Child Abuse & Neglect 2
Session: Child Abuse & Neglect 2
359 - In Search of the Unknown Mimic of Abusive Head Trauma
Sunday, April 27, 2025
8:30am - 10:45am HST
Publication Number: 359.5231
Ruairi E. Smith-Dewey, Children's Mercy Hospital, KANSAS CITY, MO, United States; Angela Bachim, Baylor College of Medicine, Houston, TX, United States; Colleen J. Bressler, Medical University of South Carolina College of Medicine, Charleston, SC, United States; Kristine A. Campbell, University of Utah School of Medicine, Salt Lake City, UT, United States; Lori Frasier, Penn state hershey, Hershey, PA, United States; Danielle Horton, Children's Mercy Hospital, Kansas City, MO, United States; Nicole R. Johnson, University of Minnesota Masonic Children's Hospital, Minneapolis, MN, United States; Jan Leonard, Children's Hospital of Philadelphia, Philadelphia, PA, United States; Megan M.. Letson, Nationwide Children's Hospital, Columbus, OH, United States; Caitlin R. McNamara, UPMC Childrens Hospital of Pittsburgh, Pittsburgh, PA, United States; Shalon M. Nienow, UC San Diego School of Medicine, San Diego, CA, United States; Stuart W. Sommers, Boston University School of Medicine, Boston, MA, United States; Joanne N. Wood, Children's Hospital of Philadelphia, Philadelphia, PA, United States; Jim Anderst, Children's Mercy Hospitals and Clinics, Kansas City, MO, United States
.jpg)
Ruairi E. Smith-Dewey, DO (she/her/hers)
Child Abuse Pediatric Fellow
Children's Mercy Hospital
KANSAS CITY, Missouri, United States
Presenting Author(s)
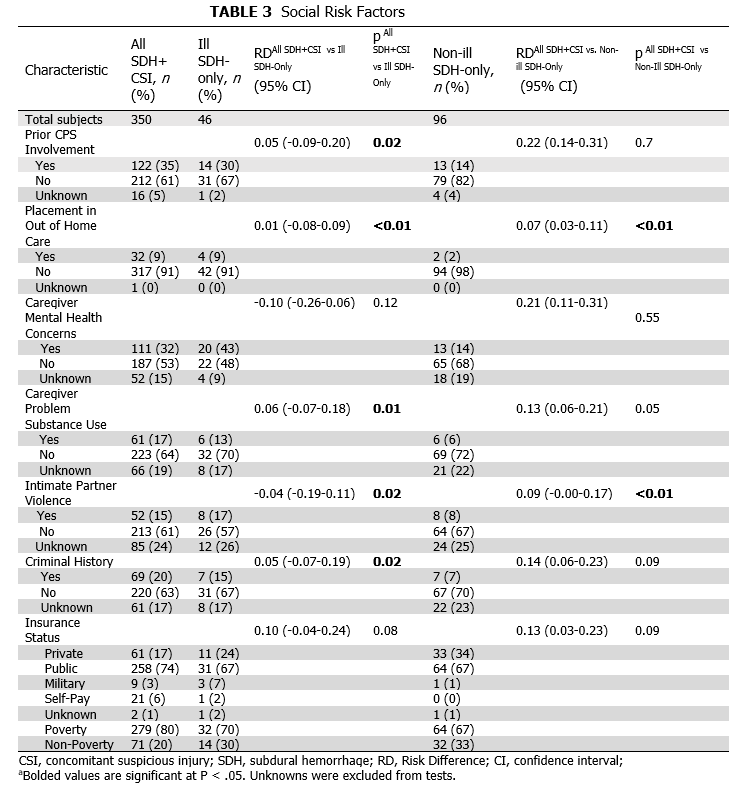
Background: Child Abuse Pediatricians (CAPs) are accused of misdiagnosing a yet-to-be-identified mimic as abusive head trauma (AHT), particularly in ill children with an isolated subdural hemorrhage (SDH). Though not diagnostic criteria, specific social stressors are identified as AHT risk factors. The existence of a mimic can be assessed by comparing the prevalence of AHT risk factors across study groups (See Table 1).
Objective: We hypothesize that the distribution of AHT risk factors will be: fewer in the CAP-identified mimic group versus the CAP-diagnosed abuse group, no difference between ill SDH only and SDH+CSI groups as these are likely the same condition, and fewer in the non-ill SDH only versus SDH+CSI groups as there are likely undocumented known mimics in the non-ill SDH only group.
Design/Methods: Retrospective case-control study using Child Abuse Pediatrics Research Network (CAPNET) data from 10 sites over 27 months. As proof of concept, the prevalence of AHT risk factors was compared between CAP-identified mimics and CAP-diagnosed abuse groups. Social risks were compared using unadjusted odds ratios with 95% confidence intervals. For social risk comparison across SDH groups, subjects were < 24 months old and evaluated by a CAP. Ill subjects had cardio-respiratory collapse and/or significantly altered consciousness. CSIs were injuries that are highly associated with abuse in the skin, bones, eyes, and abdomen. CAP diagnosis was not considered for SDH group determination. Prevalence of social risk, demographics, and trauma history were compared between groups using two one-sided equivalence tests with a 20% equivalence margin.
Results: In proof of concept, 1058 subjects with known medical mimics had statistically significantly fewer AHT social risk factors than 548 abused subjects with ICH/fracture in 5/7 domains. In the main study, when comparing the 350 SDH+CSI subjects and 46 Ill SDH subjects, the two groups were statistically equivalent in 5/7 social risks. When comparing the 350 SDH+CSI and 96 Non-Ill SDH subjects, they were statistically equivalent in 2/7 social risks. Provision of trauma history was equivalent across all three groups (RD –0.01-0.10).
Conclusion(s): Social risk distribution differentiates CAPNET subjects with medical mimics from those without. Social risk distribution largely did not differ between SDH+CSI and Ill-SDH groups, indicating that a yet-to-be-identified mimic is not widely prevalent in the Ill-SDH group. Non-ill appearing subjects with SDH appear to have fewer AHT risks compared to SDH+CSI, supporting possible medical causes in some of these children.
Study Definitions
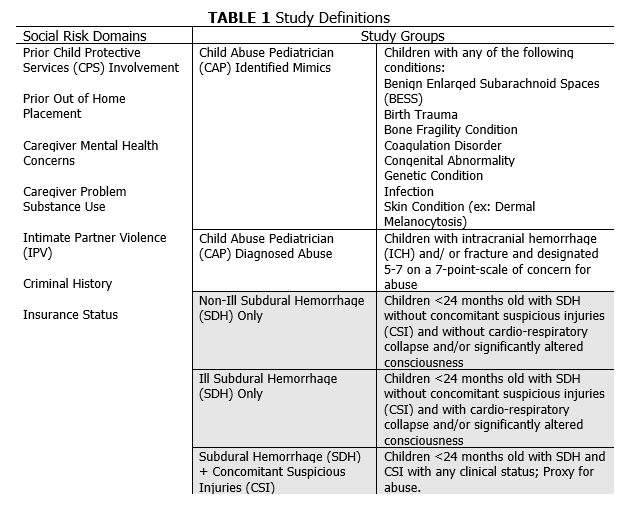
Proof of Concept
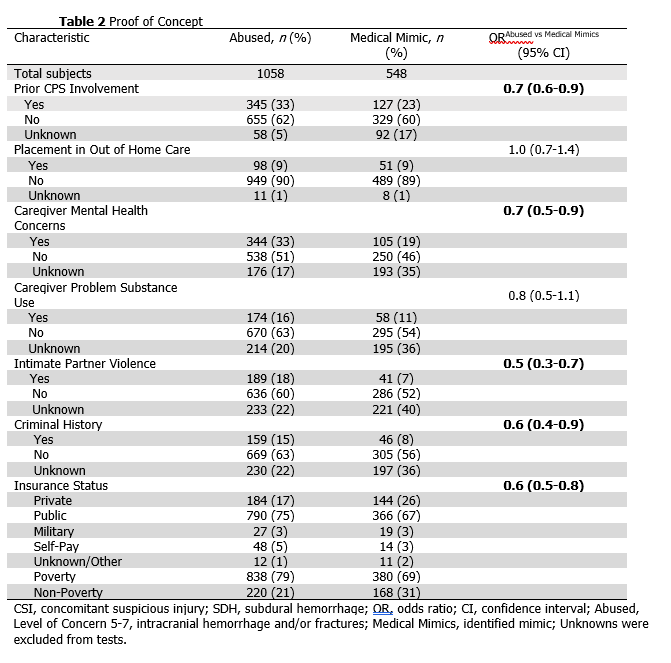
Social Risk Factors