Emergency Medicine 8
Session: Emergency Medicine 8
113 - Evolving epidemiology of acute rhinovirus infection following the COVID-19 pandemic
Sunday, April 27, 2025
8:30am - 10:45am HST
Publication Number: 113.5021
Karla F. Vazquez- De Jesus, University of Utah School of Medicine, Salt Lake City, UT, United States; Aksel E. Anderson, Primary Children's Hospital, Salt Lake City, UT, United States; Zhining Ou, University of Utah - Salt Lake City, UT, Salt Lake City, UT, United States; Anne J.. Blaschke, University of Utah School of Medicine, Salt Lake City, UT, United States; Michael D.. Johnson, University of Utah School of Medicine, Bountiful, UT, United States
- KV
Karla F. Vazquez- De Jesus, MD, MBA (she/her/hers)
PEM Fellow
University of Utah School of Medicine
Salt Lake City, Utah, United States
Presenting Author(s)
Background: Rhinovirus is a common cause of respiratory infections and wheezing illnesses in young children, often leading to emergency department (ED) visits for asthma-like symptoms treated with albuterol. Mitigation strategies related to the COVID-19 pandemic affected the circulation of all respiratory viral pathogens, potentially altering the epidemiology of rhinovirus infections and increasing rhinovirus-induced wheezing illness.
Objective: This study aims to characterize changes in the epidemiology and clinical nature of rhinovirus infection related to the COVID-19 pandemic.
Design/Methods: We considered all children aged 0-17 who received care at any ED in a large regional healthcare system between 2017-2023 for a first-time wheezing episode. An episode was defined as either the administration of albuterol or a qualifying ICD diagnosis (wheezing R06.2, bronchospasm J98.01, or asthma J45.xx) with no prior asthma diagnosis (J45.xx) to the index visit. Data was electronically abstracted from health records and compared across three time periods: pre-COVID defined from 2017 to the first locally reported case of COVID (January 2017 - February 2020), COVID until the first available COVID vaccine (March 2020 - February 2021), and post-COVID (March 2021 onward). We assessed three outcomes using multivariable modified Poisson regression: rhinovirus test positivity, hospitalization for rhinovirus-positive episodes, and continued albuterol treatment during hospitalization. COVID-19 period was the primary predictor of interest, adjusted for age, sex, race, state-level Child Opportunity Index of the child’s zip code, and season.
Results: We analyzed 6823 episodes: 3460 pre-COVID, 297 during COVID, and 3066 post-COVID. The proportion of children with viral testing who were positive for rhinovirus was 33.3% pre-COVID, 52.5 % during COVID, and 44.4% post-COVID. Hospitalization rates of children testing positive for rhinovirus were 38.2 % pre-COVID, 25.8 % during COVID, and 44.7 % post-COVID. Among hospitalized children, 15.2% pre-COVID, 12.5% during COVID, and 17.4% post-COVID continued to receive albuterol in the last 6 hours of hospitalization. In multivariable analysis, risk of rhinovirus positive was higher post-COVID than pre-COVID (p = 0.016), although the risk of hospitalization and continued albuterol treatment for patients with rhinovirus were unchanged.
Conclusion(s): Rhinovirus is a more dominant viral trigger of first-time wheezing in children after the COVID-19 pandemic but is not more likely to lead to hospitalization or lead to continued asthma treatment during hospitalization.
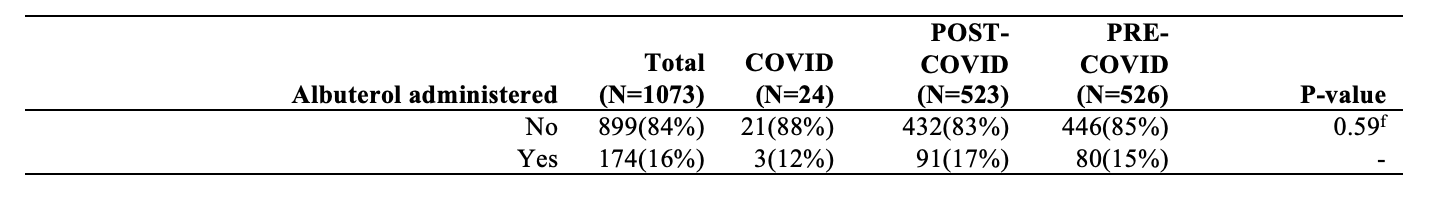
Demographics of study episodes
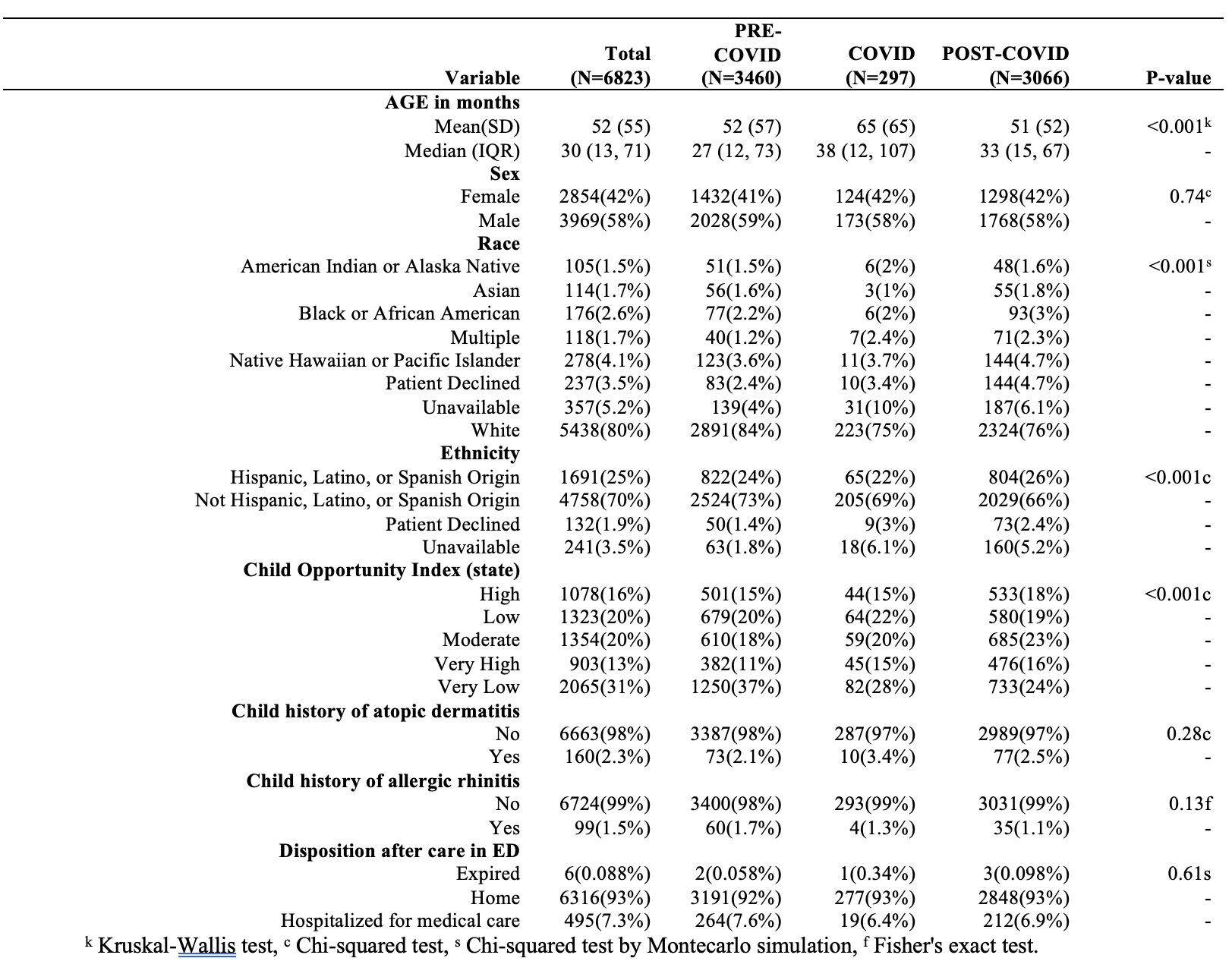
Viral results for episodes in whom rhinovirus was tested
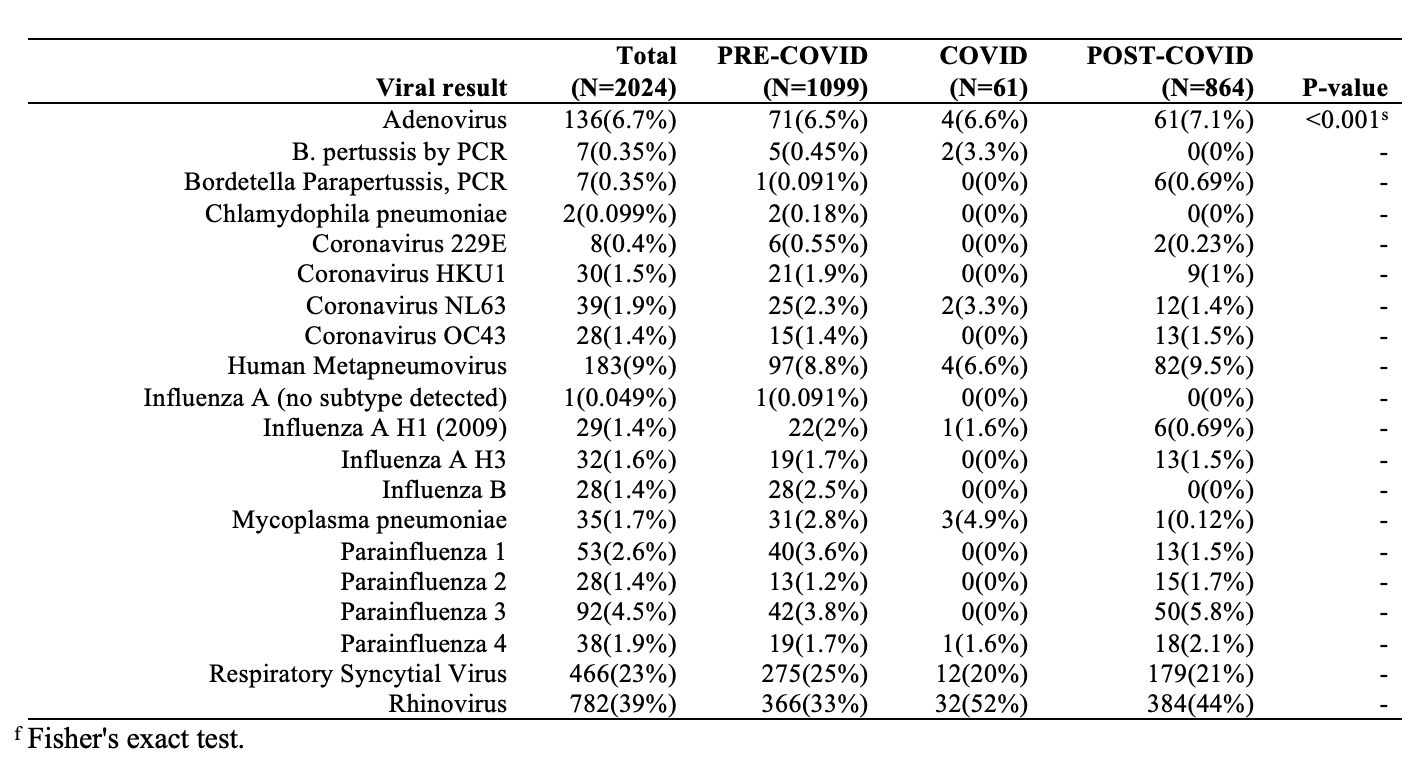
Administration of albuterol within 6 hours of hospital discharge – limited to patients hospitalized after treatment with albuterol in the ED with results positive for rhinovirus