Hospital Medicine 6: Clinical
Session: Hospital Medicine 6: Clinical
545 - In-Hospital Weight Gain Goals and Association with Readmission for Infants Admitted for Malnutrition
Sunday, April 27, 2025
8:30am - 10:45am HST
Publication Number: 545.5312
Emily B. Manion, Phoenix Children's, Phoenix, AZ, United States; Joshua B. Ritzema, Phoenix Children's Hospital, Phoenix, AZ, United States; Minu S. Bhanvadia, Phoenix Children's Hospital, Phoenix, AZ, United States; Sandra Gage, Phoenix Children's Hospital, Racine, WI, United States; Brittany Wold, Phoenix Children’s Hospital, Phoenix, AZ, United States

Emily B. Manion, MD (she/her/hers)
Hospital Medicine Fellow
Phoenix Children's
Phoenix, Arizona, United States
Presenting Author(s)
Background: Annual hospital costs for infants admitted for malnutrition (or failure to thrive) exceed $6.8 million, yet comprehensive guidelines on weight gain before discharge are lacking. Two recent studies found that 81-85% of these patients had adequate in-hospital weight gain, but evidence on outcomes is unclear. Prior studies assessed adequate weight gain using the slope of World Health Organization (WHO) growth charts to calculate expected daily weight gain; however, this method does not account for catch-up growth often needed and incorporated in nutritionist recommendations. Establishing in-hospital weight gain targets is important for outpatient success and reduction in readmissions.
Objective: Compare the association of readmission for infants admitted for malnutrition meeting WHO weight velocity standards versus nutritionist goals for daily weight gain.
Design/Methods: This IRB-approved retrospective cohort study examined infants 1-12 months old admitted to hospital medicine for malnutrition at a tertiary children’s hospital from 1/2018 to 12/2022. Exclusion criteria: < 36 weeks’ gestation, acute illness. In-hospital daily weight gain calculated as the difference between admission and discharge weight divided by the number of days between measurements. Infants were categorized as meeting or not meeting expected daily weight gain (1) based on WHO weight velocity standards (50th percentile for age and sex) and (2) based on the documented nutritionist goal. Descriptive statistics were used for categorical variables. Associations between goal categories and malnutrition-specific readmissions within 2 years were analyzed using χ2 tests, with P values < 0.05 considered statistically significant.
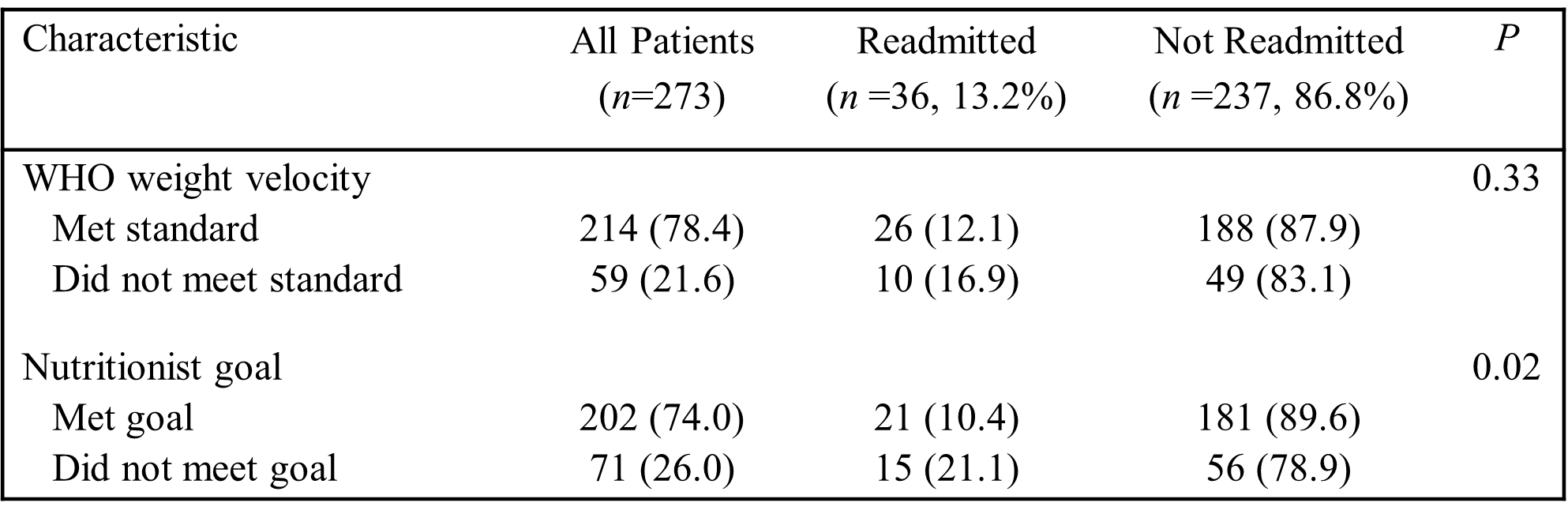
Results: Of the 273 infants included, 78.4% met expected daily weight gain based on WHO standards and 74% met the nutritionist goal, which was higher than the WHO standard in two-thirds of cases. There was no association with readmission for infants meeting the WHO standard, however those meeting the nutritionist goal were less likely to be readmitted (P=0.02) (Table).
Conclusion(s): Most infants hospitalized for malnutrition met daily weight gain targets based on both WHO standards and nutritionist goals. Meeting the nutritionist goal was associated with lower likelihood of readmission, while meeting the WHO standard showed no effect on readmission. WHO growth charts, used in prior studies to estimate adequate weight gain, may be insufficient for assessing appropriate growth in malnourished infants, and goals incorporating catch-up growth may better support post-discharge success.
Table: Infants Admitted for Malnutrition Meeting or Not Meeting Standard/Goal for Expected Daily Weight Gain