Global Neonatal & Children's Health 3
Session: Global Neonatal & Children's Health 3
762 - Mothers' Voices: Attitudes Towards Providing and Accepting Donor Human Milk Among NICU Families in Ethiopia
Sunday, April 27, 2025
8:30am - 10:45am HST
Publication Number: 762.5685
Sharla Rent, Duke University School of Medicine, Durham, NC, United States; Merhawit Abadi, Saint Paul's Hospital Millennium Medical College, ADDIS ABABA, Adis Abeba, Ethiopia; Gregory C.. Valentine, University of Washington School of Medicine, Tacoma, WA, United States; Krystle M.. Perez, University of Washington, Seattle, WA, United States; Olivia C. Brandon, University of Washington: Magnuson Health Sciences Center – RR 544A, Seattle, WA, United States; Gal Barbut, Golisano Children's Hospital at The University of Rochester Medical Center, Rochester, NY, United States; Redeat Workneh, St Paul's Hospital Millennium Medical College, Addis Ababa, Ethiopia, Adis Abeba, Ethiopia; Mahlet Abayneh, St Paul's Hospital Millennium Medical College, Addis ABABA, Adis Abeba, Ethiopia

Sharla Rent, MD, MScGH (she/her/hers)
Assistant Professor of Pediatrics
Duke University School of Medicine
Durham, North Carolina, United States
Presenting Author(s)
Background: Ethiopia ranks in the top 10 countries for neonatal mortality. A low-cost intervention to prevent death and improve outcomes of small and/or sick newborns (SSNBs) is early and exclusive feeding with human milk. Provision of mother’s own milk (MOM) is preferred but not always possible (e.g. if mothers are ill or die during childbirth). Moreover, production of sufficient MOM for preterm newborns can take up to 2 weeks. While donor human milk (DHM) is used in high-income countries when deficiencies in MOM exist, only 7 out of 54 African countries have DHM programs – a significant health disparity.
Objective: We seek to describe the beliefs and preferences of Ethiopian mothers regarding breastfeeding and the use of DHM to nourish SSNBs. This study is part of a pre-implementation assessment for establishing a DHM program at St Paul’s Hospital Millennium Medical College (SPHMMC) in Ethiopia. Here, we focus on mothers of infants admitted to the Neonatal Intensive Care Unit (NICU) at SPHMMC.
Design/Methods: We performed a prospective, observational, cross-sectional study including mothers of newborns born at < 37 weeks gestation or < 2.5kg who were admitted to the SPHMMC NICU. We evaluated current breastfeeding practices, beliefs about DHM, and perceptions of nutritional content of MOM and DHM. Data was collected Jan-May 2024.
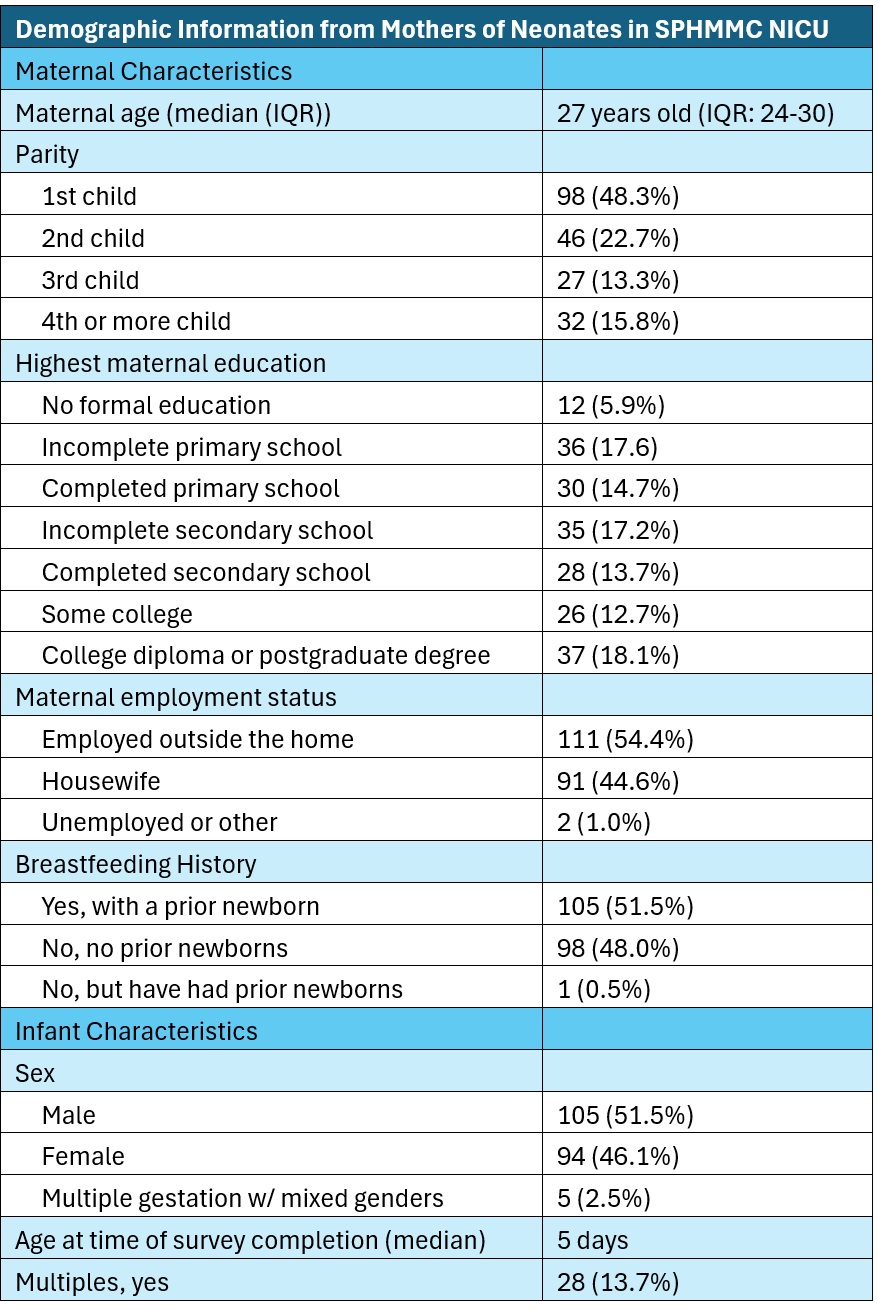
Results: 205 mothers completed the survey (Table 1); 46 (22.5%) had a “favorable” or “very favorable” view of using DHM if they did not have adequate MOM. Mothers preferred to supplement MOM with formula (98.0%), cow’s milk (47.3%), or unpasteurized milk from a relative (35.6%) as opposed to milk from a non-relative (11.7% unpasteurized, 25.4% pasteurized; Figure 1a). Formula was cited most often (99.5% of respondents) as having “good” or “very good” nutrition, followed by cow’s milk, IV fluids, and then MOM (Figure 1b). Safety was the primary concern by those unwilling to accept DHM (40% of subset, Figure 1c). 52 mothers (25.9%) reported having “excess expressed breastmilk”. Of those, 26 (50%) currently discard their excess milk. Most mothers would donate any excess expressed milk to both relatives and non-relatives (55.1%-61.5% across scenarios; Figure 2).
Conclusion(s): While >55% of mothers of infants admitted to the SPHMMC NICU were willing to donate their excess milk, the majority were hesitant to feed DHM to their SSNBs. Further work is needed to evaluate the socio-cultural and systems barriers and facilitators to establishing a DHM program in Ethiopia and to develop an educational intervention seeking to overcome these barriers.
Table 1: Demographic information from n=204 mothers with small and sick newborns in the SPHMMC NICU in Addis Ababa, Ethiopia
Maternal Perceptions of Donor Human Milk
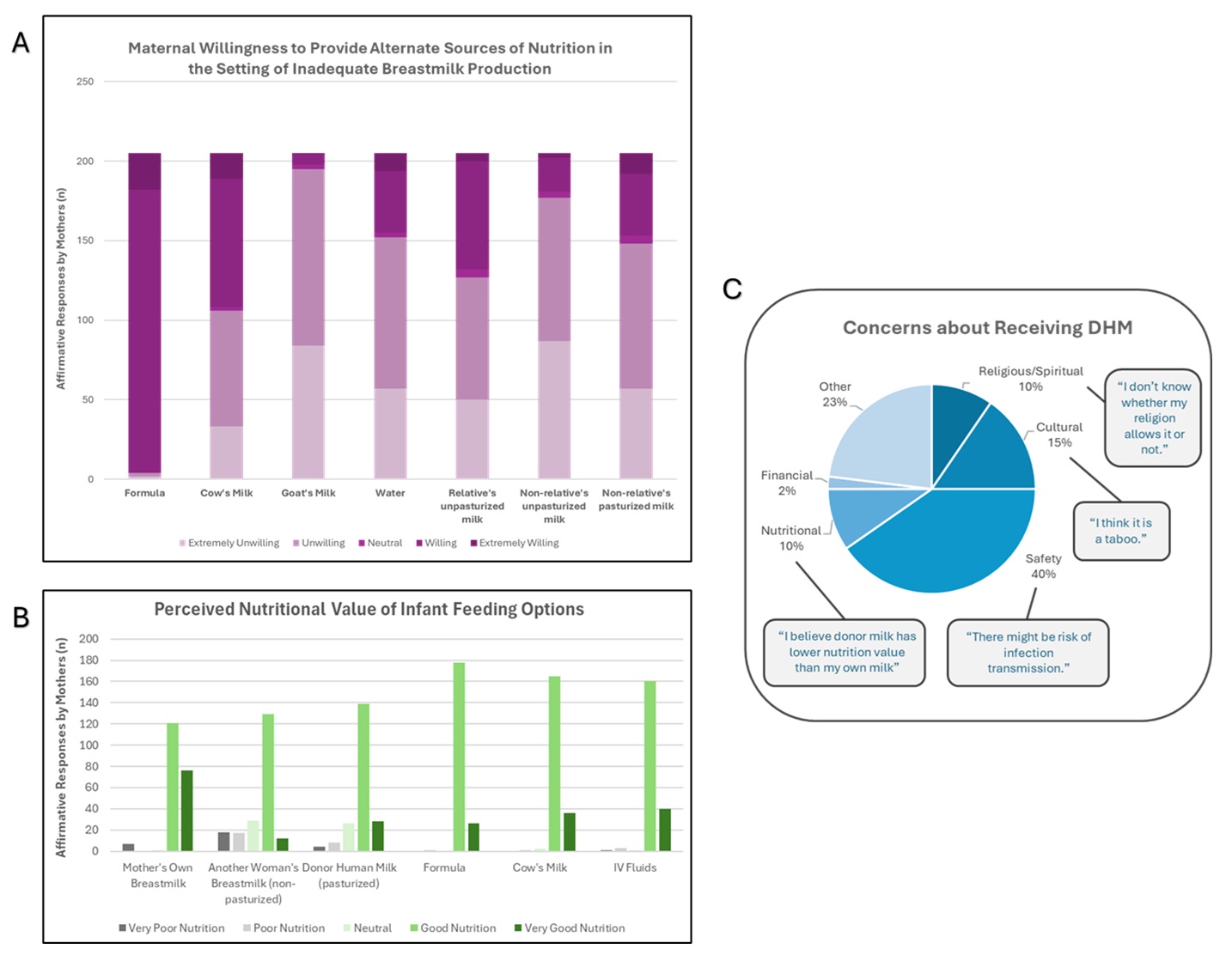 Figure 1: (A) Maternal preferences for providing nutrition if they have insufficient milk supply to feed their infant and (B) Perceived nutritional value of mother’s own milk and alternative feeding options by mothers of infants in an Ethiopian NICU. (C) Stated concerns and associated free-text responses about donor human milk from a subset of these mothers (n=52) who answered optional clarifying questions on donor milk use preferences.
Figure 1: (A) Maternal preferences for providing nutrition if they have insufficient milk supply to feed their infant and (B) Perceived nutritional value of mother’s own milk and alternative feeding options by mothers of infants in an Ethiopian NICU. (C) Stated concerns and associated free-text responses about donor human milk from a subset of these mothers (n=52) who answered optional clarifying questions on donor milk use preferences.Stated willingness of Ethiopian mothers to donate their milk to relatives and non-relatives
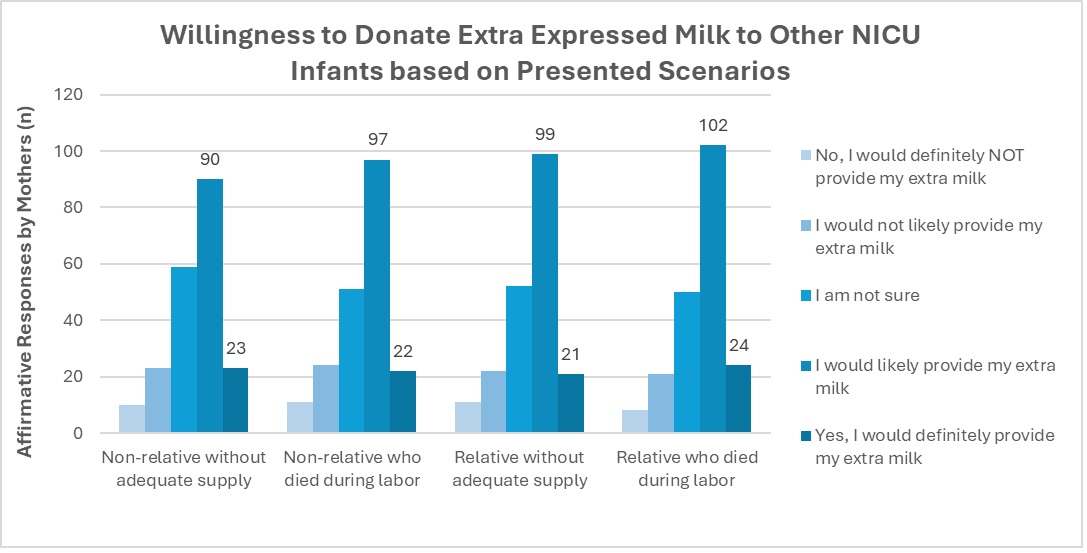 Figure 2: Stated willingness of Ethiopian mothers to donate their milk to relatives and non-relatives.
Figure 2: Stated willingness of Ethiopian mothers to donate their milk to relatives and non-relatives. 
