Emergency Medicine 8
Session: Emergency Medicine 8
110 - Drivers of Bronchodilator Use in Bronchiolitis: Analyzing Treatment Trends from Pediatric Emergency Department Practices
Sunday, April 27, 2025
8:30am - 10:45am HST
Publication Number: 110.4656
Andrea Rivera-Sepulveda, Nemours Children's Health, ORLANDO, FL, United States; Timothy Maul, Nemours Children's Hospital, Orlando, FL, United States; Anna Jurlina, University of Central Florida College of Medicine, Orlando, FL, United States; Todd F.. Glass, University of Central Florida College of Medicine, Orlando, FL, United States; Kathryn Blake, Nemours Children's Health, Jacksonville, FL, United States; Matthew M. Davis, Nemours Children's Hospital, Wilmington, DE, United States; Kenneth A. Alexander, The University of Central Florida, Orlando, FL, United States

Andrea Rivera-Sepulveda, MD, MSc
Associate Professor
Nemours Children's Health
ORLANDO, Florida, United States
Presenting Author(s)
Background: Current guidelines recommend supportive care for bronchiolitis management, but bronchodilator (BD) use in the ED remains common practice without evidence of improved patient outcomes or evidence for subgroups of patients who may benefit. The basis for BD use in bronchiolitis is a demonstration of subsequent development of wheezing and asthma later in life. Studies suggest the existence of a BD-responsive bronchiolitis phenotype based on specific clinical features, such as older age, wheezing, eczema/atopic dermatitis (AD), and a history of asthma in a first-degree relative. However, no studies suggest BD response in children with bronchiolitis based on this patient profile.
Objective: This study aims to evaluate patient characteristics associated with BD use at various stages of bronchiolitis illness and examine whether BD use is associated with patient outcomes in the ED.
Design/Methods: This retrospective, cross-sectional study involves secondary data analysis from a sample of 932 children ages 3 to 24 months who received a diagnosis of bronchiolitis during an ED visit (1,057 cases). Predictor variables included demographics, past medical history, family history, physical findings, medication use, and disposition. Outcomes included (1) prior use of a BD before the current illness, (2) BD use during the current illness before the ED, (3) BD administered in the ED, and (4) prescription of a BD upon discharge from the ED, as well as associated care outcomes in the ED. Predictors of BD use in the ED with statistical significance were incorporated in a predictive multivariable logistic regression model with a training-validation split of 70%-30%.
Results: Children with prior BD use were significantly more likely than children without such history to receive BD treatment during their current bronchiolitis illness before the ED (OR 23.7, 95%CI 14.4-39), in the ED (OR 2.6, 95%CI 1.76-3.77), and as a prescription upon discharge from the ED (OR 3.7, 95%CI 2.49-5.58). In multivariable regression analyses, older age, parental asthma history, and wheezes and retractions on ED physical exam were significantly associated with BD use in the ED (p < 0.05). The AUC for the validation model with these variables was 0.826 (95%CI 0.794-0.858).
Conclusion(s): Prior BD use was associated with subsequent use during the current illness, during ED care, and subsequent prescription, forming a cyclical pattern. A perceived bronchospastic phenotype of bronchiolitis may influence clinical practice in ED settings. However, whether ED use of BD for bronchiolitis is associated with a discernible phenotype has not been characterized.
Association between clinical characteristics in children with bronchiolitis and the use of a bronchodilator.
.png)
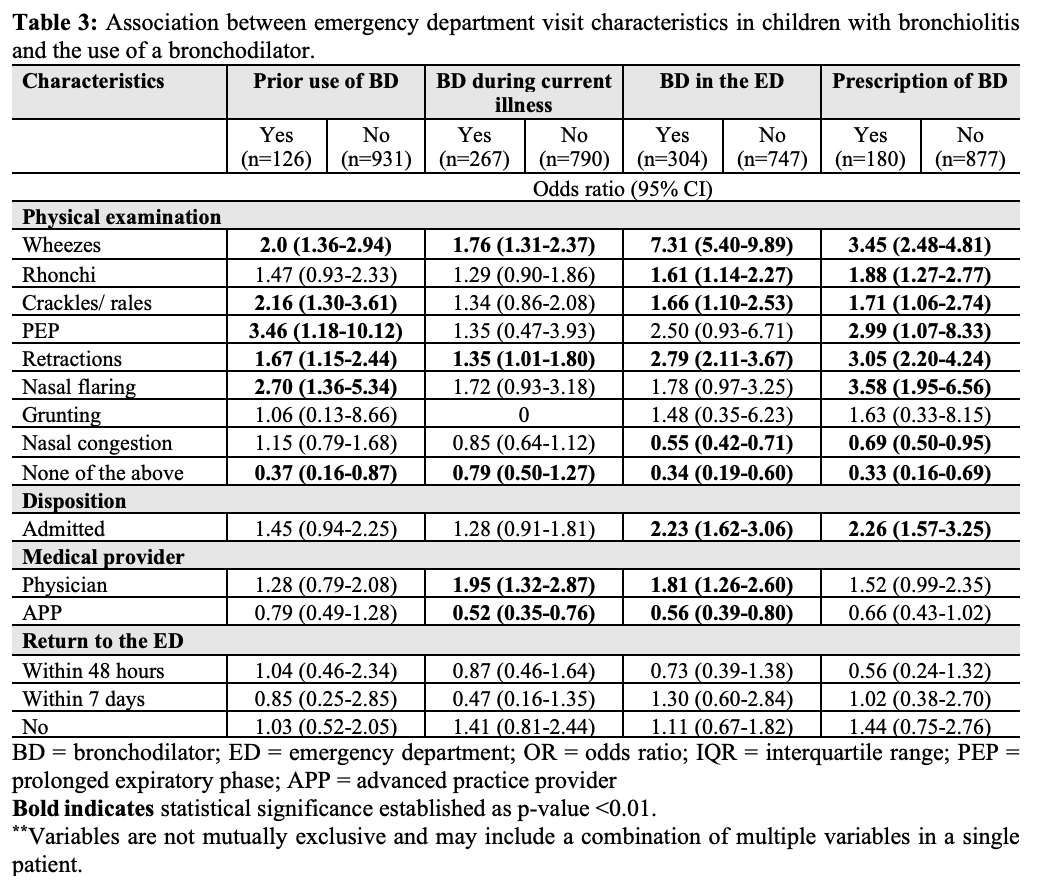
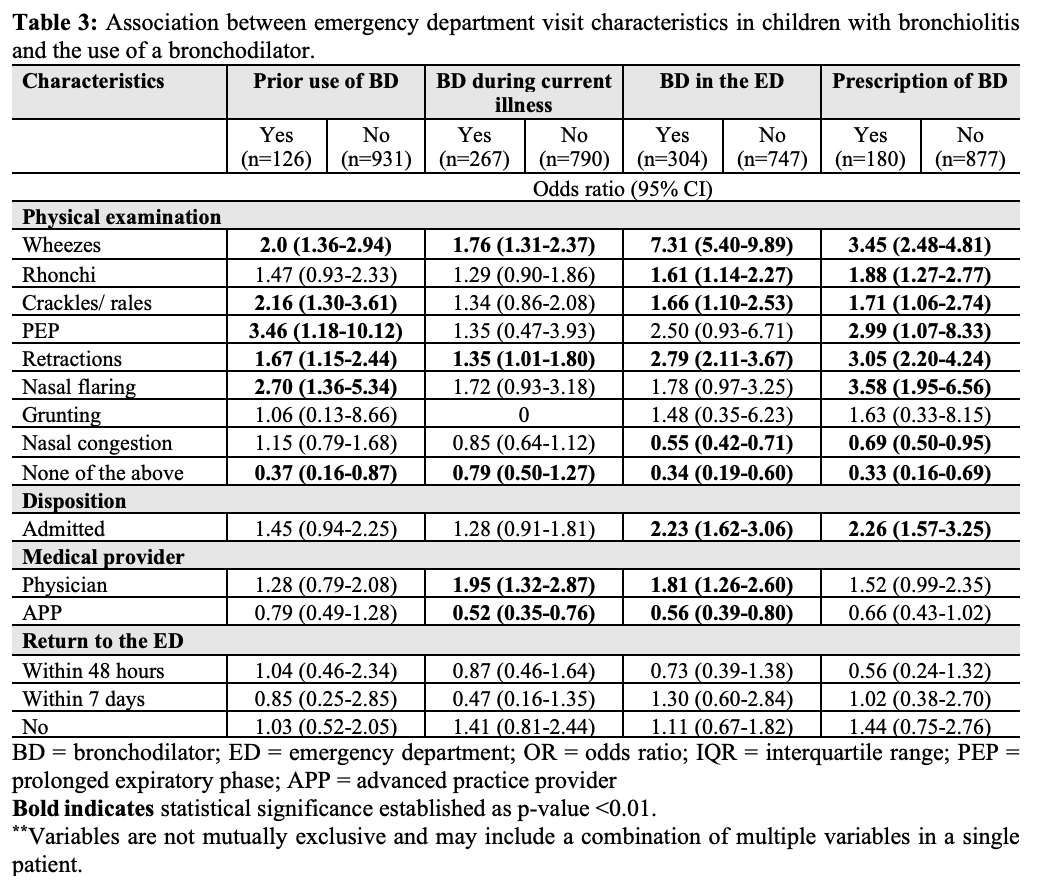
Association between emergency department visit characteristics in children with bronchiolitis and the use of a bronchodilator.
Comparison of the ROC curves
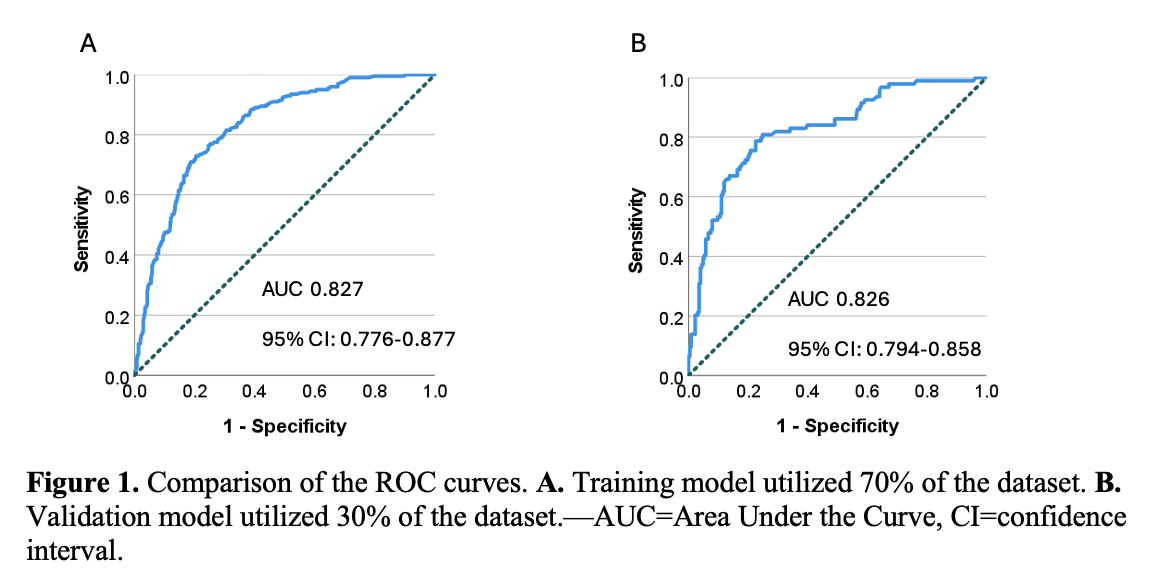 A. Training model utilized 70% of the dataset. B. Validation model utilized 30% of the dataset.—AUC=Area Under the Curve, CI=confidence interval.
A. Training model utilized 70% of the dataset. B. Validation model utilized 30% of the dataset.—AUC=Area Under the Curve, CI=confidence interval.Association between clinical characteristics in children with bronchiolitis and the use of a bronchodilator.
.png)
Association between emergency department visit characteristics in children with bronchiolitis and the use of a bronchodilator.
Comparison of the ROC curves
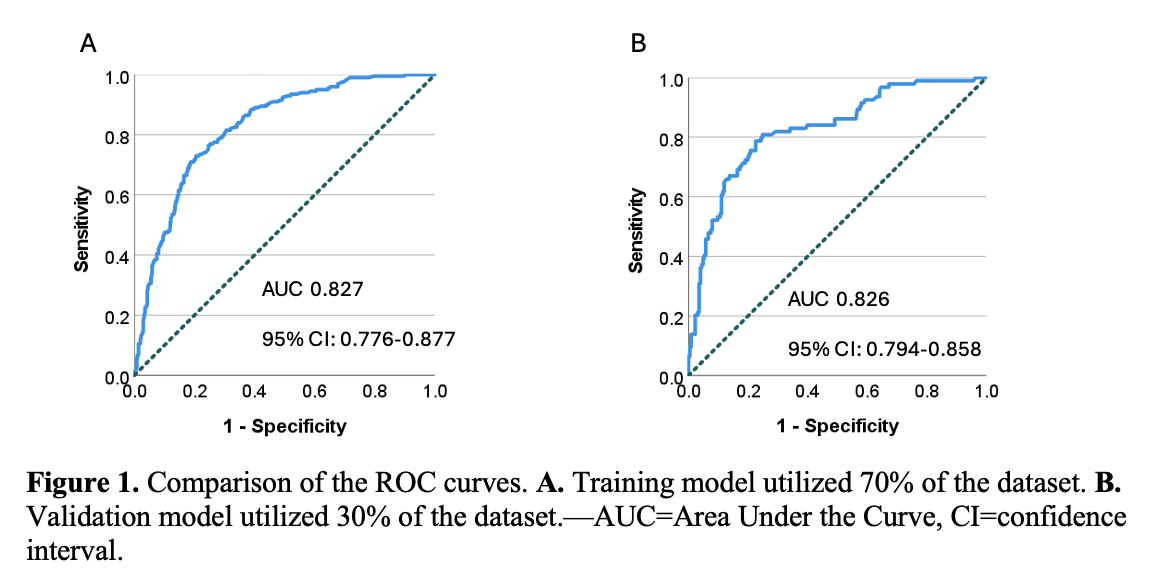 A. Training model utilized 70% of the dataset. B. Validation model utilized 30% of the dataset.—AUC=Area Under the Curve, CI=confidence interval.
A. Training model utilized 70% of the dataset. B. Validation model utilized 30% of the dataset.—AUC=Area Under the Curve, CI=confidence interval.
