Hospital Medicine 3: Systems/Population-based Research
Session: Hospital Medicine 3: Systems/Population-based Research
141 - Familial and Provider Communication During Pediatric Rapid Response Activation
Sunday, April 27, 2025
8:30am - 10:45am HST
Publication Number: 141.5078
Tammy Wang, Frank H. Netter MD School of Medicine at Quinnipiac University, New York, NY, United States; Kelley A. Groves, Hassenfeld Children's Hospital at NYU Langone, New York, NY, United States; Ami Shah, Hassenfeld Children's Hospital at NYU Langone, New York, NY, United States; Kristyn Pierce, New York University Grossman School of Medicine, New York, NY, United States
.jpg)
Tammy Wang, BA (she/her/hers)
Medical Student
Hassenfeld Children's Hospital at NYU Langone, New York, United States
Presenting Author(s)
Background: Effective management of acute clinical deterioration in hospitalized children relies on Pediatric Rapid Response Activations (PRRAs). Challenges such as incomplete involvement of the floor team, communication barriers between physicians and nurses, and sociocultural barriers between providers and families can delay PRRAs and compromise patient care.
Objective: This study aims to (1) conduct a retrospective chart review to analyze patient demographics, PRRA indications, language preferences, interpreter use, family communication, and medical interventions, and (2) explore stressors and communication during PRRAs through qualitative interviews with patient family members and healthcare workers.
Design/Methods: This mixed-methods study, approved by the institutional IRB in July 2024, includes an anticipated retrospective 5-year chart review (REDCap, Jan 1, 2019 to Dec 31, 2020) and semi-structured interviews with patients’ family members and healthcare workers who experience PRRAs to assess perceptions, stressors, communication, and feedback on the family presence facilitator concept. Descriptive statistics evaluated demographics, language preferences, PRRA interventions, and Pediatric Intensive Care Unit (PICU) outcomes. Thematic content analysis identified key themes from qualitative interview transcripts.
Results: Results demonstrate that 82.5% of patients requiring a PRRA were transferred to the PICU. Forty-eight percent of activations had documentation of a Pediatric Early Warning Score (PEWS), and none of the documented PEWS were accurate. Documentation of preferred language was significantly higher in English-speaking families (100%) compared to non-English speaking families (83%, p < 0.01). Additional statistics on patient demographics, reasons for PRRA, and interventions required during PRRA are in Tables 1-4. Qualitative data highlights tensions between teams: the responding PICU team expressed concerns about stress and overcrowding and questioned the need for their involvement, while the floor team felt the interaction was more about justifying the need for PICU care rather than a collaborative discussion (Figure 1).
Conclusion(s): This study reveals significant differences in language documentation during PRRAs between English and non-English preferring families. Gaps in documentation, including missing PEWS, and qualitative feedback from team members emphasize the need for improved communication and support during PRRAs. Future studies should assess the impact of interventions to enhance family experience, communication and documentation during PRRAs.
Table 1-4
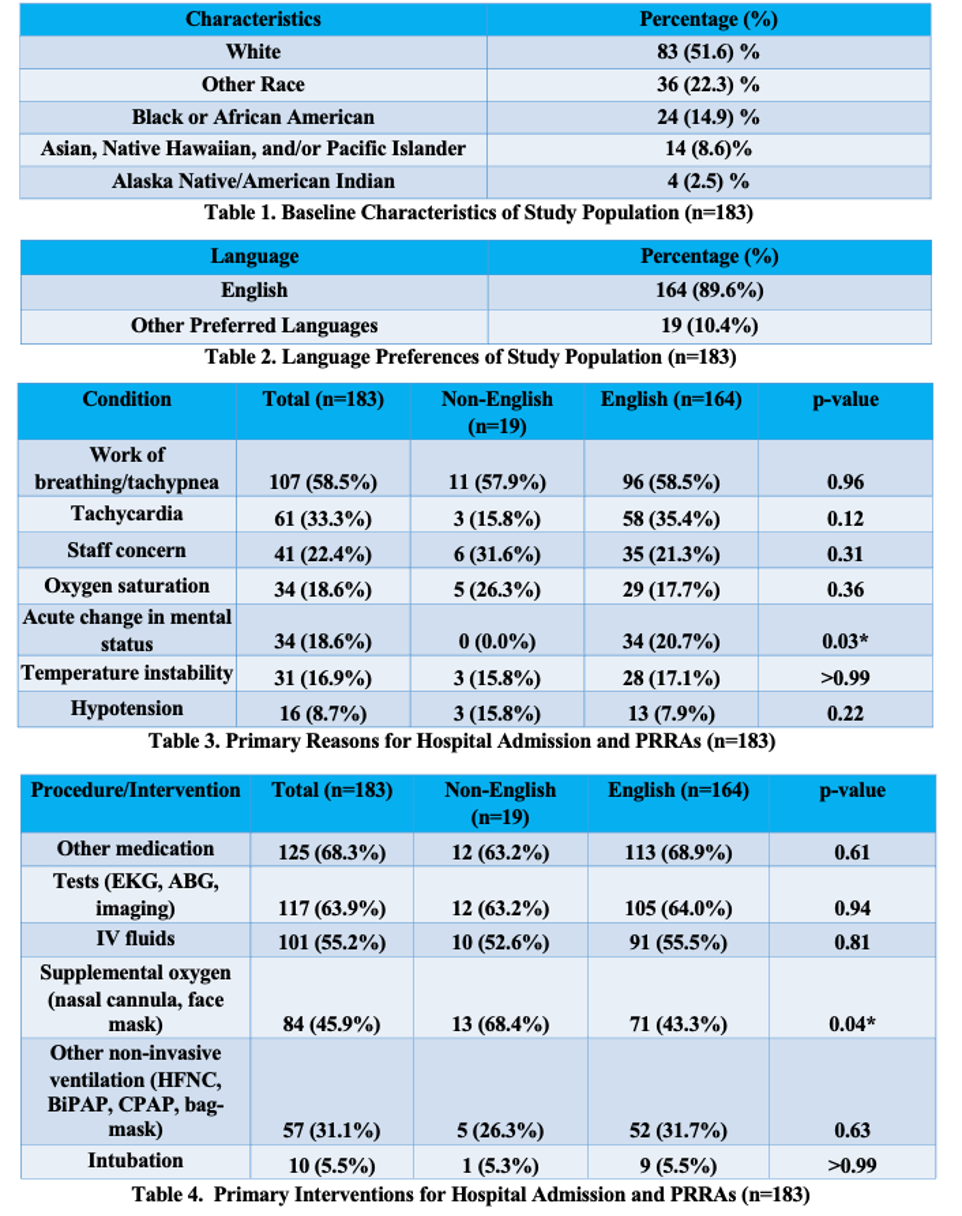 Table 1. Baseline Characteristics of Study Population
Table 1. Baseline Characteristics of Study PopulationTable 2. Language Preferences of Study Population
Table 3. Primary Reasons for Hospital Admission and PRRAs
Table 4. Primary Interventions for Hospital Admission and PRRAs
Figure 1
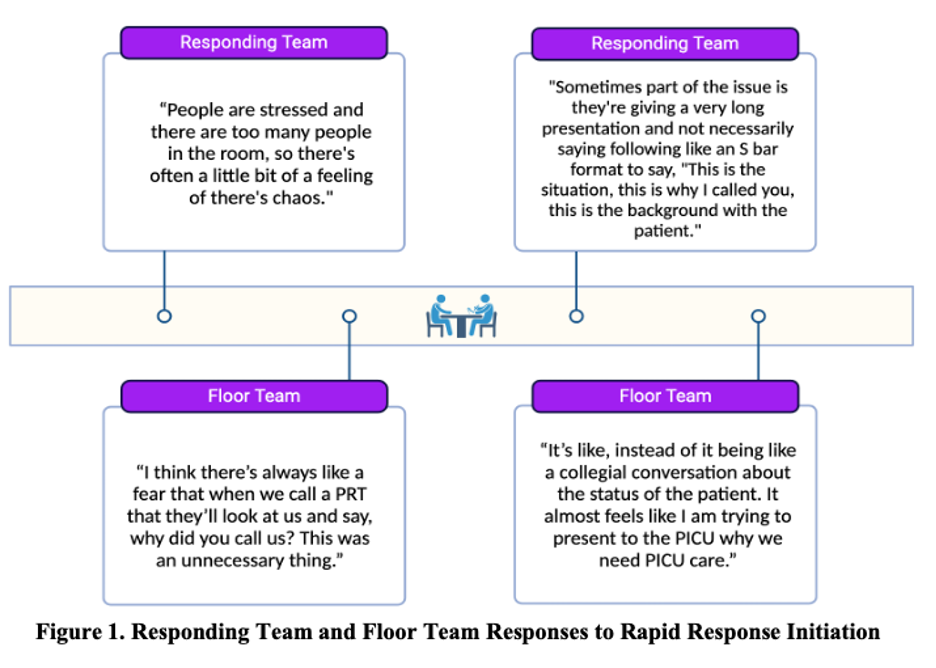 Responding Team and Floor Team Responses to Rapid Response Initiation
Responding Team and Floor Team Responses to Rapid Response Initiation
