Global Neonatal & Children's Health 3
Session: Global Neonatal & Children's Health 3
758 - Epidemiology and Outcomes of Children with Acute Respiratory Infection at a Referral Hospital in Douala, Cameroon
Sunday, April 27, 2025
8:30am - 10:45am HST
Publication Number: 758.5000
Bianca M. Nfonoyim Bernhard, Children's Hospital of Philadelphia, Cherry Hill, NJ, United States; Madeline Chandra, Perelman School of Medicine at the University of Pennsylvania, Philadelphia, PA, United States; Lucie V. Ngaba, Philadelphia College of Osteopathic Medicine, Philadelphia, PA, United States; Arsen Edzogo, Laquintinie Hospital in Douala, Douala, Sud-Ouest, Cameroon; Betsy B. Bate, Laquintinie Hospital Douala, Douala, Littoral, Cameroon; Kathleen Miller, Childrens Hospital of Philadelphia, Philadelphia, PA, United States; Sahr Yazdani, Childrens Hospital of Philadelphia, Philadelphia, PA, United States; Niharika Shukla, Perelman School of Medicine, Philadelphia, PA, United States; Leonel E. Toledo, Childrens Hospital of Philadelphia, Cinnaminson, NJ, United States; Charlotte Ekoube. Eposse, Faculty of médecine and pharmaceutical sciences, university of Douala, Douala, Littoral, Cameroon; Andrew P. Steenhoff, Children's Hospital Of Philadelphia & Univ Of Pennsylvania, Philadelphia, PA, United States; Madiha Raees, Childrens Hospital of Philadelphia, Philadelphia, PA, United States

Bianca Nfonoyim Bernhard, MD (she/her/hers)
Pediatrics resident
Children's Hospital of Philadelphia
Cherry Hill, New Jersey, United States
Presenting Author(s)
Background: Most childhood deaths from acute respiratory illnesses (ARI) are preventable, partially due to advanced technologies such as non-invasive positive pressure ventilation. Children in low-and middle-income countries have a high risk of mortality from ARI, even in large, tertiary referral centers such as Laquintinie Hospital (LHD) in Douala, Cameroon. To prioritize limited resources and inform future investigations, it is critical to characterize the current burden of ARI in LHD.
Objective: We sought to analyze children under age 5 years presenting with an ARI at LHD to identify characteristics associated with in-hospital mortality.
Design/Methods: This was a retrospective chart review completed on children under 5 years presenting from 2022-2023 to LHD emergency department with an ARI. Children with known cardiac or lung disease, trauma, or prematurity were excluded. We utilized chi-square, Mann-Whitney U, regression analysis and Spearman correlation in Stata (College Station, TX). This study was approved by the CHOP (23-020901) and LHD IRBs.
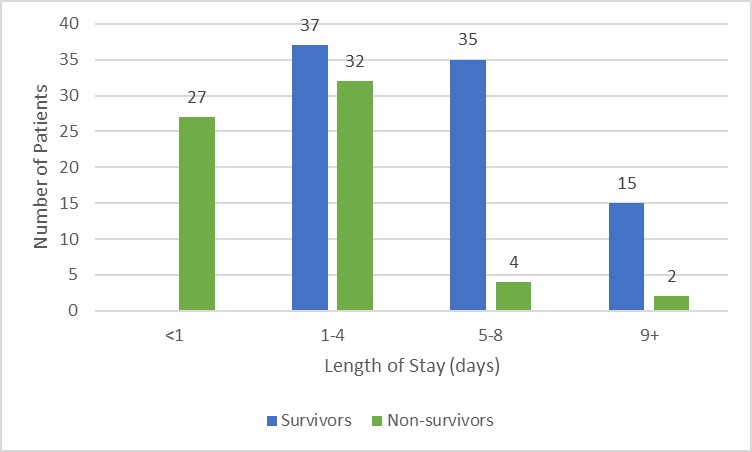
Results: One hundred fifty-two patient records were analyzed; demographics are summarized in Table 1. The most common admission diagnosis was pneumonia (56%, n=85), followed by bronchiolitis (32%, n=48) (Figure 1). Most children (78%, n=119) did not receive chest radiographs. Laboratory testing beyond glucose, malaria testing, and blood counts were uncommon. Ninety-five percent (n=145) of children received antibiotics. Low-flow oxygen was utilized in 94% (n=143). Mortality was 43% (n=65); 42% (n=27) of these children died in the first 24 hours of presentation (Figure 2). Length of stay inversely correlated with mortality (r-value –0.7, p< 0.01). Patients who died had higher median temperatures, white blood cell counts, and lower hemoglobin (p < 0.05). A diagnosis of bronchiolitis was associated with a decreased odds of mortality (OR 0.24, p 0.001, CI 0.10-0.57), while a diagnosis of COVID was associated with increased odds of mortality (OR 4.05, p 0.024, CI 1.20-13.65). Among survivors, median discharge Pediatric Overall Performance Category was 1 (IQR 1-2).
Conclusion(s): Mortality was high and occurred early in admission, suggesting late presentation and the potential to improve pre-hospital care. Given the frequent use of oxygen, access to additional respiratory support such as bubble CPAP could improve outcomes for children with ARI in Douala. Future directions include prospective observational studies, including closer evaluation of factors like malnutrition.
Table 1: Patient Characteristics
.jpg)
Figure 1: Comparing mortality by primary diagnosis on admission
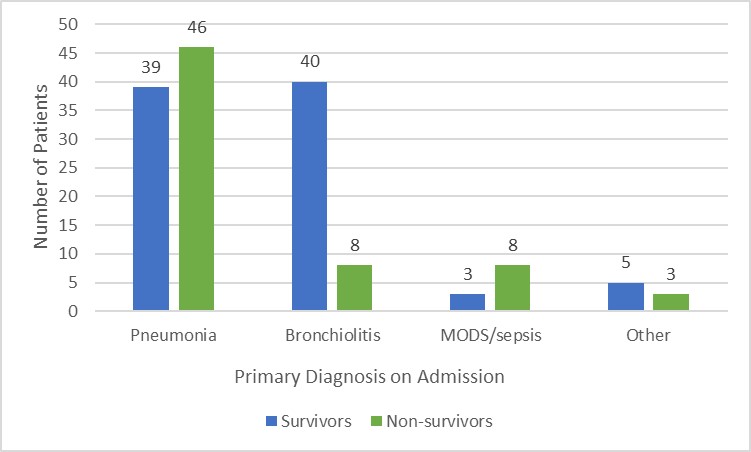
Figure 2: Comparing mortality by length of stay