Health Equity/Social Determinants of Health 5
Session: Health Equity/Social Determinants of Health 5
717 - Racial and Ethnic Disparities in Vaccination Rates Among Infants with Bronchopulmonary Dysplasia
Sunday, April 27, 2025
8:30am - 10:45am HST
Publication Number: 717.6097
Mallory Go, Brown University, Providence, RI, United States; Robin McKinney, HASBRO CHILDREN'S HOSPITAL, PROVIDENCE, RI, United States; Natasha Sokol, The Warren Alpert Medical School of Brown University, Providence, RI, United States; Shilo H. McBurney, Brown University School of Public Health, Providence, RI, United States; Sara Conroy, Nationwide Children's Hospital, Columbus, OH, United States; Joseph Collaco, Johns Hopkins Children's Center, Baltimore, MD, United States; Valery A. Danilack-Fekete, Yale School of Medicine, Old Saybrook, CT, United States

Mallory Go (she/they)
Researcher
Brown University
Providence, Rhode Island, United States
Presenting Author(s)
Background: Minoritized children with bronchopulmonary dysplasia (BPD) are at high risk of respiratory morbidity in early childhood. Vaccination is an important tool in the prevention of respiratory infection-related morbidity. Racial and ethnic disparities in vaccination rates may contribute to disparate respiratory outcomes in infants with BPD.
Objective: (1) To compare racial and ethnic differences in vaccination rates of influenza and RSV among infants with BPD (2) To estimate the association of vaccination rates of influenza and RSV with adverse health outcomes in infants with BPD.
Design/Methods: We analyzed 1,574 patients from the BPD Collaborative Outpatient Registry with complete data. Mixed-effects logistic regression models examined associations for vaccination status (primary outcome) with child race/ethnicity (primary exposure). Secondary analysis used logistic regression to estimate the association of rescue medication and oral steroid use (secondary outcome) with vaccination status (secondary exposure). Confounders were selected based on literature and data availability.
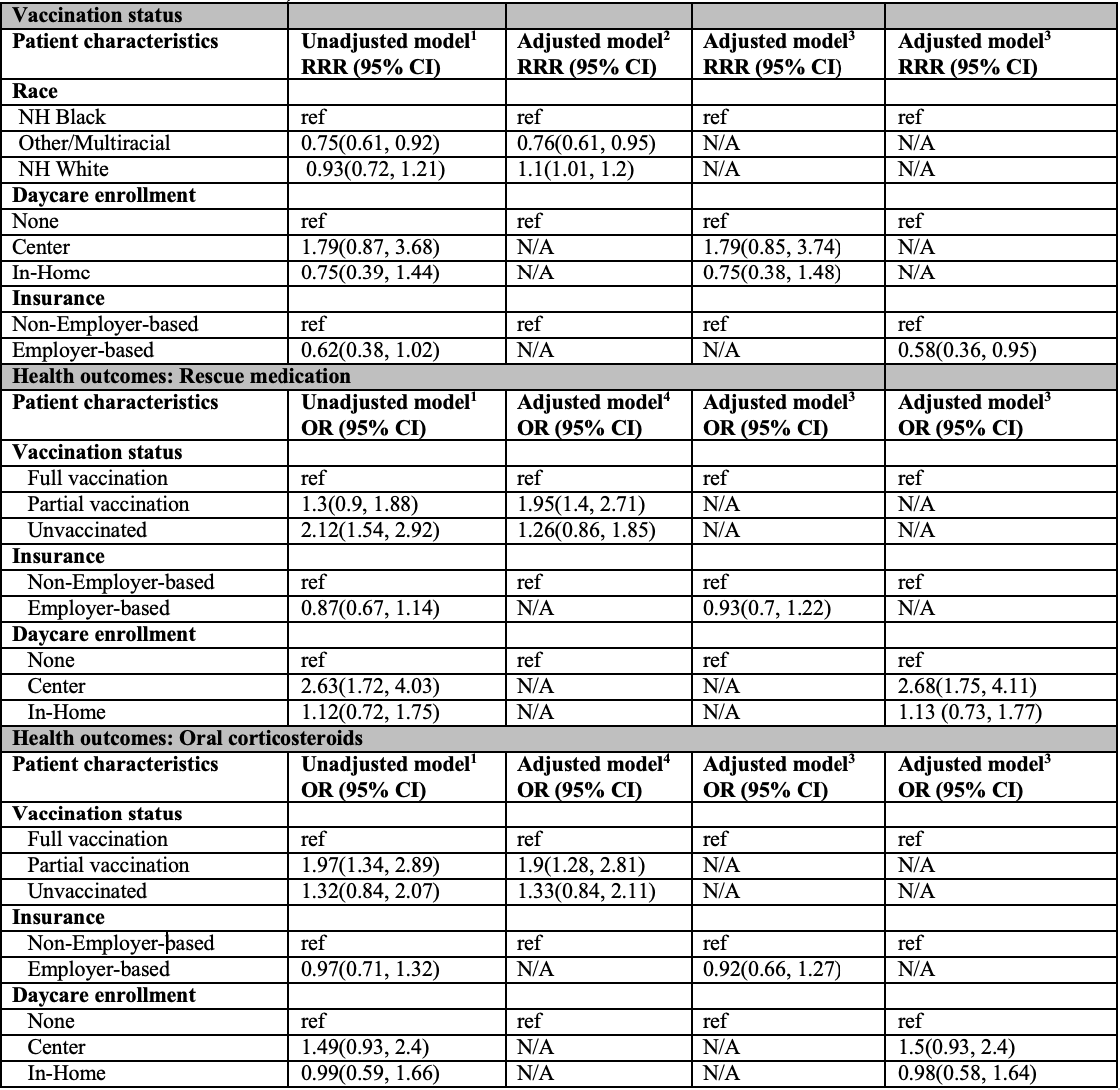
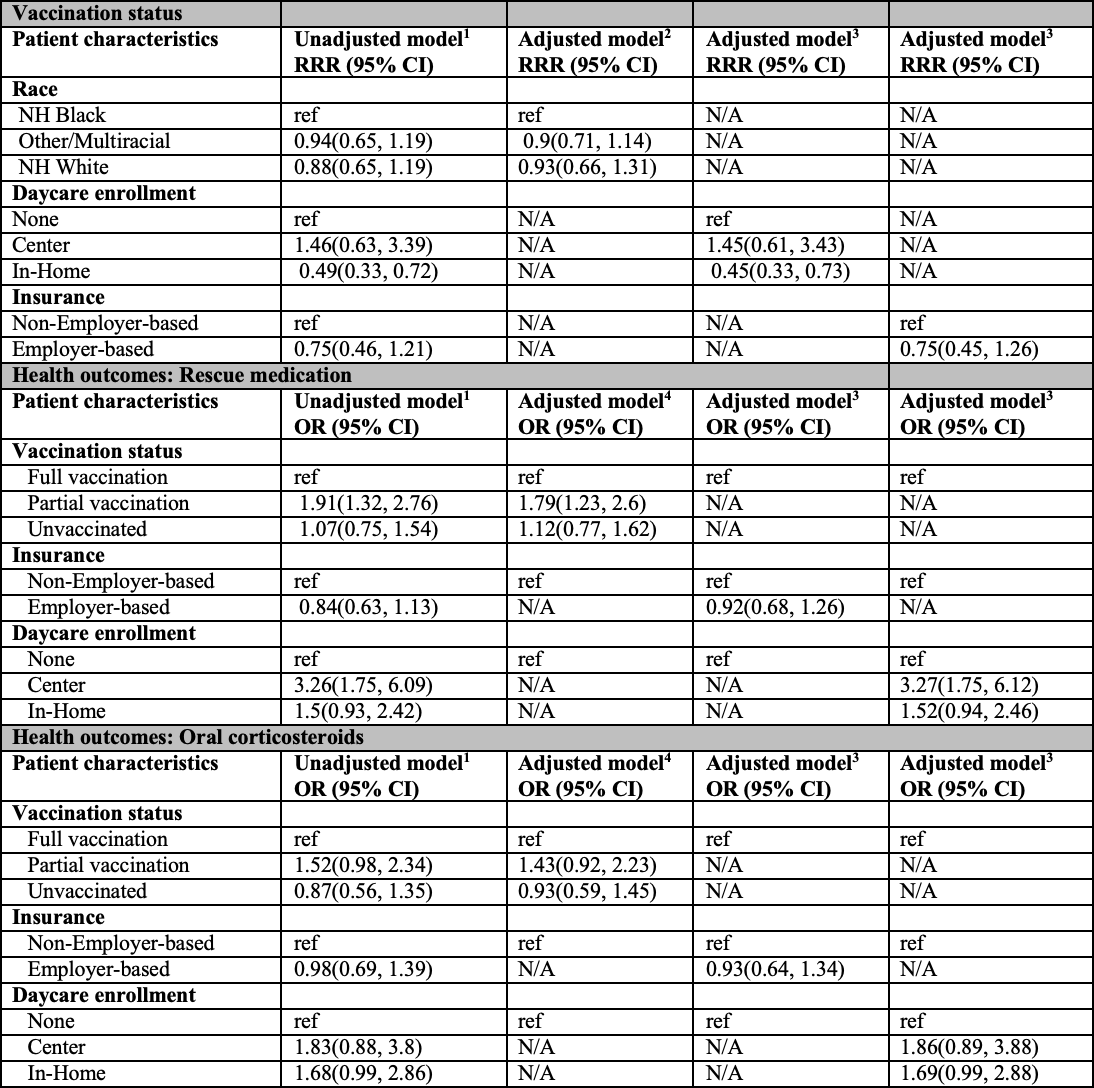
Results: The percentage of non-Hispanic Black patients unvaccinated for both influenza and RSV was 27% and 40% respectively, while the percentage for non-Hispanic White patients was approximately 24% and 36% respectively (Table 1). There was not significant evidence that adjusted vaccination rates between groups for influenza or RSV was lower for NH White infants compared to NH Black infants (Influenza Relative Risk Ratio (RRR): 1.1 (95% CI: 1.01-1.2), (RSV RRR: 0.93 (95% CI: 0.66-1.31)) after controlling for confounders (Tables 2-3). The odds of rescue medication use were higher for infants with partial vaccination compared to those with full vaccination for both influenza (aOR: 1.95 (95% CI: 1.4-2.71, p< 0.001) and RSV (aOR: 1.79 (95% CI: 1.23-2.6, p=0.002) (Tables 2-3). Additionally, the odds of oral steroid use were higher for infants with partial vaccination compared to those with full vaccination only for influenza (aOR: 1.9 (95% CI: 1.28-2.81) but not RSV (aOR: 1.43 (95% CI: 0.92-2.23). The odds of rescue medication use were higher for patients enrolled in-center daycare for both influenza (aOR: 2.68 (95% CI: 1.75, 4.11) and RSV (aOR: 3.27 (95% CI: 1.75, 6.12).
Conclusion(s): Vaccination status was not significantly associated with infant race and ethnicity for both influenza and RSV. However, incomplete vaccination status for both influenza and RSV was associated with increased odds of rescue medication and oral steroid use, compared to fully vaccinated patients.
Table 1: Descriptive Statistics
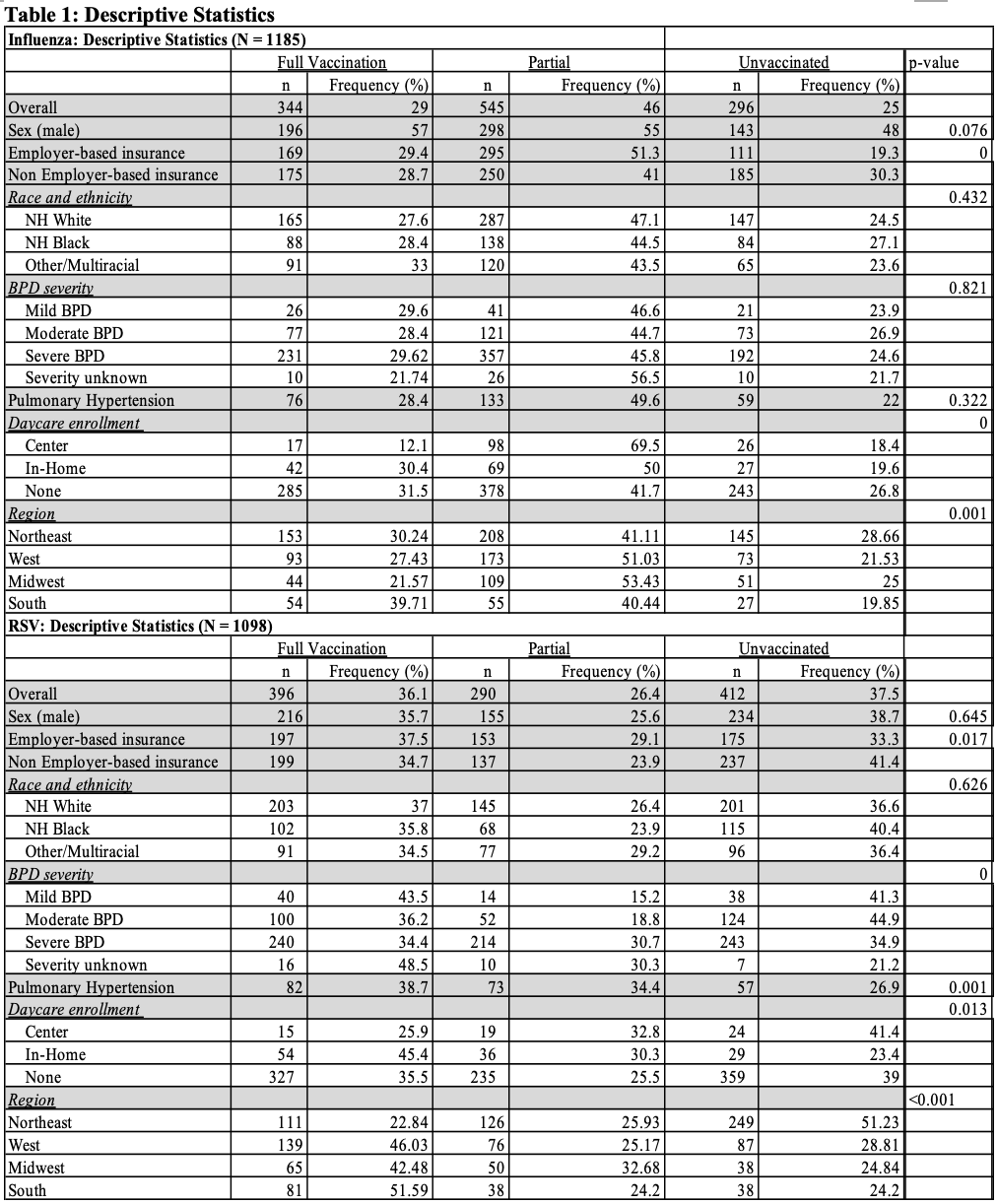
Table 2: Relative risk ratios and odds ratios for association between patient characteristics influenza vaccination, and adverse health outcomes
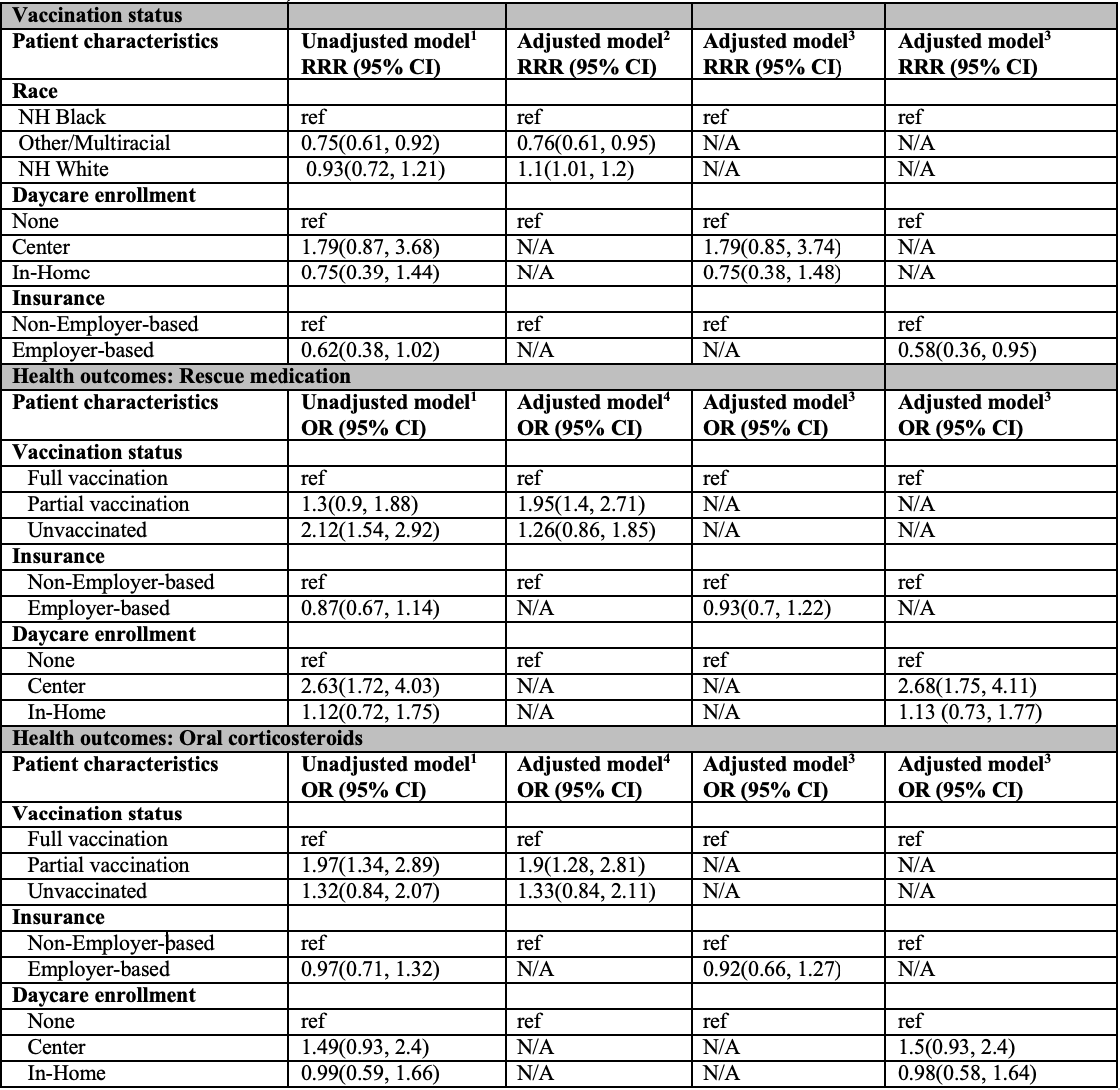 RRR: relative risk ratio
RRR: relative risk ratio OR: odds ratio
CI: confidence interval
All models are adjusted for clustering by geographic region
1 unadjusted for confounders
2 adjusted for infant sex, insurance status, daycare enrollment, pulmonary hypertension, BPD severity
3 adjusted for aggregated race
4 adjusted for aggregated race, infant sex, insurance status, daycare enrollment, pulmonary hypertension, BPD severity
Table 3: Relative risk ratios and odds ratios for association between patient characteristics RSV vaccination, and adverse health outcomes
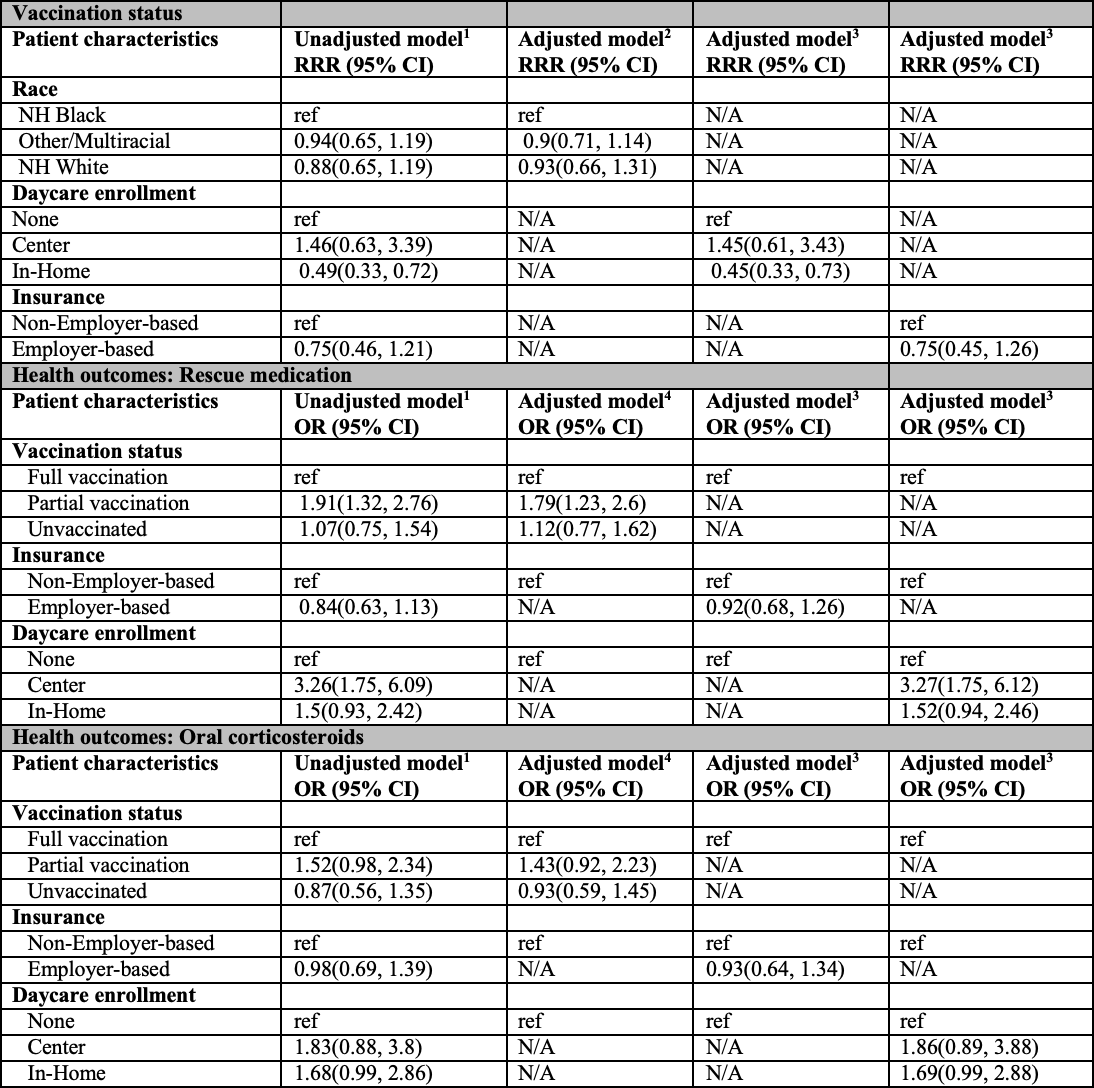 RRR: relative risk ratio
RRR: relative risk ratio OR: odds ratio
CI: confidence interval
All models are adjusted for clustering by geographic region
1 unadjusted for confounders
2 adjusted for infant sex, insurance status, daycare enrollment, pulmonary hypertension, BPD severity
3 adjusted for aggregated race
4 adjusted for aggregated race, infant sex, insurance status, daycare enrollment, pulmonary hypertension, BPD severity
Table 1: Descriptive Statistics
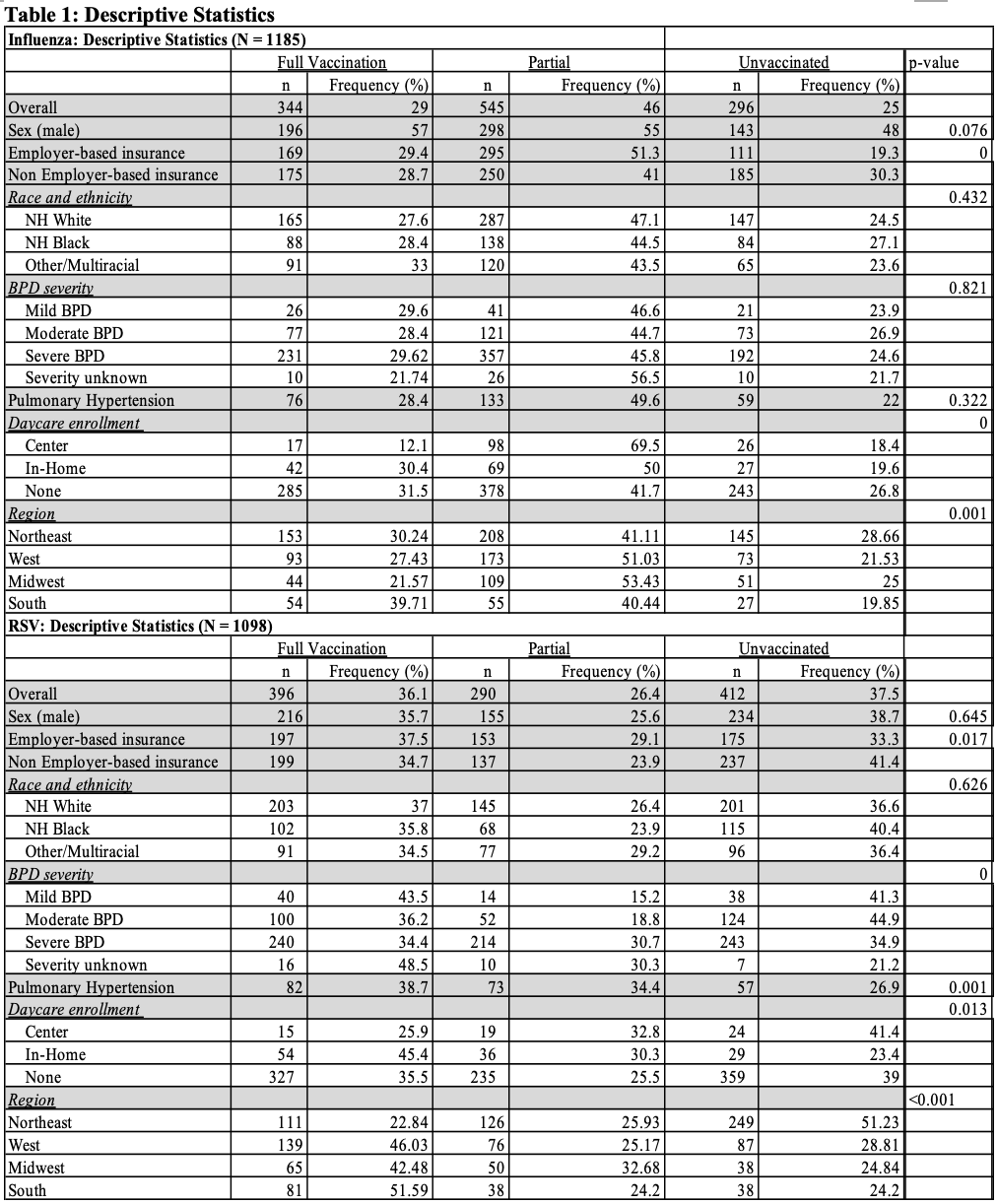
Table 2: Relative risk ratios and odds ratios for association between patient characteristics influenza vaccination, and adverse health outcomes
 RRR: relative risk ratio
RRR: relative risk ratio OR: odds ratio
CI: confidence interval
All models are adjusted for clustering by geographic region
1 unadjusted for confounders
2 adjusted for infant sex, insurance status, daycare enrollment, pulmonary hypertension, BPD severity
3 adjusted for aggregated race
4 adjusted for aggregated race, infant sex, insurance status, daycare enrollment, pulmonary hypertension, BPD severity
Table 3: Relative risk ratios and odds ratios for association between patient characteristics RSV vaccination, and adverse health outcomes
 RRR: relative risk ratio
RRR: relative risk ratio OR: odds ratio
CI: confidence interval
All models are adjusted for clustering by geographic region
1 unadjusted for confounders
2 adjusted for infant sex, insurance status, daycare enrollment, pulmonary hypertension, BPD severity
3 adjusted for aggregated race
4 adjusted for aggregated race, infant sex, insurance status, daycare enrollment, pulmonary hypertension, BPD severity

