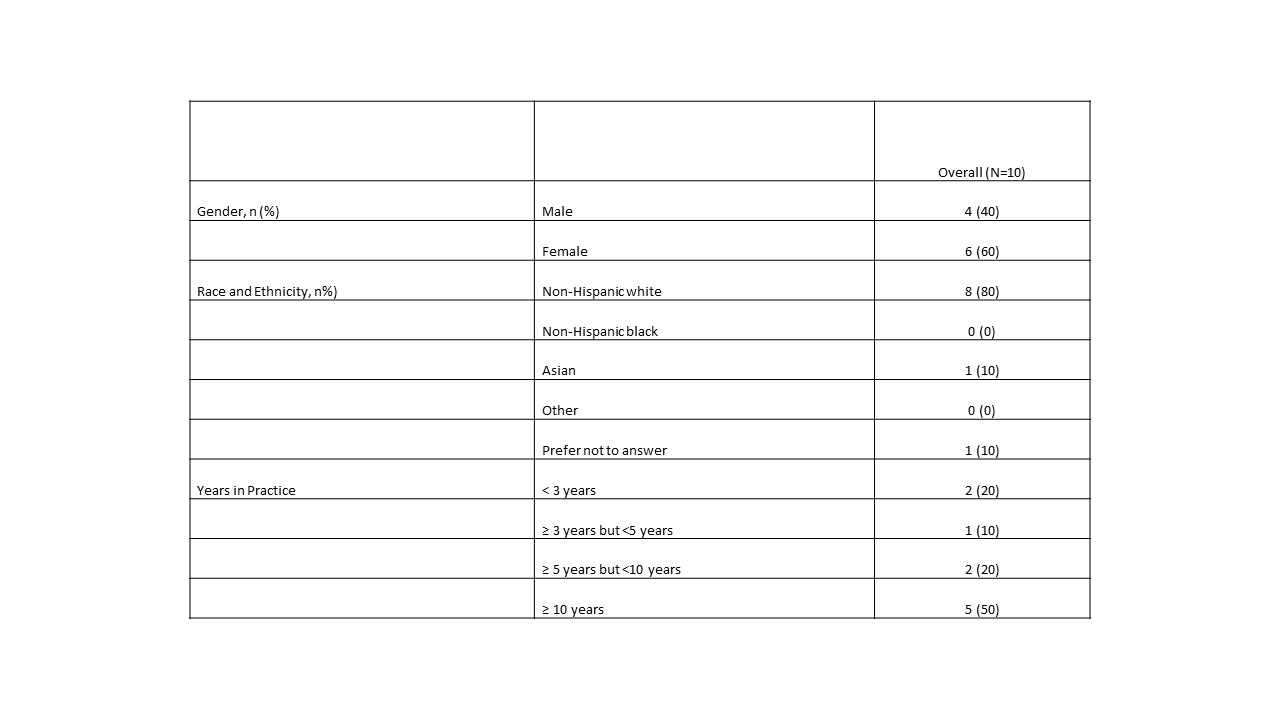
Table 2. Drivers of antibiotic prescribing diversity supported by representative quotations organized using the social ecological model.
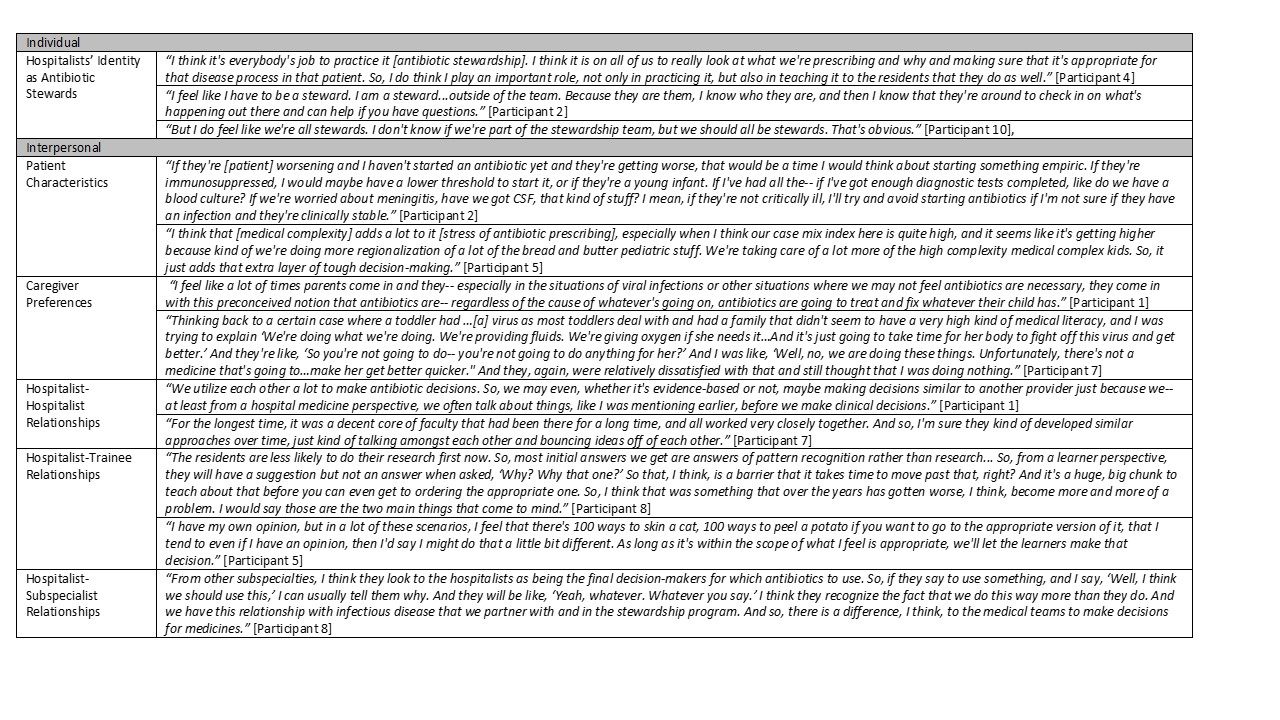
Table 2 (Continued) Drivers of antibiotic prescribing diversity supported by representative quotations organized using the social ecological model.
.jpg)

