Gastroenterology/Hepatology
Session: Gastroenterology/Hepatology
330 - Management of pediatric patients admitted for colonic disimpaction: A scoping review
Sunday, April 27, 2025
8:30am - 10:45am HST
Publication Number: 330.5788
Zunaira Mahmood, University of Iowa Stead Family Children's Hospital, Iowa City, IA, United States; Hunter Fischer, University of Iowa Roy J. and Lucille A. Carver College of Medicine, Coralville, IA, United States; Dawn Ebach, University of Iowa Roy J. and Lucille A. Carver College of Medicine, Iowa City, IA, United States; Nathaniel A. Justice, University of Iowa Hospitals & Clinics, Iowa City, IA, United States; Alaina Berg, University of Iowa Stead Family Children's Hospital, Iowa City, IA, United States; Andrew Smelser, University of Iowa Stead Family Children's Hospital, Atlanta, GA, United States; Riley J. Samuelson, University of Iowa Libraries, Iowa City, IA, United States; Aamer Imdad, University of Iowa Roy J. and Lucille A. Carver College of Medicine, 200 Hawkins drive, IA, United States
- AI
Aamer Imdad, MBBS, MPH (he/him/his)
University of Iowa Stead Family Children's Hospital
Iowa City, Iowa, United States
Presenting Author(s)
Background: Pediatric functional constipation (FC) affects 9.5% of children globally. Fecal impaction is a severe progression of FC, involving dilated rectum filled with stool, diagnosed via physical exam (PE) or X-ray. While most cases are managed outpatient, inpatient care is required when outpatient management fail, imposing stress on young patients and financial burdens on families and healthcare. Despite research, no standardized inpatient protocol exists for colonic disimpaction. This review aims to summarize current literature on inpatient fecal disimpaction in pediatrics and identify knowledge gaps.
Objective: To map evidence on inpatient interventions for pediatric fecal impaction and identify knowledge gaps.
Design/Methods: We conducted a database search in February 2024 for studies on pediatric inpatient colon cleanout, including pharmacologic interventions via the upper or lower gastrointestinal (GI) tract or both. Outcomes assessed are shown in fig.1. Eligible studies included randomized and quasi-experimental, cohort studies, systematic reviews, and hospital protocols. Two reviewers screened titles and abstracts, extracted data using Covidence, with data graphically represented in Microsoft Excel and evidence maps created in EPPI reviewer.
Results: The search identified 8,690 titles, with 65 studies undergoing full-text review; 21 met inclusion criteria. Of these, 6 were U.S. hospital protocols and 15 research studies, primarily single-center: 3 randomized trials, 8 cohort studies, 1 quasi-experimental, 1 non-comparative, and 1 retrospective survey; 1 was multi-center. Sample sizes ranged from 8 to 14,243, spanning 7 countries: U.S., India, U.K., Chile, Philippines, South Africa, and South Korea. Definitions of severe constipation varied (Fig.2).
For cleanout success, 3 studies used stool consistency, while others used imaging, PE, symptom resolution, stool count, and therapy discontinuation. Polyethylene glycol (PEG) via upper GI was most common, followed by enemas (fig.3). Among 11 studies using PEG, 4 used nasogastric (NG) tubes, 2 used NG tubes as needed, 2 used oral PEG without NG, and 3 were unclear. IV fluids were used in 12 of 15 studies. Cleanout success definitions varied by stool consistency, imaging, PE, symptom resolution, and therapy discontinuation.
Conclusion(s): Significant variability exists in definitions of fecal impaction, cleanout success, and treatment methods. Optimal inpatient disimpaction methods for efficacy and safety remain undetermined. This review highlights the need for further studies to establish effective strategies for inpatient pediatric fecal impaction management.
Figure 1
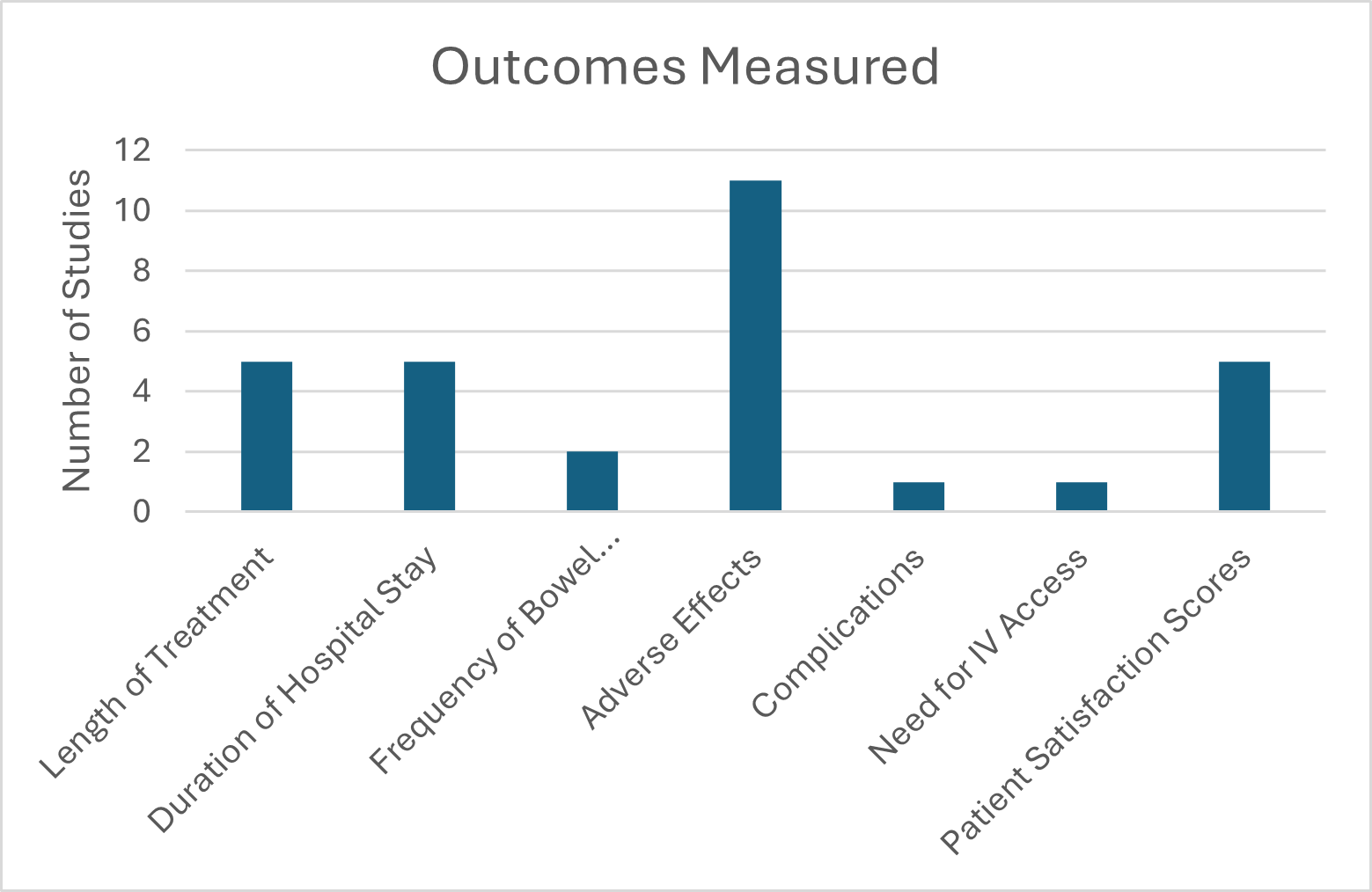 Outcomes measured during study.
Outcomes measured during study. Figure 2
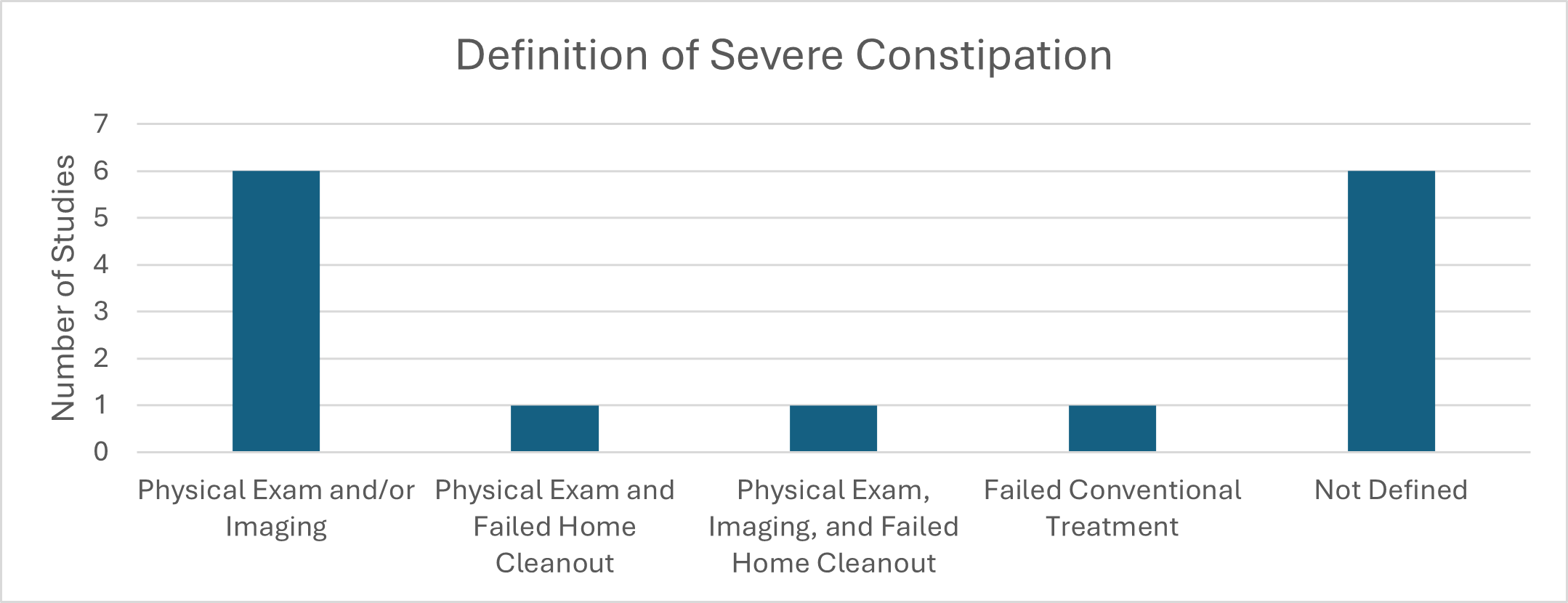 Definition of severe constipation based on included studies.
Definition of severe constipation based on included studies.Figure 3
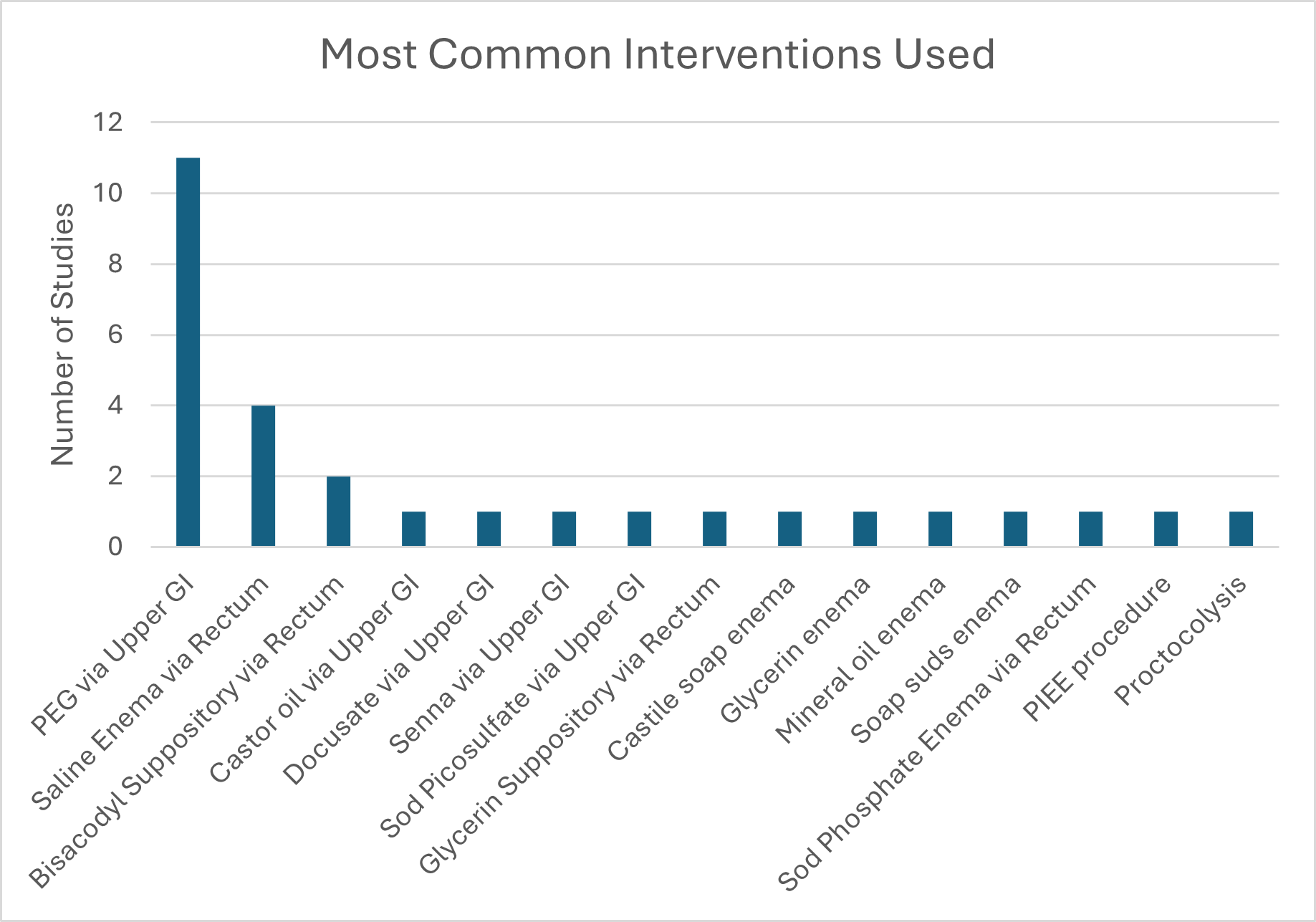 Most common interventions used in the studies for colon cleanout
Most common interventions used in the studies for colon cleanout
