General Pediatrics 3
Session: General Pediatrics 3
215 - Early Relational Health Programs in Pediatric Primary Care: Perceived Clinic Needs to Support Implementation
Sunday, April 27, 2025
8:30am - 10:45am HST
Publication Number: 215.4914
Yu Chen, New York University Grossman School of Medicine, New York, NY, United States; Elizabeth Miller, New York University Grossman School of Medicine, NEW ROCHELLE, NY, United States; Janae Kuttamperoor, New York University Grossman School of Medicine, Wayne, NJ, United States; Victoria Guevara, Hassenfeld Children's Hospital at NYU Langone, New York, NY, United States; Diana Walther, NYU Grossman School of Medicine, New York, NY, United States; Hollyce Tyrrell, Academic Pediatric Association, McLean, VA, United States; Shonna Yin, NYU Grossman School of Medicine, New York, NY, United States; Alan L.. Mendelsohn, New York University Grossman School of Medicine, New York, NY, United States; Caitlin F. Canfield, NYU Grossman School of Medicine, New York, NY, United States

Yu Chen, PhD (she/her/hers)
Postdoctoral Fellow
New York University Grossman School of Medicine
New York, New York, United States
Presenting Author(s)
Background: Early relational health (ERH), the presence of safe, stable, nurturing relationships in early life, is crucial in fostering optimal child development and preventing toxic stress responses to adverse experiences. Pediatric primary care has been identified as a key platform for effectively promoting ERH due to its broad reach, ability to capitalize on existing infrastructure, and trust between families and clinicians. However, little is known about whether and how pediatric clinics employ ERH programs and barriers to their implementation.
Objective: The goal of this research was to describe nationwide ERH program utilization, perceived clinic needs related to effective implementation, and whether those needs vary by clinic characteristics (i.e., academic vs. non-academic, percent Medicaid eligible patients, and number of ERH programs offered) or respondent role.
Design/Methods: 131 respondents across 42 clinics were recruited nationally through Academic Pediatric Association’s Continuity Research Network (CORNET), Reach Out and Read, HealthySteps Connect, and the AAP Council on Early Childhood. Respondents participated in an anonymous online survey, which assessed use of evidence-based ERH programs (subscale of Evidence-Based Practices in Pediatric Care) and clinic needs and resources (subscales of Organizational Social Context Scale).
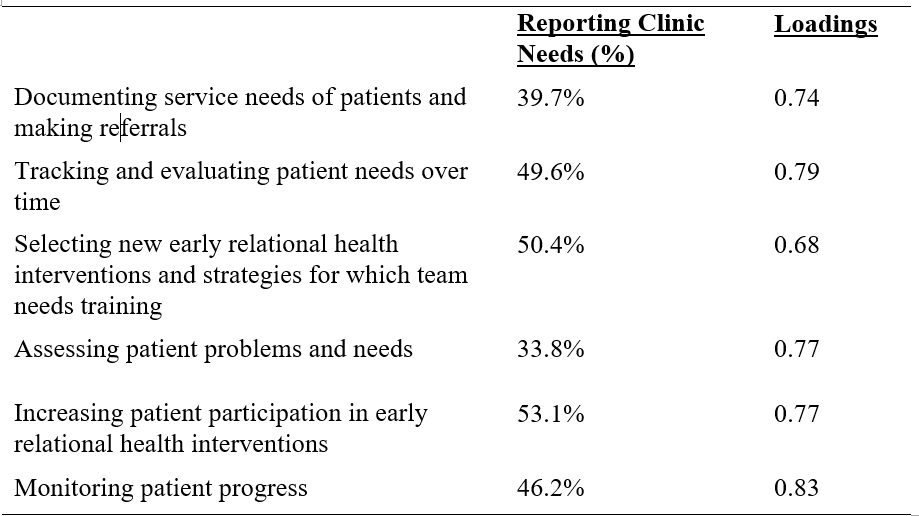
Results: Respondents represented a diverse array of pediatric care roles, geographic locations, and populations served (Table 1). Over 90% of respondents reported having at least one ERH program at their clinic. Of those with ERH programs, 97% had programs on site, 37% had home visiting, and 32% had both modalities. Respondents at academic clinics were more likely to report multiple (vs. 0 or 1) ERH programs (χ2=9.18, p<.01). Respondents reported clinic needs related to documenting, tracking, and evaluating patient needs, as well as training in and encouraging patient participation in ERH programs. Exploratory factor analysis with varimax rotation revealed one factor representing these needs and factor scores were created for analysis (Table 2). Hierarchical regression, including clinic characteristics and respondent role, indicated that the level of perceived clinic needs was associated only with clinic type, with respondents in non-academic clinics reporting higher needs (β=-.19, p<.05).
Conclusion(s): Although most clinics implement multiple ERH programs, further support in assessing and monitoring patients’ needs and progress is needed, especially for non-academic clinics, to effectively utilize evidence-based preventive interventions to best serve children and families.
Table 1. Clinic Characteristics and ERH Program Use
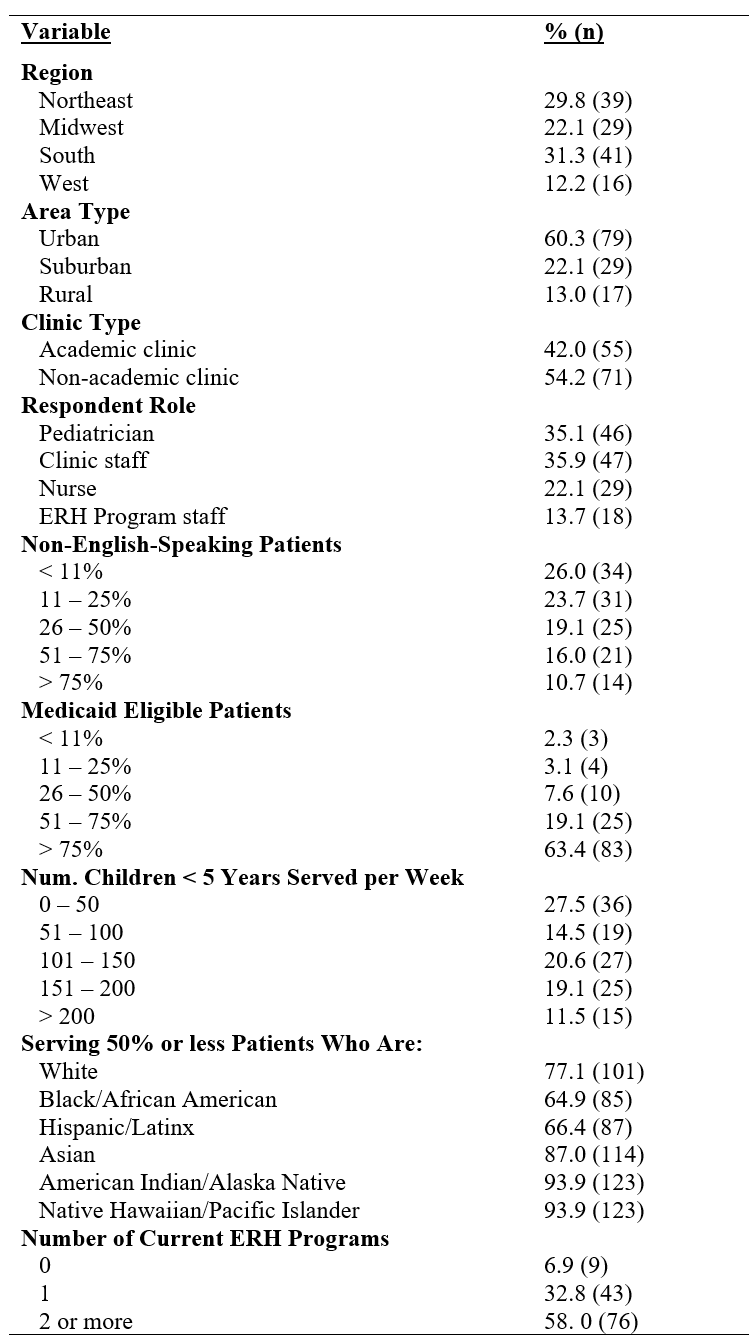
Table 2. Perceived Clinic Needs: Descriptive Data and Exploratory Factor Analysis