Endocrinology 1
Session: Endocrinology 1
303 - Growth and Metabolic Outcomes of Neonates with Hyperinsulinism
Sunday, April 27, 2025
8:30am - 10:45am HST
Publication Number: 303.5137
Sheri VanOmen, University of Michigan Medical School, Ann Arbor, MI, United States; Nellie S. Said, University of Michigan Medical School, Ann Arbor, MI, United States; Julie Sturza, University of Michigan Medical School, Ann Arbor, MI, United States; Brigid Gregg, University of Michigan Medical School, Ann Arbor, MI, United States; Lindsay Ellsworth, University of Michigan Medical School, Chelsea, MI, United States

Sheri VanOmen, MD (she/her/hers)
Clinical Assistant Professor, Neonatal-Perinatal Medicine
University of Michigan Medical School
Ann Arbor, Michigan, United States
Presenting Author(s)
Background: Neonatal hyperinsulinism is a common cause of persistent hypoglycemia in infants and increases the risk of long-term morbidity. There is an association between hyperinsulinism and higher birth weight, however there are no studies assessing the relationship between neonatal hyperinsulinism and long-term growth trajectory beyond the neonatal period.
Objective: To characterize a cohort of neonates with hyperinsulinism evaluating comorbidities and related medical or surgical interventions. To evaluate growth outcomes and weight trajectory over the first 6 months of life.
Design/Methods: A retrospective chart review was performed on eligible patients, between 2010-2022 at an academic children’s hospital, with a diagnosis of neonatal hyperinsulinism (defined by an insulin level >2 microU/mL within the first month of life). Patients were classified into groups based on presence/absence of signification comorbidities and the need for medical and/or surgical intervention for hyperinsulinism. Data were collected for birth history, demographics, management of hyperinsulinemia, feeding support, and lab values. Infant growth data included weight-for-age (WFA), length-for-age (LFA), and weight-for-length (WFL) with Z-scores calculated at birth and near 6 months of age. Slow, on track, and rapid growth were determined based on change in Z-score. Descriptive statistics were used to describe the whole sample and subgroups. Differences between groups were determined using Fisher's exact test and ANOVA.
Results: A total of 32 infants were included with an average gestational age of 37.9 weeks, 7 (22%) infants of diabetic mothers, and 13 (41%) significant comorbidities (Table 1). From the full cohort, 19 (59%) infants required intervention with 17 (90%) medication and 2 (10%) surgery. Analysis of growth outcomes demonstrated a significant difference in LFA Z-score at 6 months between infants with and without significant comorbidities (Table 2). There were no significant differences in growth outcomes in infants without significant comorbidities based on requiring intervention (Table 3). When evaluating growth trajectory in the full cohort, 6 (10%) of infants had a rapid weight gain Z-score and 17 (53%) had a slow weight gain Z-score.
Conclusion(s): In this single center study, half of neonates with hyperinsulinism had slow weight gain in the first months of life with no difference in growth outcomes based on the infant receiving medical/surgical intervention. Further studies in larger cohorts are needed to investigate how intervention may be associated with growth trajectories and future long-term metabolic disease risk.
Table 1: Neonatal hyperinsulinism cohort characteristics.
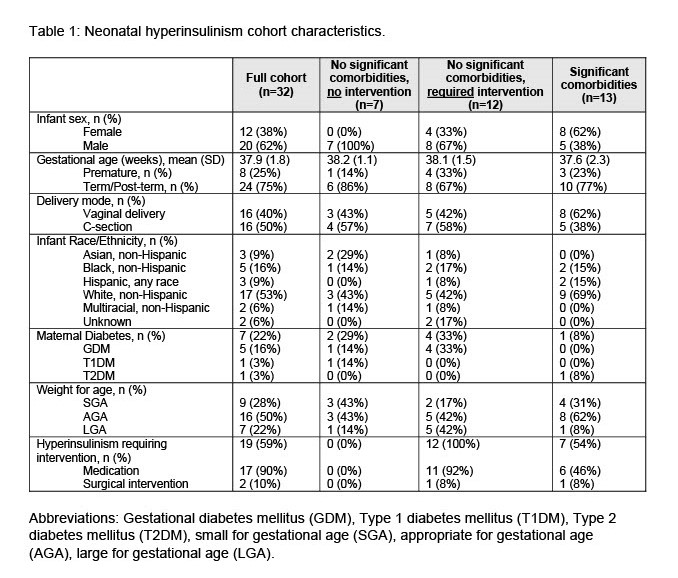 Abbreviations: Gestational diabetes mellitus (GDM), Type 1 diabetes mellitus (T1DM), Type 2 diabetes mellitus (T2DM), small for gestational age (SGA), appropriate for gestational age (AGA), large for gestational age (LGA).
Abbreviations: Gestational diabetes mellitus (GDM), Type 1 diabetes mellitus (T1DM), Type 2 diabetes mellitus (T2DM), small for gestational age (SGA), appropriate for gestational age (AGA), large for gestational age (LGA).Table 2: Growth outcomes for the full cohort including infants with and without significant comorbidities.
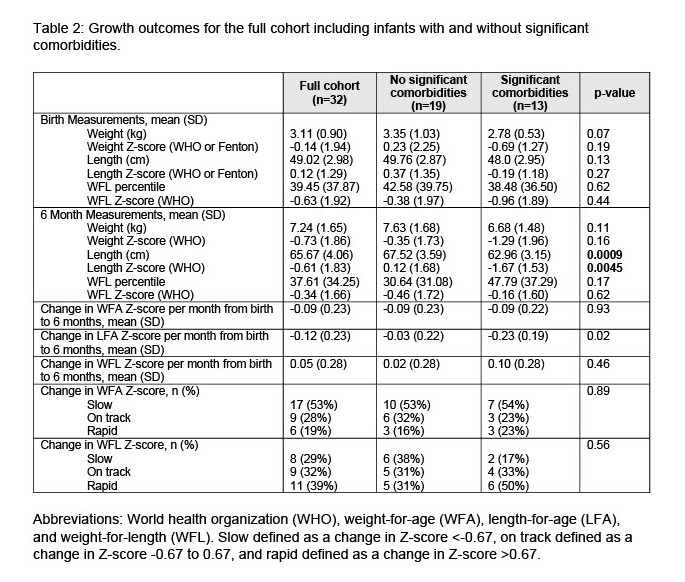 Abbreviations: World health organization (WHO), weight-for-age (WFA), length-for-age (LFA), and weight-for-length (WFL). Slow defined as a change in Z-score <-0.67, on track defined as a change in Z-score -0.67 to 0.67, and rapid defined as a change in Z-score >0.67.
Abbreviations: World health organization (WHO), weight-for-age (WFA), length-for-age (LFA), and weight-for-length (WFL). Slow defined as a change in Z-score <-0.67, on track defined as a change in Z-score -0.67 to 0.67, and rapid defined as a change in Z-score >0.67.Table 3: Growth outcomes for infants with no significant comorbidities.
.jpg) Abbreviations: World health organization (WHO), weight-for-age (WFA), length-for-age (LFA), and weight-for-length (WFL). Slow defined as a change in Z-score <-0.67, on track defined as a change in Z-score -0.67 to 0.67, and rapid defined as a change in Z-score >0.67.
Abbreviations: World health organization (WHO), weight-for-age (WFA), length-for-age (LFA), and weight-for-length (WFL). Slow defined as a change in Z-score <-0.67, on track defined as a change in Z-score -0.67 to 0.67, and rapid defined as a change in Z-score >0.67.Table 1: Neonatal hyperinsulinism cohort characteristics.
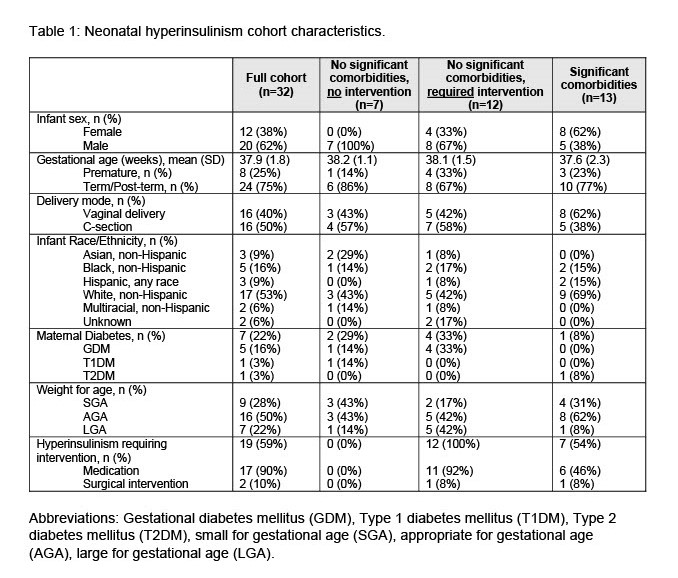 Abbreviations: Gestational diabetes mellitus (GDM), Type 1 diabetes mellitus (T1DM), Type 2 diabetes mellitus (T2DM), small for gestational age (SGA), appropriate for gestational age (AGA), large for gestational age (LGA).
Abbreviations: Gestational diabetes mellitus (GDM), Type 1 diabetes mellitus (T1DM), Type 2 diabetes mellitus (T2DM), small for gestational age (SGA), appropriate for gestational age (AGA), large for gestational age (LGA).Table 2: Growth outcomes for the full cohort including infants with and without significant comorbidities.
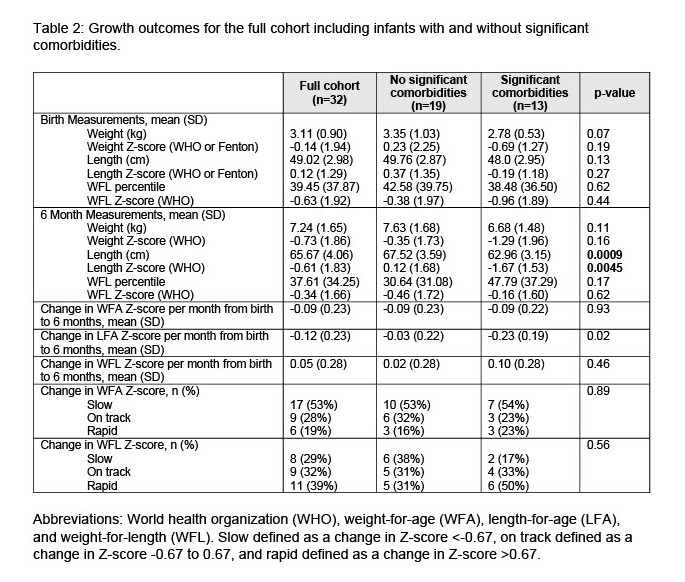 Abbreviations: World health organization (WHO), weight-for-age (WFA), length-for-age (LFA), and weight-for-length (WFL). Slow defined as a change in Z-score <-0.67, on track defined as a change in Z-score -0.67 to 0.67, and rapid defined as a change in Z-score >0.67.
Abbreviations: World health organization (WHO), weight-for-age (WFA), length-for-age (LFA), and weight-for-length (WFL). Slow defined as a change in Z-score <-0.67, on track defined as a change in Z-score -0.67 to 0.67, and rapid defined as a change in Z-score >0.67.Table 3: Growth outcomes for infants with no significant comorbidities.
.jpg) Abbreviations: World health organization (WHO), weight-for-age (WFA), length-for-age (LFA), and weight-for-length (WFL). Slow defined as a change in Z-score <-0.67, on track defined as a change in Z-score -0.67 to 0.67, and rapid defined as a change in Z-score >0.67.
Abbreviations: World health organization (WHO), weight-for-age (WFA), length-for-age (LFA), and weight-for-length (WFL). Slow defined as a change in Z-score <-0.67, on track defined as a change in Z-score -0.67 to 0.67, and rapid defined as a change in Z-score >0.67.
