Child Abuse & Neglect 2
Session: Child Abuse & Neglect 2
357 - Improper Utilization of Head Ultrasounds Among Infants and Opportunities For Improvement
Sunday, April 27, 2025
8:30am - 10:45am HST
Publication Number: 357.5282
Bianca L. Rochelle, University of Arkansas for Medical Sciences College of Medicine, Maumelle, AR, United States; Liza Murray, University of Arkansas for Medical Sciences College of Medicine, Little Rock, AR, United States

Bianca L. Rochelle, MBS, BA (she/her/hers)
Medical Student
University of Arkansas for Medical Sciences College of Medicine
Maumelle, Arkansas, United States
Presenting Author(s)
Background: Head ultrasounds (HUS) are often utilized to evaluate infants but are not an appropriate study to evaluate for nonspecific symptoms associated with abusive head trauma. The Pittsburgh Infant Brain Injury Score (PIBIS) is a validated screening tool utilizing infant age, head circumference, skin exam, and hemoglobin level to determine when a head CT is recommended for infants < 12 months with nonspecific complaints.
Objective: Our primary aim was to explore HUS utilization for infants at our institution and quantify the rates of false positive or negative HUS studies. We also sought to identify infants inaccurately screened with a HUS when they met criteria for a head CT as measured by PIBIS.
Design/Methods: This is a single institution, retrospective review of infants < 12 months with a HUS completed outside of the NICU. An EMR-generated list of patients with HUS ordered between 1/1/23 and 4/30/24 was reviewed for inclusion. Cases were excluded if a HUS was ordered for intraventricular hemorrhage, infants on ECMO, known brain injury, or known neurological pathology. We recorded demographics, clinical presentation, PIBIS criteria, and whether the HUS demonstrated a falsely negative, positive or consistent screen as compared to head CT/MRI if obtained. PIBIS screening criteria included: >3 months, head circumference >85%, and hemoglobin < 11.2 (each 1 point) and bruising (2 points). A combined score of 2 or more is defined as a “positive” screen for a recommended head CT. Statistical analysis included descriptive statistics and chi square tests.
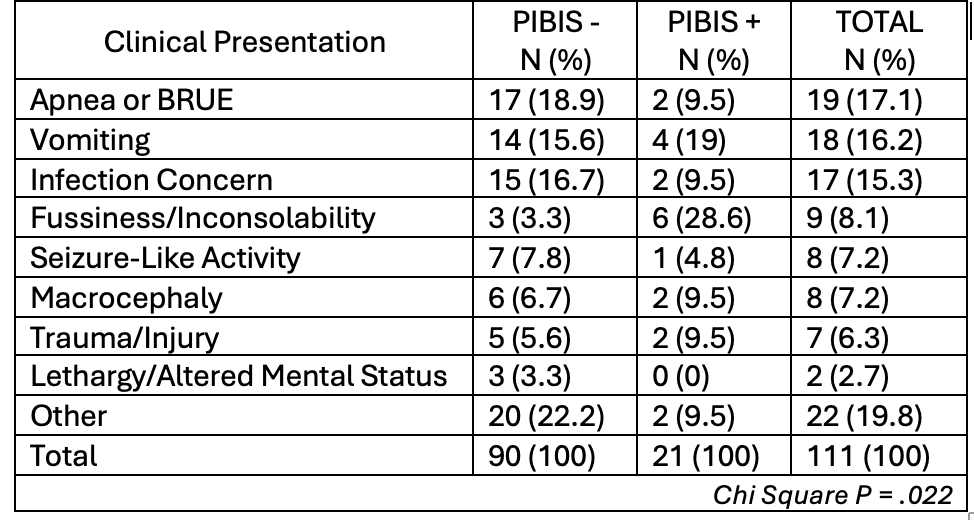
Results: We identified 111 infants with a HUS, with 63 completed in the ER and 46 in the inpatient setting. The majority were performed for infants < 3 months (74.8%) and the most common presentations were apnea/BRUE (17.1%) and vomiting (16.2%). There were 9 patients who had a head CT or MRI completed with 3 consistent results (33.3%), 3 false negatives (33.3%) and 3 false positives (33.3%). There were 21 (18.9%) cases of a positive PIBIS screen (Table 1). Of those screening positive, 6 (28.6%) presented with fussiness and 4 (19%) with vomiting. The relationship between presentation and a positive PIBIS screen was significant (p=.022).
Conclusion(s): While head ultrasounds are routinely utilized for evaluation of infants, this testing modality is not recommended for nonspecific complaints given both false positive and negative results. With nearly 20% of infants with a HUS meeting criterion for a head CT by PIBIS screening, we have also identified an opportunity for improved evaluation of infants at risk for AHT.
Clinical Presentation and Relationship to PIBIS Screen